ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 22
A comparative study: transecting versus avoiding incision of the anterior placenta previa
1Department of Obstetrics and Gynecology, Guangzhou Women and Children’s Medical Center, Guangzhou Medical Center, Guangzhou Medical University, Guangzhou, Guangdong, PR China
2Department of Hematology, the Third Affiliated Hospital, Sun Yat-Sen University, Guangzhou, Guangdong, PR China
- *Corresponding Author:
- Huishu Liu
Department of Obstetrics and Gynecology
Guangzhou Women and Children’s Medical Center
Guangzhou Medical Center
Guangzhou Medical University, PR China
Accepted date: October 13, 2017
Objective: To evaluate the method of avoiding incision of the placenta using partial separation of the anterior placenta previa during cesarean delivery and to compare the outcomes between this method and the conventional method involving transection of the placenta.
Patients and Methods: In this retrospective study, subjects were categorised into two groups: 32 patients underwent placental transection to rupture the membranes (transection group), and 22 patients underwent deliver partial separation of the placenta for membrane rupture (non-transection group). Maternal and fetal outcomes, including the operative time, volume of blood loss, maternal transfusion of packed red blood cells, Apgar score, new-born hemoglobin, and blood gas analysis, were compared.
Results: The surgical blood loss was significantly lower in the non-transection group (P<0.05). There were no significant differences in operation time and incision to delivery time (P>0.05) between the two groups. Neonatal blood gas analysis show that the pH and Base Excess (BE) values were significantly decreased (P<0.05) while the blood lactic acid was significantly increased (P<0.05) in the transection group compared to the non-transection group. The Apgar scores at 1 min and new-born hemoglobin levels did not significantly differ between in the groups (P>0.05).
Conclusions: Avoiding incision of the anterior placenta previa may help reduce the risk of intrapartum hemorrhage and neonatal acidosis.
Keywords
Placenta previa, Cesarean delivery, Placental position, Intrapartum hemorrhage, Blood loss.
Introduction
Placenta previa is a potentially life-threatening condition for both mother and infant. It is an inequivocal indication for cesarean section, but nonetheless can be a challenging delivery to complete safely. One study reported the incidence of placenta previa to be approximately 0.4% [1]. The incidence of excessive blood loss, massive transfusion, hysterectomy, and fetal anemia has been reported to be higher when the placenta is anteriorly located than when it is posteriorly located [2,3]. Limited data are available regarding the preferred delivery method among women with anterior placenta previa.
We employed procedure for cesarean section developed from the method described by Ward et al. [4]. This method of avoiding incision of the placenta to rupture the membranes can avoid transecting the placenta, and may help to reduce the risk of maternal and fetal hemorrhage.
In this retrospective study, we compared the maternal and fetal outcomes of transection of the placenta and partial separation of the placenta to rupture the membranes in order to investigate the presumed advantages of the Ward method.
Materials and Methods
Patients
Data of women with anterior placenta previa who underwent cesarean section at the Guangzhou Women and Children’s Medical Center from June 2011 to July 2013 were extracted and used for the present study. The inclusion criteria were as follows: women had anterior placenta previa diagnosed by ultrasound and the placenta covered >50% of the anterior uterine wall, and singleton pregnancies. Patients with placenta accreta were excluded (one patient was diagnosed with placenta accreta during delivery by cesarean section) from the study. A total of 32 patients were treated with traditional transection of the placenta to rupture the membranes during cesarean delivery (transection group), while 22 patients were treated by partial separation of the placenta, avoiding incision of the placenta, to rupture the membranes and deliver the infant (non-transection group). Table 1 shows the demographic and clinical characteristics of the two groups. The operative time, fetal labor time, Estimated Blood Loss (EBL), Apgar score, new-born hemoglobin level, and blood gas analysis were all obtained from the patient records.
| Groups (n) | Non-transection (22) | Transection (32) | p |
|---|---|---|---|
| Maternal age (y) | 31 ± 4 | 30 ± 2 | 0.14 |
| Gravidity | 2 ± 1 | 3 ± 1 | 0.14 |
| Parity | 1.2 ± 1 | 1.1 ± 1 | 0.36 |
| Gestational age at delivery (w) | 36.1 ± 1.4 | 36.3 ± 1.2 | 0.29 |
| Birth weight (g) | 2610 ± 450 | 2720 ± 330 | 0.15 |
Table 1: Demographic and clinical characteristics.
The study protocol was approved by the Research Ethics Committee of Guangzhou Women and Children’s Medical Center and all patients gave their informed consent before study commencement.
Preoperative assessment
Before C/S, ultrasound was used to locate the position of the placenta, including placental boundary (relationship between boundary and pubic symphysis, navel, and other identification landmarks), placental thickness, umbilical cord insertion site, fetal position, and whether or not placenta accreta was present.
Operative methods
Non-transection method: Before incision, the location and margin of the placenta are estimated. An incision site is selected in the lower uterine segment, avoiding the area of vascular ectasia, and a 2 to 3 cm incision is then made in the anterior wall of the uterus until placental tissue is encountered. The placenta is lifted. For lifting of the placenta, the position of the placenta is evaluated before the operation and the distance between the placenta and the uterine incision is estimated. This can guide the surgeon to lift or separate the placenta. This procedure is accomplished by placing the right hand down along the placenta edge nearest to the uterine incision to lift the placenta. After perceiving the external and upper edges of the placental edge, the membranes are ruptured. The operating assistant then pushes the uterine fundus to distend the fetal membranes and membranes are ruptured. The operator lifts and separates the placenta from the uterus, avoiding incision of the placenta until the membranes can be palpated beyond the placental edge, after membrane rupture and blunt dissection of the myometrium. The placenta is then moved aside and the neonate is delivered. After the neonate is delivered, approximately 25-30 cm of the umbilical cord is milked towards the neonate before omphalotomy.
Transection method: A routine incision is made in the lower uterine segment, followed by blunt dissection of the myometrium, and rapid transection of the placenta to rupture the membranes and deliver the neonate.
Statistical analysis
Statistical analysis was performed using SPSS10.0 software (need manufacturer and location here). Continuous variables were compared using independent t test and Mann-Whitney U test for normal and non-normal variables, respectively. A p value of <0.05 was considered to be statistically significant.
Results
The maternal age, gravidity, parity, gestational age, and neonatal birth weight did not significantly differ between the transection and non-transection groups.
There were no significant differences in the operative time and incision to delivery time between the transection and nontransection groups EBL was statistically significantly lower in the non-transection group than in the transection group The cases with EBL more than 1000 ml, need for blood transfusion and hospitalization days were statistically significantly less in the non-transection group than those in the transection group.
The Apgar scores at 1 min and asphyxia rate did not significantly differ between the two groups in the nontransection and transection groups, respectively. The hemoglobin level of the neonates did not significantly vary between the two groups. Neonatal blood gas analysis showed that the pH and BE were significantly decreased, while the blood lactic acid was significantly increased in the transection group, there was no significant difference in the incidence of severe neonatal anemia between the two groups (Tables 2 and 3).
| Groups (n) | Non-transection (22) | Transection (32) | p |
|---|---|---|---|
| Operation time (min) | 35 ± 15 | 39 ± 12 | 0.14 |
| Incision to delivery time (min) | 4 ± 3 | 5 ± 2 | 0.09 |
| Intraoperative blood loss (ml) | 425 ± 123 | 514 ± 104 | 0.006 |
| Cases with EBL>1000 ml | 2 | 11 | 0.001 |
| Need for blood transfusion | 3 | 13 | 0.039 |
| Hospitalization days (d) | 3 ± 2 | 5 ± 3 | 0.009 |
Table 2: Maternal morbidity.
| Groups (n) | Non-transection (22) | Transection (32) | p |
|---|---|---|---|
| Apgar score at 1 min | 9.1 ± 0.3 | 9 ± 0.5 | 0.18 |
| Apgar score<7 at 5 min | 1 | 5 | 0.4 |
| Hemoglobin at birth, g/L | 150 ± 34 | 142 ± 36 | 0.21 |
| pH at birth | 7.3 ± 0.10 | 7.1 ± 0.3 | < 0.001 |
| Base excess at birth (mmol/l) | -5.4 ± 4.8 | -7.5 ± 2.1 | 0.03 |
| Blood lactic acid (mmol/l) | 1.5 ± 0.5 | 3.8 ± 1.3 | <0.001 |
| Neonatal anemia (Hb<60 g/l) | 1 | 4 | 0.607 |
Table 3: Neonatal morbidity.
Discussion
Placenta previa is an important cause of intrapartum hemorrhage. Many studies have indicated that patients with placentas attached to the posterior wall of the uterus have less bleeding than women whose placentas are attached to the anterior wall [3,5,6]. Cesarean section is the usual route of delivery for these patients. The optimal method of cesarean delivery for patients with anterior placenta previa has not yet been established and it must be better evaluated to reduce maternal blood loss and avoid harm to the baby.
In recent years, several studies have focused on the choice of the uterine incision used to circumvent the placenta in cases of anterior placenta previa [4,7,8]. Uterine incision of anterior placenta previa can be divided into two types: one in which the incision is made through the placenta and the other, where the uterine incision avoids the placenta. Incisions used to avoid the placenta include vertical, along the placental edge, and such as T- or J-shaped cuts [8]. All these incisions extend to body of the uterus. Vertical incisions may damage the bladder and increase the risk of subsequent uterine rupture. [9]. If the placenta is too large, covering the entire front wall of the uterus, these incisions may not be effective. If the incision is too high, and located far from the placental separation of the lower uterine segment, it is difficult to control postpartum bleeding because of the narrow view of the central pelvis. Some methods have used a T-shaped uterine incision or added a transverse incision in the lower segment (after suturing the initial uterine incision, through which infant has been delivered, a transvers incision is made in the lower uterine segment). While this procedure facilitates easy viewing of the placenta dissection, it may lead to more problems for the mother and fetus, for example, it may increase the risk fetal anemia a higher risk of uterine rupture in subsequent pregnancies [10]. In 2003, Ward proposed deliberate partial separation of the placenta to rupture the membranes and deliver the infant, without transection of the placenta [4]. Our study further developed and assessed the usefulness of this method.
The traditional Pfannenstiel technique requires a surgical incision of 12-13 cm in length that allows access to the abdomen. If surgeons are unable to avoid the placenta in case of anteriorly placed placentas, they transect the placenta, extending the incision to both sides of the placenta, thereby releasing amniotic fluid for delivery [11,12]. This method is done blind. The amount of bleeding may differ depending on the position of incision on the placenta. For example, blood loss may be higher if the central part of the placenta or the part to which the umbilical cord is attached is incised, as this would lead to rupture of blood vessels during the operation.
Compared with the traditional Pfannenstiel incision technique, the Ward procedure appears to be an improved approach which is involved lifting the placenta instead of making an incision in it. This method does not harm the placental cotyledons, retains placental integrity for longer, and helps reduce hemorrhage at separating the placenta. It also may provide the surgeon with a better view, contributing to a successful delivery. Furthermore, this method may help to reduce the time between uterine incisions to rupture membranes, which may reduce the risk of blood loss in the new-born. In this study, the amount of bleeding during delivery was significantly lower in the nontransection group than in the transection group. In this study, there was no significant difference in neonatal anemia in the transection and non-transection groups. This is probably because the method of receiving umbilical cord blood after delivery may lead to transfusion of some cord blood to the new-born. However, the pH and base excess were significantly reduced in the transection group. We also noted that the serum lactic acid was significantly increased in the transection group compared to non-transection group. One study has shown that the umbilical artery blood lactate levels are closely related to the prognosis of high-risk infants at delivery [13]. This illustrates that the non-transection method of rupturing membranes may better prevent neonatal acidosis and may be associated with a better neonatal prognosis compared to the transection method.
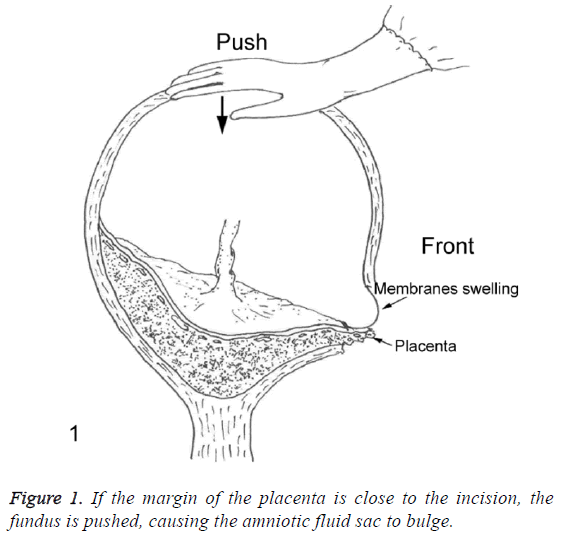
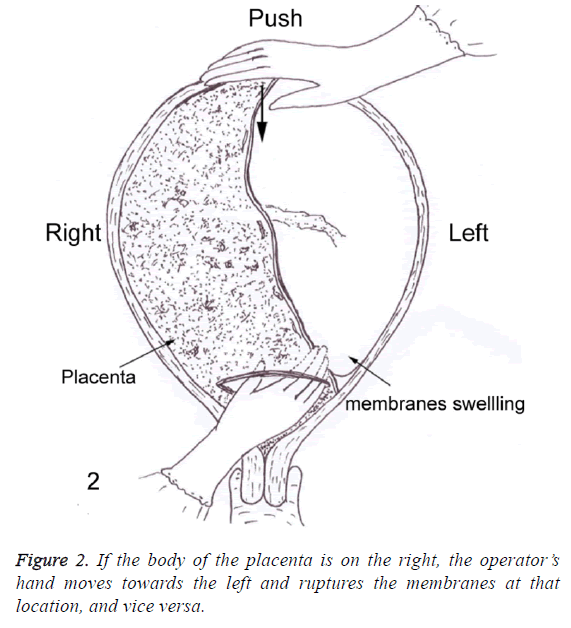
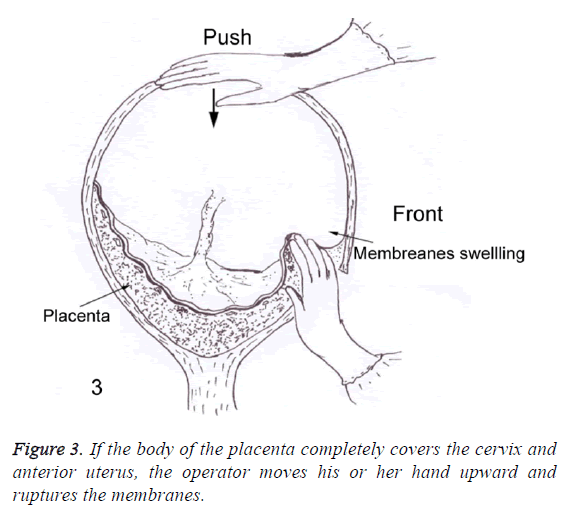
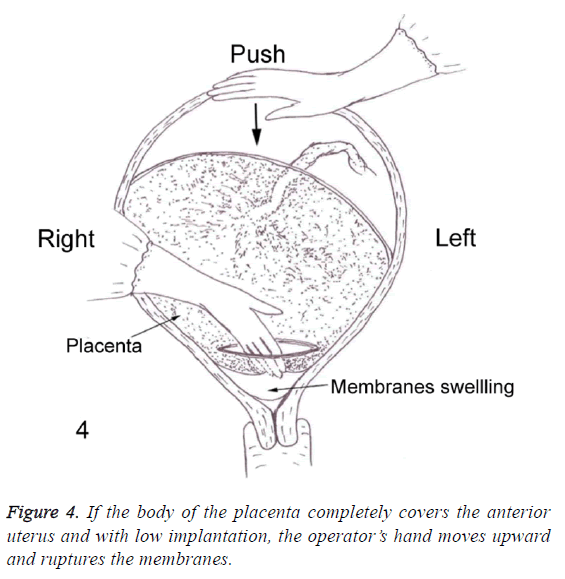
In 2003, Ward reported the results from three patients in a study in which he described a technique by which transection of the placenta could be avoided by passing a hand around the margin of the placenta [4]. In our study, we performed a similar but more flexible method of rupturing membranes. If the margin of the placenta was close to the incision, the fundus is pushed, causing the amniotic fluid sac to bulge (Figure 1). If the body of the placenta is on the right, the operator moves his or her hand towards the left and ruptures the membranes, and vice versa (Figure 2). If the body of the placenta completely covers the cervix and anterior uterus, the operator’s moves upward and ruptures the membranes (Figure 3). If the body of placenta completely covers the anterior uterus and with low implantation, the operator’s hand moves downward and ruptures membranes (Figure 4).
By following the guidelines described above, the integrity of the placenta can be maintained. A method of sharp dissection should be adopted to make a 2-3 cm incision (if the body of placenta is on the right, the incision can be moved to the left, and vice versa) to arrive at the interface between the uterus and placenta. The uterine wall is then bluntly dissected to moderate width with a forefinger. Assistants should push the uterus from the fundus to move the placenta upward and cause the membranes to bulge or extend outward. The resultant increase in tension in the membranes will make it easier to rupture them.
There are some limitations to this method: The method of lifting the placenta requires some practice, but the procedure is simple and it is easy to train obstetricians. Situations in which the placenta is considerably distant from the incision of the lower uterus can lead to difficulties in childbirth.
At times, transection of the placenta is unavoidable by any method in placenta previa with broad involvement of the anterior uterine wall.
Conclusion
In conclusion, the method we developed and describe in this present study appears to help reduce the risk of intrapartum hemorrhage and may reduce neonatal morbidity. This approach could be selected for treating anterior placenta previa in clinical practice.
Limitations to this Study
You need to include these one is small sample size with potential beta-error. Another is retrospective, non-randomized design.
Conflicts of Interest
We declare that we have no conflict of interest.
Ethical Approval
This study was retrospective in nature, therefore for this type of study formal consent is not required.
References
- Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med 2003; 13: 175-190.
- Bahar A, Abusham A, Eskandar M, Sobande A, Alsunaidi M. Risk factors and pregnancy outcome in different types of placenta previa. J Obstetr Gynaecol Canada 2009; 31: 126-131.
- Jang DG, We JS, Shin JU, Choi YJ, Ko HS, Park IY. Maternal outcomes according to placental position in placental previa. Int J Med Sci 2011; 8: 439-444.
- Ward CR. Avoiding an incision through the anterior previa at cesarean delivery. Obstet Gynecol 2003; 102: 552-554.
- Baba Y, Matsubara S, Ohkuchi A, Usui R, Kuwata T. Anterior placentation as a risk factor for massive hemorrhage during cesarean section in patients with placenta previa. J Obstet Gynaecol Res 2014; 40: 1243-1248.
- Sekiguchi A, Nakai A, Kawabata I, Hayashi M, Takeshita T. Type and location of placenta previa affect preterm delivery risk related to antepartum hemorrhage. Int J Med Sci 2013; 10: 1683-1688.
- Kotsuji F, Nishijima K, Kurokawa T, Yoshida Y, Sekiya T, Banzai M. Transverse uterine fundal incision for placenta praevia with accreta, involving the entire anterior uterine wall: a case series. Int J Obstetr Gynaecol 2013; 120: 1144-1149.
- Zou L, Zhong S, Zhao Y, Zhu J, Chen L. Evaluation of J-shaped uterine incision during caesarean section in patients with placenta previa: a retrospective study. J Huazhong Univ Sci Technol Med Sci 2010; 30: 212-216.
- Kayem G, Raiffort C, Legardeur H, Gavard L, Mandelbrot L, Girard G. Specific particularities of uterine scars and their impact on the risk of uterine rupture in case of trial of labor. J de Gynecologie Obstetrique et Biologie de la Reprod 2012; 41: 753-71.
- Nishida R, Yamada T, Akaishi R, Kojima T, Ishikawa S, Takeda M. Usefulness of transverse fundal incision method of cesarean section for women with placentas widely covering the entire anterior uterine wall. J Obstetr Gynaecol Res 2013; 39: 91-95.
- Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 2006; 107: 927-941.
- Palacios-Jaraquemada JM. Caesarean section in cases of placenta praevia and accreta. Best Pract Res Clin Obstetr Gynaecol 2013; 27: 221-232.
- Surmiak P, Baumert M, Fiala M, Sypniewska K, Walencka Z, Lukomska A. Umbilical cord blood NGAL concentration as an early marker of perinatal asphyxia in neonates. Ginekologia Polska 2014; 85: 424-427.