ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2010) Volume 21, Issue 3
A giant intra-abdominal testicular seminoma
Department of Surgery, College of Medicine, King Khalid University, Abha, Saudi Arabia.
- *Corresponding Author:
- Mishari H. Alshyarba
Department of Surgery
College of Medicine
King Khalid University
PO Box 641, Abha 61421
Saudi Arabia
Accepted Date: March 11 2010
A case is presented of a 40 year old fertile man with a history of unilateral cryptorchidism who presented with a lower abdominal mass. On investigations a giant intraabdominal seminoma was diagnosed. Laparotomy and complete excision was carried out. The possible association between the undescended testis and cancer transformations is briefly discussed
Keywords
Undescended testis, seminoma, cryptorchidism
Introduction
Cryptorchidism (testicular maldescent), the most common congenital anomaly of the genitourinary tract in males, is encountered in 1% of boys. The incidence increases in subjects with deficiencies of androgen function.1Such an organ is at high risk of torsion, trauma, infertility, and malignancy. A giant seminoma of an intra-abdominal testis in a fertile patient is reported in this case.
Case report
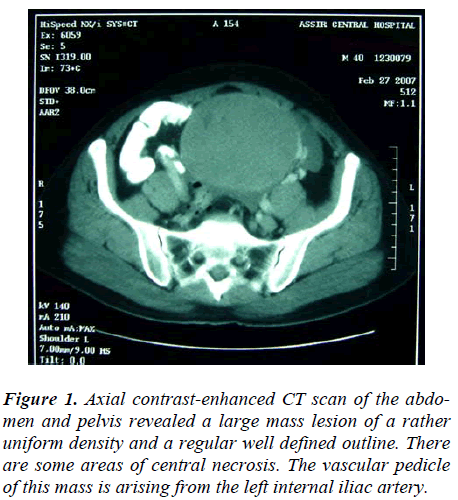
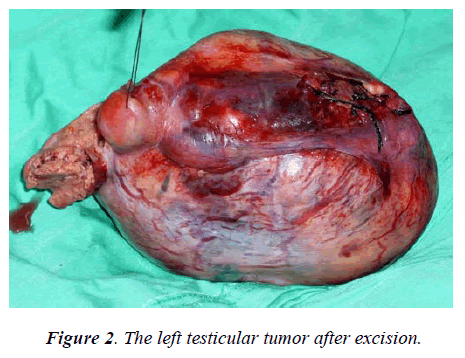
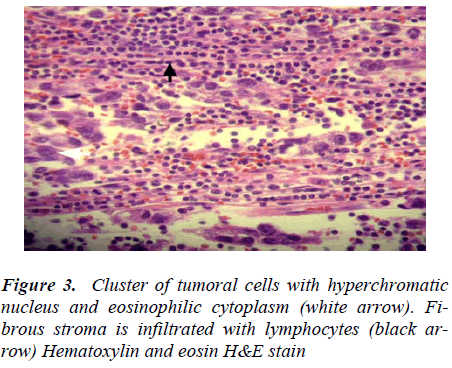
A 40-year-old patient, fathering seven siblings, presented to our hospital and was complaining of lower abdominal mass and discomfort for one year. No history of weight Scrotal examinations revealed a normal right testis; whereas, left testis was neither palpable in the scrotum nor in the inguinal region. The laboratory investigations were all normal; apart from a slightly elevated serum beta- human chorionic gonadotropin (β-HCG) 296 mmol/ L. The serum alpha- fetoprotein (α-FP) was within normal limits. The abdominal computed tomography (CT) scan revealed an 18x9x10cm solid mass with central necrosis extending from root of mesentery of transverse colon down to the pelvis. No paraortic lymphadenopathy (Figure 1). No other significant findings. Based on the age of the patient, clinically non-palpable left testis, the abdominal mass and the elevated β-HCG tumor of the intraabdominal testis was, therefore, suspected. Seminoma was the most probable diagnosis. Laparotomy was done through lower midline incision and total excision of the tumour was carried out. The tumour weight was approximately one kilogram (920 grams) (Figure 2). Postoperative course was uneventful. The histopathological examination of the excised tumour confirmed the diagnosis of pure classic seminoma (figure3). Patient was discharged home in good condition after 23 days from admission. After recovery patient received a prophylactic radiotherapy to the retroperitonium by oncologist after six weeks from discharge. At three months from surgery, α-FP was normal (37ng/ml) and β-HCG returned to normal value (12mIU/ml).There was no clinical evidence of local recurrence or distant metastasis after 18-months follow up after discharge.
Discussion
One of every 500 men has an undescended testis that may be associated with complications such as cancer, ischemia, and infertility. The cancer risk of an ectopic testis is 40 times higher than in a normal testis, and an abdominal testis is four times more likely to undergo malignant degeneration than an inguinal testis.2 The cancer of undescended testes peaks in the third or fourth decade of life.3 Seminoma is a germ cell neoplasm of the testis. Pure seminoma is the most frequent cancer in the undescended testis.4 For this reason, testicular cancer should be considered in the differential diagnosis of a retroperitoneal mass in a patient with a non-palpable testis.
Two hypotheses have been proposed to explain this association. The first, posits that local temperature elevation of an ectopic testis is, somehow, procarcinogenic. If this hypothesis is correct, then orchidopexy (testis descend and fixation in the scrotum) could protect against cancer; if the procedure is performed before precancerous cells differentiate to a critical point such as could occur in puberty. The second hypothesis, posits that an underlying hormonal condition predisposes to both cryptorchidism and testicular cancer. If so, orchidopexy would not prevent testicular cancer; and orchidectomy would be required. The surgical treatment of cryptorchidism to prevent testicular cancer remains unclear. The early age of orchidopexy is ascertained in substantially reducing the risk of testicular tumour development. The timing of orchidopexy, however, was a field of debates and discussions among authors. Lisa J et al observed, in their casecontrolled study with good number in the series, no increased risk of testicular cancer among men whose cryptorchidism had been successfully resolved by their 11th birthday; but a 32-fold increased risk among men whose cryptorchidism persisted after this age.5 They estimate of a 4.8 fold increased risk of testicular cancer among men with a history of cryptorchidism which is consistent with numerous earlier reports.
Though this patient was fertile, the association of male sub-fertility and testicular cancer has been studied recently. It has been hypothesized that both testicular cancer and male sub-fertility may be caused by exposure of the developing male embryo to agents that disrupt normal hormonal balance. This in-utro hormonal imbalance can explain the risk of testicular cancer in a normal descended testis. Henrik Møller et al in, a large population-based case-control study, found that men who had fathered a child or who had impregnated a woman had a significantly decreased subsequent risk of testicular cancer.6 The reduction in risk seemed to increase with each successive child. Men with low relative fertility had double the risk of testicular cancer compared with men with the expected number of children for their age. When they analyzed the results separately they found them to be similar for the two main histological types of testicular cancer: seminoma and non-seminoma.
The issue of a routine biopsy of the contra-lateral testis, in patients with newly diagnosed unilateral testicular cancer, is a matter of ongoing discussions. Sophie D et al evaluated the risk of contra-lateral testicular cancer and survival in a large population-based cohort study of men diagnosed with testicular cancer before age 55 years. The 15-year cumulative risk of developing a metachronous contra-lateral testicular cancer was only 1.9%.7 They found also men who were younger than 30 years at diagnosis with a seminomatous unilateral testicular cancer had the highest 15-year cumulative risk of developing metachronous contra-lateral testicular cancer 3.1%; whereas men who were 30 years or older at diagnosis with a nonseminomatous unilateral testicular cancer had the lowest 15-year cumulative risk of developing metachronous contra- lateral testicular cancer 1.2%. So, they concluded that the need to perform a routine biopsy of the contra-lateral testis in patients with newly diagnosed unilateral testicular cancer is not recommended because of the low overall cumulative risk (<2%). Some European investigators, however, advice that all testicular cancer patients to have a biopsy of the contra-lateral testis, followed by treatment of any carcinoma in situ.8 So with these conflicting opinions; for high-risk patients for metachronous testicular cancer, especially those with a history of testicular maldescent, infertility, or testicular atrophy or a family history of testicular cancer and younger age at diagnosis of testicular cancer a testicular biopsy followed by individual counseling and or treatment of carcinoma in situ may be justified. The clinician should inform the patient that the overall cumulative risk of metachronous testicular cancer is ranging from 2%-5% in most studies. It is, therefore, for the patient to decide whether to have biopsy and or treatment for the detected contra-lateral testicular carcinoma in situ. For the none-high risk patients, it is, however, recommended that clinicians should encourage all unilateral testicular cancer patients to perform regular testicular self-examination (TSE) and undergo regular testicular ultrasonography. The patient was, in fact, counseled for contra-lateral testicular biopsy but preferred to do (TSE) and to have a close surveillance. The aim of this approach, is to detect a nonmetastatic metachronous contralateral testicular cancer while the primary tumor is still small enough to perform testis-sparing surgery. Thus, avoid problems associated with androgen substitution after bilateral orchidectomy and reduce the risk of delayed presentations with the complications that have an inverse impact on patient's life and overall health expenses.
In conclusion, early diagnosis and treatment of cryptorchidism can dramatically reduce the risk of testicular cancer and probably preserve the fertility, as well as, the virility of the patient.
References
- Kiely EA. Scientific basis of testicular descent and management implications for cryptorchidism. Br J Clin Pract 1994; 48: 37-41.
- Fonkalsrud EW. Current management of undescended testis. Semin Pediatr Surg. 1996; 5: 2-7.
- Rao AB. Seminoma in undescended testes. Br J Urol. 1969; 41: 83-88.
- Batata MA, Whinore WF Jr, Chu FCH, et al. Cryptorchidism and testicular cancer. J Urol. 1980; 124: 382-387.
- Lisa J. Herrinton, Wei Zhao, Gail Husson: Management of Cryptorchidism and Risk of Testicular Cancer. Am J Epidemiol 2003; 157:602- 605.
- Henrik Møller, Niels E Skakkebæk. Risk of testicular cancer in sub-fertile men:case-control study. BMJ 1999; 318: 559-562.
- Sophie D. Fosså , Jinbo Chen , Sara J. Schonfeld et al. Risk of Contralateral Testicular Cancer: A Population based Study of 29 515 U.S. Men. J Natl Cancer Inst 2005; 97: 1056-1066.
- Daugaard G, Giwercman A, Skakkebæk NE. Should the other testis be biopsied? Semin Urol Oncol 1996; 14: 8-12.