ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2019) Volume 30, Issue 6
An intervention study on utilization of cauliflower leaf powder (CLP) on the nutritional status of selected rural school children of Kumarganj, Ayodhya, Uttar Pradesh, India
1Department of Food Science and Nutrition, College of Home Science, Narendra Deva University of Agriculture and Technology, Kumarganj, Ayodhya, India
2Department of Agriculture, Biochemistry, College of Agriculture, Narendra Deva University of Agriculture and Technology, Kumarganj, Ayodhya, India
- *Corresponding Author:
- Manju Lata Mishra
Department of Food Science and Nutrition
Narendra Deva University of Agriculture and Technology
Ayodhya,India
Accepted Date: September 22, 2019
In our country, micronutrient deficiency is growing very rapidly and affects all category of the population. Cauliflower leaves are normally redundant and contain high nutritional value. But due to unawareness, ignorance and socio-economic factor influenced its use to treat various micronutrient deficiencies. So it can be exploited at domestic level by incorporating in powder form (most acceptable percentage) and prepared products i.e. Fara, Dhokla and Laddoo were given. These supplements were given along with their daily diet. After feeding trials, blood samples were again collected and analyzed for hemoglobin level. Anthropometric measurements were also taken before and after intervention. When compared the weight (kg) of boys and girls before and after intervention, it was found that average% weight gain were 13.45 and 14.66 respectively. Whereas, when compared the average% gain in height (cm) of boys and girls before and after intervention, were 2.11 and 1.26, correspondingly. It was found that% Increase in Haemoglobin of boys of age 10 year+ and Age 11 year+ was 20.12 and 12.83 respectively. Whereas% Increase in Haemoglobin of girls of age 10 year+ and Age 11 year+ were 8.33 and 13.75 respectively. Hence, cauliflower leaves powder (CLP) could be utilized to progress the nutritional status of the people.
Keywords
Anthropometric, Cauliflower Leaf Powder (CLP), Hemoglobin, Supplements, Nutritional Status.
Introduction
As India is the second largest producer of vegetables in the world, but still Indian diet are poor in micronutrient rich food and causes so many serious disorders and diseases prevalent. United States, France, Italy, India and China are that country that produces significant magnitude of cauliflower in their places [1]. Cauliflower (Brassica oleraceae var. Botrytis) belongs to the Brassicaceae family and is the most commonly and frequently used vegetable in our day to day life. Although only half of the cauliflower is used for culinary preparation, rich in nutrients like proteins of high quality and vitamin C which is stable even after cooking and the remaining part i.e. leaves of the cauliflower is discarded at higher level and contributes high wastages. These plants based phytochemical can be used as majorly food source due to its deviating nutritional, functional, antioxidant and other therapeutic properties and adds nutritional security as well. There is no significance value given to the discarded leaves of cauliflower which is also rich source of dietary fibre, minerals, beta carotene, iron and calcium. The cauliflower leaves powder (CLP) could be used to treat anemia or iron deficiency or other micronutrient deficiencies [2]. The green leaves of cauliflower were dried and reported as highly nutritious and a good source of beta carotene as 43.11 mg, Iron as 60.38 mg, Copper as 1.55 mg, Manganese as 5.86 mg and Zinc contained 5.10 mg per 100g of CLP [3]. The leaves could be dried by home based technique which is easy and convenient to keep in airtight container for future use [4]. The premix of leaves powder of beet root, carrot, cauliflower and turnip were in the ratio of 1:2:1:1 and found 10% level of these leaf mixtures were best for sensory attributes [5]. Singh et al. also reported that the mortality rate can be reduced by 25-30 percent in malnourished children by incorporating dehydrated cauliflower leaves for development of various recipes can help to reduce the incidence of iron and vitamin A deficiency [6].
In today’s scenario, most of the children are stunting greatly which is an indicator of long duration malnutrition for nutritional status. About one fourth of the world population is suffering from anemia. It becomes very big challenges for all over the world. So, Kaviyarasi et al. studied the hemoglobin level of the adolescent girls was found to be 8.3mg/dl before intervention of CLP [7]. But after giving its supplemented diet, it was increased up to 12.9mg/dl. Bhandari et al. evaluated the other functional and phytochemical properties that are present in cauliflowers greens of different cultivars were glucosinolate profiles, vitamin C, total phenol, total flavonoid, and free sugar (glucose, fructose, and sucrose) content, fatty acid composition, and antioxidant activity [8].
So the present study was aimed to assess the anthropometric measurement and hemoglobin level to carry out the feeding trials of cauliflower leaves powder on selected rural school children and to find out effect on their nutritional status by incorporated into different value added products based on it.
Materials and Methods
Sample collection
Bengal gram was procured from the local market of Kumarganj, Ayodhya, UP. Cauliflower greens were arranged from the kitchen gardens in the university campus. It was cleaned, washed and dried in the oven at 65°C to 75°C for further use.
Cauliflower leaf powder preparation
Collection and sorting of leaves → washing in water → drying in hot air oven at 60°C-70°C Grinding in Mixer → storing in air tight containers for further nutritional analysis, product development and intervention studies.
Selection of subjects
A group of 60 students in age group of 10-12 years free from serious complication of any diseases were selected from Prathmic Vidyalaya, Bawan Dwitiya and Prathmic Vidyalaya, Narendra Nagar, Kumarganj, Ayodhya.
Anthropometric parameters
Height and weight of the subjects were measured before and after experimental period using method given by Jelliffe. Body Mass Index (BMI) of the subjects was calculated by standard method. Measurements of anthropometric parameters viz. body weight, height, mid upper arm circumference (MUAC), were recorded as per the following method.
Body weight: Body weight (kg) indicates the body mass and is a composite of all body constituents like water, minerals, fat, protein, bone etc. For the present study, body weight (kg) was taken by personal machine with the maximum capacity of 120 kg and the minimum division of 0.5 kg. The following precautions were taken to measure body weight (kg). School children were asked not to lean against or hold any support, while the weight (kg) was being recorded (Gibson, 1990).
Height: Height in (cm.) of the school children was taken by anthropometric rod. School children were asked to stand erect on a leveled surface, without shoes, looking straight with heels together and toes apart. The anthropometric rod was placed behind the school children in the centre of the heels perpendicular to the ground. The investigator standing on left side of the children held firmly the chin of the school children with his/her left hand and the occipital of the school children with his right little finger to maintain the Frankfurt plane horizontal. The readings were taken when the anthropometric rod was still in position (Gibson, 1990).
BMI Z-score: The nutritional status of children was assessed on the basis of BMI Z-score classification given by WHO:
≥ Median -2SD to+<1SD : Normal
Median < -2SD to >-3SD : Moderate Under nutrition
>Median -3SD : Severe Under nutrition
Median ≥+1SD to <+3 SD : Over weight
≥+3SD : Obesity
Children were categorized stunted i.e. low height-for-age based on WHO criteria which is Z-score lower than -2SD.
Likewise children were also categorized as wasted i.e. Low weight- for -age as per WHO criteria i.e. weight – for - age having less than -2SD.
Mid upper arm circumference (MUAC): MUAC (in cm.) indicates the status of muscle development. For the present investigation, MUAC was taken using fiber glass tape with minimum count of 0.1cm. The midpoint between the tip of the acromion of scapula and the tip of the olecranon process of the (forearm bone) ulna, with the arm flexed at the elbow at right angle; was marked with a marker pen. Arm of subject was hanged freely and the fiber glass tape was gently, but firmly placed embracing the arm without exerting too much pressure on the soft tissues. The reading was taken to the nearest millimeter, with tape still in position [9].
Prepared supplementary foods were fed to selected children
Group I – children of group I were given placebo (control)
Group II - children were given most acceptable food for three months
Feeding trials were carried out for a period of three months with daily dosage of four nos. These supplements were given along with their daily diet. After feeding trials blood samples were again collected and analyzed.
Biochemical analysis
Haemoglobin estimation: Blood sample were collected and analyzed for haemoglobin content. The In charge of Community Health Centre, Milkipur (Dr. Santosh Kumar) was consulted and haemoglobin estimation of school children was done by Lab. Technician (Mr. Rajveer Singh) of their CHC using following method:
Sahil’s method: The finger tip of subjects is cleaned and 0.02 ml blood is drawn in a dry pipette by pricking the fingertip with a sterilized disposable needle. Then blood had blown in to hemoglobin tube that contains N/10 HCL up to the lower mark. This blood is diluted with the help of distilled water and is mixed with glass rod till the colour is matched with standard hemoglobin “A”. The reading was taken in g%.
Statistical analysis
The obtained data on food and nutrient intake, anthropometric measurement and hemoglobin profile of subjects were analyzed by using analysis of variance (ANOVA) technique as suggested by Gomez and Gomez and t-test. Critical difference was calculated to draw valid conclusions
Results and Discussion
To ascertain the effect of developed iron rich food products on nutritional status of school going children, an intervention study was conducted on 60 school children in the age group of 10-12 years. There were total 30 children were in the control group and 30 children were in experimental group. The data on anthropometric measurements and haemoglobin content as well as dietary intake of children was collected before and after intervention.
The data presented in Table 1 shows that out of total, 43.3% subjects were boys and 56.6% were girls. 58.4% were in the age group of 10 year+ whereas 41.6% were in the age group of 11 year+(Figures in Parenthesis indicate percentage).
| Age (year) | Boys | Girls | Total (N=60) |
|---|---|---|---|
| 10 + | 15 (25.0) | 20 (33.3) | 35 (58.4) |
| 11+ | 11 (18.3) | 14 (23.3) | 25 (41.6) |
| Total | 26 (43.3) | 34 (56.6) | 60 (100) |
(Figures in Parenthesis indicate percentage)
Table 1: Gender distribution.
The data given in Table 2 illustrates the age-wise mean anthropometric measurements of children. It revealed that mean height (cm), weight (kg), BMI (kg/m2) and MUAC (cm) of boys were 127.82, 22.38, 13.60 and 17.58, respectively whereas; in case of girls the particular values were 127.73, 22.56, 13.6 and 17.74.
| Age (year) |
Height (cm) Mean ± SD |
Weight (kg) Mean ± SD |
BMI (kg/m2) Mean ± SD |
MUAC (cm) Mean ± SD |
|---|---|---|---|---|
| Boys | ||||
| 10 + | 123.46 ± 3.12 | 21.13 ± 3.11 | 13.72 ± 0.15 | 17.26 ± 0.26 |
| 11 + | 132.18 ± 6.58 | 23.63 ± 2.93 | 13.48 ± 0.21 | 17.90 ± 0.34 |
| Mean | 127.82 ± 6.58 | 22.38 ± 3.02 | 13.6 ± 0.18 | 17.58 ± 0.3 |
| Girls | ||||
| 10 + | 125.95 ± 7.93 | 21.05 ± 2.04 | 13.14 ± 0.28 | 17.2 ± 0.34 |
| 11 + | 129.5 ± 3.43 | 24.07 ± 2.58 | 14.06 ± 0.36 | 18.28 ± 0.56 |
| Mean | 127.73 ± 5.7 | 22.56 ± 2.31 | 13.60 ± 0.32 | 17.74 ± 0.45 |
Table 2: Age-wise anthropometric measurements of Boys and Girls before intervention.
Before intervention, it was necessary to know the average deficient relevancy, so when compared with NCHS standards in Table 3, the mean height of boys was 11.82% less, on the counterpart the mean deficit was observed as 12.17%, compared to NCHS standards.
| Age (year) |
Boys | Girls | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Average Height (cm.) | NCHS Standard (cm.) | Deficit (%) | Average Height (cm.) | NCHS Standard | Deficit (%) | Average Height (cm.) | NCHS Standard (cm.) | Deficit (%) | |
| 10 + | 123.46 | 141.8 | 12.93 | 125.95 | 141.15 | 10.76 | 124.70 | 141.47 | 11.85 |
| 11 + | 132.18 | 148.05 | 10.71 | 129.5 | 149.85 | 13.58 | 130.84 | 148.95 | 12.15 |
| Mean | 127.82 | 144.93 | 11.82 | 127.72 | 145.50 | 12.17 | 127.77 | 145.21 | 12.00 |
*National Center for Health Statistics
Table 3: Comparison of height (cm.) of children with NCHS* standard before intervention.
From the Table 4, there was drastic average weight deficient in percentage of boys as 38.63% reported and approximately same occurrence of 40.81% was observed in girls on the other side. In total, about 40 percent children were deficient when compared with the weight of National Council for Health Standards (NCHS).
| Age (year) | Boys | Girls | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Average Weight (Kg.) |
NCHS Standard (Kg.) |
Deficit (%) |
Average Weight (Kg.) |
NCHS Standard (Kg.) |
Deficit (%) |
Average Weight (Kg.) |
NCHS Standard (Kg.) |
Deficit (%) |
|
| 10 + | 21.13 | 34.3 | 38.39 | 21.05 | 35.85 | 41.28 | 21.09 | 35.07 | 39.86 |
| 11 + | 23.63 | 38.65 | 38.86 | 24.07 | 40.35 | 40.34 | 23.85 | 39.50 | 39.62 |
| Mean | 22.38 | 36.48 | 38.63 | 22.56 | 38.10 | 40.81 | 22.47 | 37.29 | 39.74 |
*National Center for Health Statistics
Table 4: Comparison of weight (Kg.) of children with *NCHS standard before intervention.
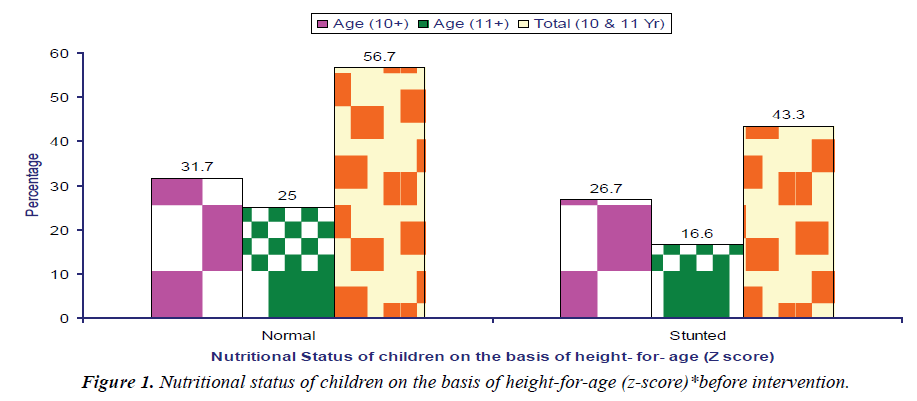
Data presented in Table 5 indicates the normal and stunted status of the both genders at same age in defined manner. Overall one fourth of the selected children were stunted. Also from the Figure 1, it clearly specifies that 25% boys and 31.6% girls were having normal nutritional status on the basis of Height-for-age (Z score) before intervention and 18.3% boys and 25% girls were found to be stunted i.e. having less height for age.
| Age (year) | Boys | Girls | Total(N=60) | |||||
|---|---|---|---|---|---|---|---|---|
| No. | Normal | Stunted | No. | Normal | Stunted | Normal | Stunted | |
| 10+ | 15 | 8(13.3) | 7(11.6) | 20 | 11(18.3) | 9(15.0) | 19(31.7) | 16(26.7) |
| 11+ | 11 | 7(11.6) | 4(6.67) | 14 | 8(13.3) | 6(10.0) | 15(25.0) | 10(16.6) |
| Total | 26 | 15(25.0) | 11(18.3) | 34 | 19(31.6) | 15(25.0) | 34(56.7) | 26(43.3) |
Table 5: Nutritional status of children on the basis of height- for -age (z-score)*before intervention.
On the basis of BMI (z-score)* classification, totally on an average, only 19.91% children were normal, 56.78% were moderately malnourished and 23.30% were severely malnourished as drawn out from the Table 6. Further on the basis of BMI (Z-score) 19.23% boys and 20.59% girls were normal. Prevalence of moderate and severe under nutrition among boys and girls was found as 57.69 and 55.88, 23.08 and 23.53 percent, respectively. No child was obese or over weight found in selected subjects.
| Gender | Normal | Moderate | Severe under nutrition | Over weight |
|---|---|---|---|---|
| Boys n=26 | 5(19.23) | 15(57.69) | 6(23.08) | - |
| Girls n=34 | 7(20.59) | 19(55.88) | 8(23.53) | - |
| Total n=60 | 12(20.00) | 34(56.67) | 14(23.33) | - |
Table 6: Gender-wise nutritional status of school children as per BMI (z-score)*before intervention.
After gender wise allocation, the Age-wise distribution of selected children according to BMI before intervention is given in Table 7 and showed that the total percentage of normal, moderately and severely malnourished children in the age group of 10 year+ were as 37.14, 40.0 and 22.86% respectively. Although, in the age group of 11 year+, there was normal (44%), moderately (32%) and severely malnourished (24%) children found.
| Age (year) |
Normal | Moderate | Severe | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Boys n (%) |
Girls n (%) |
Total n (%) |
Boys n (%) |
Girls n (%) |
Total n (%) |
Boys n (%) |
Girls n (%) |
Total n (%) |
|
| 10+ N=35 |
3 (8.57) | 10 (28.57) | 13 (37.14) | 9 (25.71) | 5 (14.29) | 14 (40.0) | 3 (8.57) | 5 (14.29) | 8 (22.86) |
| 11+ N=25 |
2 (8.0) | 9 (36.0) | 11 (44.0) | 6 (24.0) | 2 (8.0) | 8 (32.0) | 3(12.0) | 3 (12.0) | 6 (24.0) |
Table 7: Age?wise distribution of selected children according to BMI before intervention.
From the Table 8, the total Average haemoglobin level of 10 year+ and 11 year+ boys and girls were reported as 10.1 and 10.3 g/; dl correspondingly, while the average WHO cut off point is 11.5 g/dl and 12 g/dl, respectively. The deficient percentages in boys and girls of 10 year+ and 11 year+ imply 12.1 and 14.1 haemoglobin level which means the anemia prevalence distributed among them.
| Age | Boys | Girls | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Average Hb (g/dl) | WHO cut-off point Hb (g/dl)* | Deficit % | No | Average Hb (g/dl) | WHO cut-off point Hb (g/dl)* | Deficit % | No | Average Hb (g/dl) | WHO cut-off point Hb (g/dl)* | Deficit % | |
| 10+ | 15 | 10.2 | 11.5 | 11.3 | 20 | 10.0 | 11.5 | 13.0 | 35 | 10.1 | 11.5 | 12.1 |
| 11+ | 11 | 9.7 | 12.0 | 19.1 | 14 | 10.9 | 12.0 | 9.16 | 25 | 10.3 | 12.0 | 14.1 |
Table 8: Prevalence of anemia among selected school children before intervention.
After intervention of feeding trial for three months
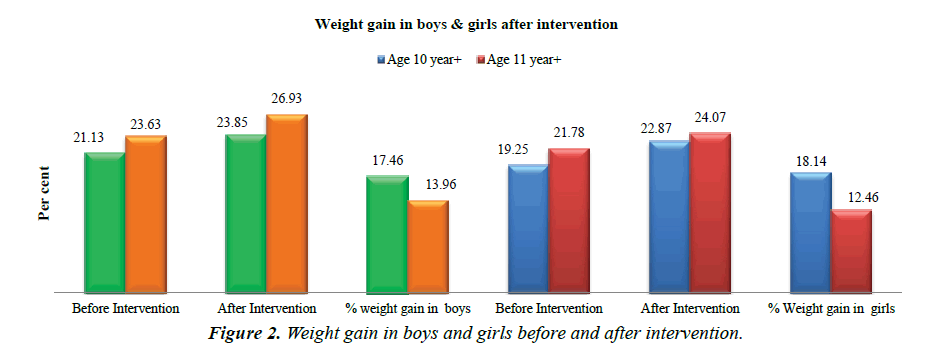
Prepared supplementary foods i.e., Fara, Dhokla and Laddoo alternately were fed to selected children for three months. These supplements were given along with their daily diet. After feeding trials, blood samples were again collected and analyzed for its haemoglobin content. Anthropometric measurements were also taken before and after intervention and compared both with the earlier data and before intervention. The data presented in Table 9 showed the significant gain in weight of Boys both aged 10 year+(17.46%) and 11 year+(13.96%). On an Average, 13.45 weight gains were accounted for boys. The percent gain in weight of girls of age 10 year+ and 11+ years were 18.14 and 12.46% correspondingly. Mean gain weights in girls were informed as 14.66 percent as depicted well in Figure 2 also.
| Weight (Kg) | Age 10year+ Mean ± SD |
Age 11 years+ Mean ± SD |
Average |
|---|---|---|---|
| Boys | |||
| Before Intervention | 21.13 ± 3.11 | 23.63 ± 2.93 | 22.38 |
| After Intervention | 23.85 ± 2.93 | 26.93 ± 2.43 | 25.39 |
| % weight gain | 17.46 | 13.96 | 13.45 |
| Girls | |||
| Before Intervention | 19.25 ± 2.04 | 21.78 ± 2.58 | 20.52 |
| After Intervention | 22.87 ± 2.17 | 24.07 ± 3.58 | 23.47 |
| % weight gain | 18.14 | 12.46 | 14.66 |
Table 9: Comparison of weight (Kg) of boys and girls before and after intervention.
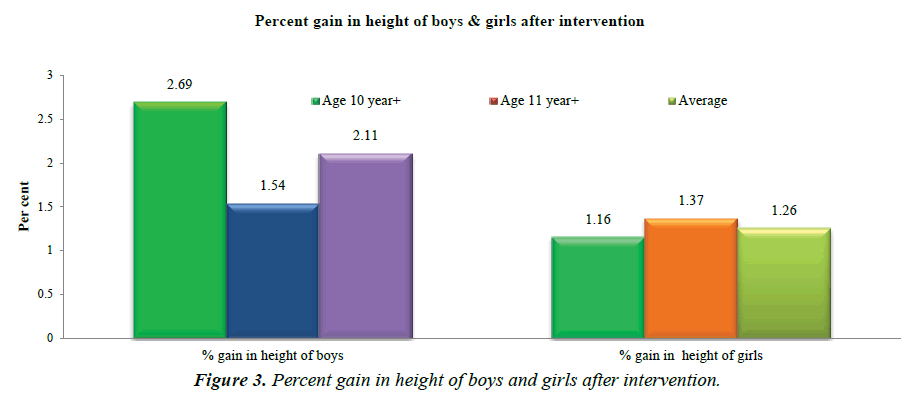
Data related to height of boys before and after intervention is presented in Table 10, Percent increase in height of boys aged 10 years+ and 11 year+ was 2.69 and 1.54. While, in case of girls the respective increase in the height of 10 year+ and 11 year+ was 1.16 and 1.37% (Figure 3).
| Height (cm) | Age 10 year+ | Age 11 year+ | Average |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Boys | |||
| Before Intervention | 123.46 ± 7.12 | 132.18 ± 6.58 | 127.82 |
| After Intervention | 126.79 ± 6.50 | 134.22 ± 5.58 | 130.505 |
| % gain in height of boys | 2.69 | 1.54 | 2.11 |
| Girls | |||
| Before Intervention | 125.95± 7.93 | 129.50± 3.43 | 127.82 |
| After Intervention | 127.42± 6.63 | 131.28 ± 7.36 | 129.35 |
| % gain in height of girls | 1.16 | 1.37 | 1.26 |
Table 10: Comparison of height (cm) of boys and girls before and after intervention.
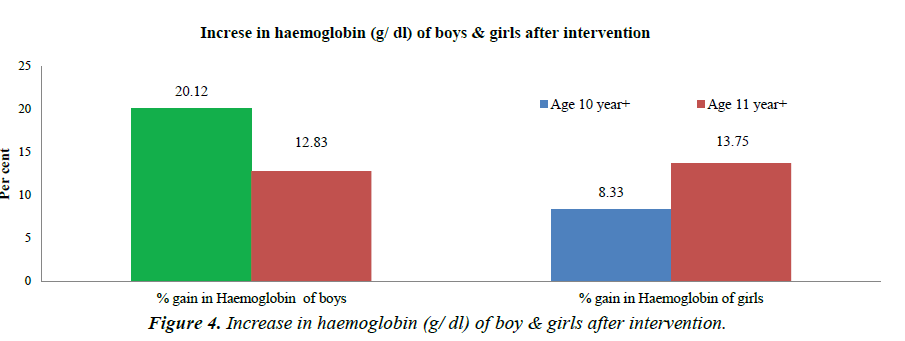
After feeding the supplements and the Mean haemoglobin (g/ dl) of boys aged 10 year+ was 8.25 which increased to 9.91 g/dl i.e. an increase of 20.12% was observed after 3 months of feeding. In case of boys aged 11+ mean haemoglobin was 10.05 which increased to 11.34 i.e. 12.83% (Table 11).
| Haemoglobin ( g/ dl) | Age 10 year+ | Age 11 year+ |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Boys | ||
| Before Intervention | 8.25 ± 2.054 | 10.05 ± 0.830 |
| After Intervention | 9.91 ± 1.591 | 11.34 ± 0.807 |
| % Increase in Haemoglobin of boys | 20.12 | 12.83 |
| Girls | ||
| Before Intervention | 9.84 ± 0.837 | 10.18 ± 0.986 |
| After Intervention | 10.66 ± 0.694 | 11.58 ± 1.152 |
| % Increase in Haemoglobin of girls | 8.33 | 13.75 |
Table 11: Comparison of haemoglobin (g/ dl) of boys and girls before and after intervention.
In girls aged 10 year+ before intervention mean haemoglobin (g/dl) was 9.84 which became 10.66 g/dl i.e. an increase of 8.33%. While in case of girls aged 11 year+ before intervention value was 10.18 g and after intervention it increased to 11.58 g/dl i.e. and increase of 13.75% was observed. Nearly, Singh et al. reported increase in heamoglobin content in by 9.42% when supplementation of functional beverages was given to sports women in which CLP was added proportionately [10]. Similar experiment was conducted and supported by the Kaviyarasi et al. [7] that there was increased in mean haemoglobin level of the selected subjects, from 12 to 12.5 g/dl after supplementation of 50 g cauliflower greens poriyal for 90 days (Figure 4).
Conclusion
It can be concluded that the intervention studies were conducted on school children providing 1/3 of iron requirement using three standardizes products namely Fara, Dhokla and laddoo alternatively for a period of three months. Before intervention mean height and weight of the 10-12 years aged school children was 12 and 39.74% respectively less than NCHS standards which shows monitoring is required to attain the desired level. The Nutritional assessments of 10-12 years aged school children on the basis of height for age (Z-scores) showed that 56.7% were normal and 43.3% stunted. After intervention studies, Average gain in weight of boys and girls of age 10+ and 11+ years after intervention was 17.46, 13.96 and 18.14, 12.46 percent, respectively. The Average gain in height of boys and girls of aged 10+ and 11+ year was 2.69, 1.54 percent and 1.16, 1.37 percent respectively was reported. Moreover, percent increase in hemoglobin level of boys and girls of age 10+ and 11+ year students were 20.12, 12.83 and 8.33, 13.75 respectively. It reflects that if the consumption of green leaves of cauliflower at household level become frequent then it might be the strong step/remedies to eradicate against micronutrient deficiencies especially anemia that are prevalent in every country.
Acknowledgement
The financial assistance provided by U.P. Council of Agriculture Research, Lucknow, for carrying out this research work is greatly acknowledged.
References
- Sharmilan P, Mary J, Dorothy J. Bioactive compounds in cauliflower leaves (brassica oleracea var.botrytis) using GCMS. Int J Recent Sci Res 2016; 7: 10459-10463.
- Pankar SA, Bornare DT. Studies on cauliflower leaves powder and its waste utilization in traditional product. Int J Agric Eng 2018; 11: 95-98.
- Wani TA, Sood M, Kaul RK. Nutritional and sensory properties of roasted wheat noodles supplemented with cauliflower leaf powder. Annals Food Sci Technol. 2011; 12: 102-107.
- Chakraborty S, Datta S. Estimation of Macro-Nutrients in Domestically Processed Cauliflower Leaf Powder. Int J Sci Res 2016; 5: 2094-2096.
- Joshi P, Mathur B. Preparation of value added products from the leaf powders of dehydrated less utilized green leafy vegetables. Int J Agr Res 2013, 1: 65-69.
- Singh G, Kawatra A, Sehgal S. Development and Nutritional Evaluation of products prepared from dried powder of Cauliflower leaves. J Food Sci Tech 2005; 42: 137-139.
- Kaviyarasi R, Abirami J. Effect of cauliflower greens poriyal supplementation on blood haemoglobin levels of anaemic adolescent girls. Int J Sci Eng Res 2017; 8: 315-322.
- Bhandari SR, Kwak JH. Chemical Composition and Antioxidant Activity in Different Tissues of Brassica Vegetables. Molecules 2015; 20: 1228-1243.
- Gibson RS. Principles of Nutritional Assessment. Oxford: Oxford University Press 1990.
- Singh A, Kochhar A. Study on the efficacy of supplementation of functional beverage on the blood profile of Sportswomen. Int J Sci Res 2012; 2: 1-5.