ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 4
Application of hemihepatectomy combined with vascular resection and reconstruction in bismuth III and IV hilar cholangiocarcinoma
1Department of Hepatobiliary Surgery, Zhangzhou Zhengxing Hospital, China
2Department of Hepatobiliary Surgery, the Affiliated Hospital (Group) of Putian University, China
- *Corresponding Author:
- Jiang X
Department of Hepatobiliary Surgery
The Affiliated Hospital (Group) of Putian University, China
Accepted on September 15, 2016
Objective: This study aims to discuss the applied value of hemihepatectomy in combination with vascular resection and reconstruction in hilar cholangiocarcinoma.
Methods: Out of 113 cases of hilar cholangiocarcinoma, 25 cases were classified as Bismuth IIIa, IIIb and IV. Hemihepatectomy in combination with vascular resection and reconstruction was performed by using the basic surgical operation method (A) to achieve radical cure. The following cases were included in this study: 2 cases received A+right hemihepatectomy+pancreatoduodenectomy+resection and reconstruction of the initial part of the right portal vein; 7 cases received A+right hemihepatectomy +resection and reconstruction of the initial part of the right portal vein; 5 cases received A+right hemihepatectomy+resection of the hepatic artery; 3 cases received A+left hemihepatectomy+resection of the left caudate lobe+resection and reconstruction of the initial part of the left portal vein+resection of the hepatic artery; 4 cases received A+left hemihepatectomy+resection of the left caudate lobe; and 4 cases received A+left hemihepatectomy+resection of the caudate lobe+resection and reconstruction of the initial part of the left portal vein.
Results: Among the 93 cases of hilar cholangiocarcinoma, the 25 cases with Bismuth IIIa, IIIb and IV hilar cholangiocarcinoma were subjected to hemihepatectomy in combination with vascular resection and reconstruction to achieve radical cure. Postoperative survival rates for one, two, three and five years were 52%, 28%, 12% and 8%, respectively.
Conclusion: The combined use of hemihepatectomy and vascular resection and reconstruction could increase the radical resection rate of hilar cholangiocarcinoma.
Keywords
Bile duct neoplasms, Hepatectomy, Vessel reconstruction.
Introduction
Hilar bile duct cancer remains one of the most difficult management problems in terms of staging and radical treatment. Surgical resection with complete removal of all cancer is the only chance for cure and long-term survival. Indeed, local or hilar resections, including that of the extrahepatic and supra-pancreatic biliary tract, have been reported to result in a high percentage (76%) of localized regional recurrence even after formal curative resections. Moreover, bile duct resection alone leads to high local recurrence rates and has low five-year survival rate because of the early involvement of the hepatic duct confluences and caudate lobe branches [1,2].
In theory, radical excisional therapy for patients with hilar bile duct cancer often necessitates extensive hepatic resection. Although many surgeons have emphasized the importance of hepatic resections, the percentage of patients who undergo major hepatic resection is still limited, presumably because of fear of the high incidence of liver failure associated with the said treatment.
In recent years, the surgical treatment for hilar cholangiocarcinoma has clearly progressed. As a result, surgical resection and survival rates have been significantly improved. In an innovative study of 59 patients with Bismuth III and IV hilar cholangiocarcinoma who underwent liver resection with curative intent, survival rates at one, three and five years were 82%, 45% and 20%, respectively [3]. In addition, for the last two decades, most centres have already adopted this approach, and the outcomes were better compared with that of the local resection only. Reported curative resection rate was at 70% with a five-year survival rate ranging from 10% to 40% [4-7].
The aim of this study was to assess the outcome following the implementation of the radical approach for the management of Bismuth III and IV hilar cholangiocarcinomas. From 1998 to 2010, 113 patients with hilar cholangiocarcinoma were treated in which 65 of them received surgical operation. According to the Bismuth classification [8], 25 patients were diagnosed as having Bismuth IIIa, IIIb and IV hilar cholangiocarcinoma and underwent hemihepatectomy in combination with vascular resection and reconstruction to achieve radical cure.
Subjects and Methods
General data
A total of 15 patients were recruited in this study, including 14 males and 11 females, with an average age of 61.5 years (ranging from 45 years to 80 years). The initial clinical manifestations were as follows: painless jaundices (25 cases), skin itching (14 cases), anorexia (11 cases) and argil-like defecate (7 cases). The serum bilirubin level of this group was at 100.6 μmol/L to 546 μmol/L (mean 279 μmol/L), whereas the serum albumin level was at 31.5 g/L to 40 g/L (mean 33.5 g/L). Preoperative colour Doppler ultrasound and MRCP examinations were carried out in this study. On the basis of the results of the MRCP examination and according to the Bismuth classification, 14 cases were classified as Bismuth IIIa (common hepatic duct and right liver tube carcinoma, 56%), 8 cases as Bismuth IIIb (common hepatic duct and left liver tube carcinoma, 32%) and 3 cases as Bismuth IV (left or right liver tube carcinoma involving the liver tube of second level and above, 12%). This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Zhangzhou Hospital Affiliated to Fujian Medical University. Written informed consent was obtained from all participants.
Surgery
A reverse-L incision at the midsection was made on the patients while under tracheal intubation anaesthesia. The basic surgical procedures were as follows: resecting the Hilar bile duct, common bile duct and gallbladder, while simultaneously resecting all the lymph nodes, nerves, fat and connective tissues in the hepatoduodenal ligament to completely expose the portal vein and hepatic artery. This procedure is called ‘skeletonization resection’. Hereinafter, we named the procedure as ‘basic surgical operation method (A)’. On the basis of the classification and according to the basic surgical operation method (A), the patients received the following treatment accordingly: two cases received A+right hemihepatectomy+pancreatoduodenectomy+resection and reconstruction of the initial part of the right portal vein; 7 cases received A+right hemihepatectomy+resection and reconstruction of the initial part of the right portal vein; 5 cases received A+right hemihepatectomy+resection of the hepatic artery; 3 cases received A+left hemihepatectomy+resection of the left caudate lobe+resection and reconstruction of the initial part of the left portal vein+resection of the hepatic artery; 4 cases received A+left hemihepatectomy+resection of the left caudate lobe; and 4 cases received A+left hemihepatectomy +resection of the caudate lobe+resection and reconstruction of the initial part of the left portal vein.
Results
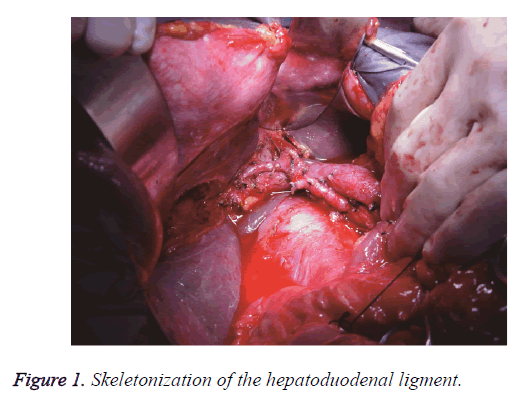
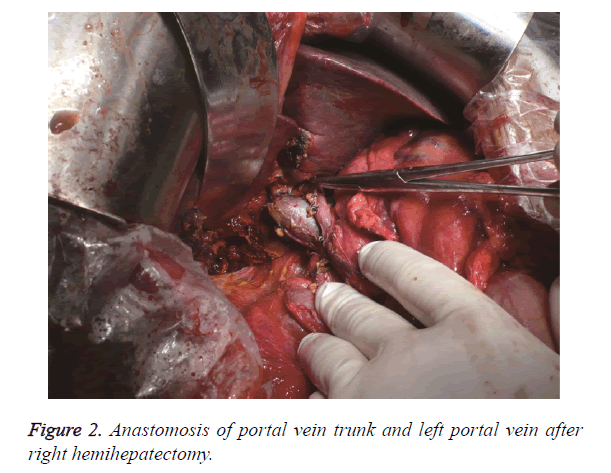
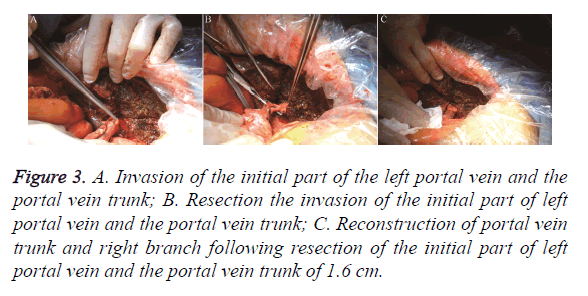
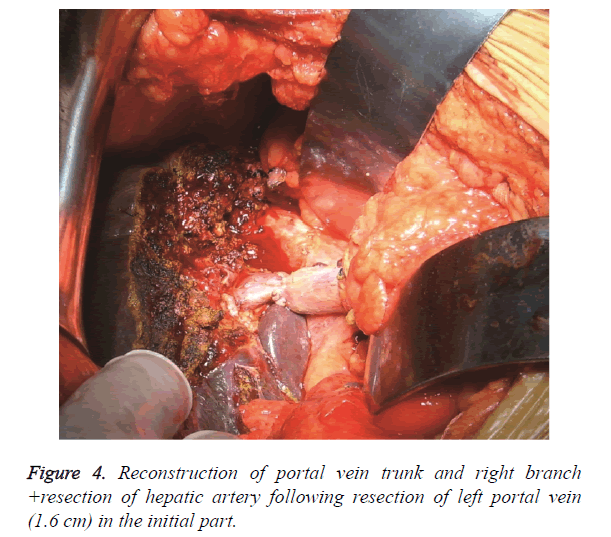
The surgical methods were chosen according to the Bismuth classification. The Hilar bile duct, common bile duct and gallbladder were resected simultaneously with the lymph nodes, nerves, fat and connective tissues inside the hepatoduodenal ligament to completely expose the portal vein and hepatic artery. This procedure is called ‘skeletonization resection’ (Figure 1). Among the 25 patients, 14 cases were subjected to right hemihepatectomy, whereas 11 cases were subjected to left hemihepatectomy. In the 14 cases that were subjected to right hemihepatectomy, the initial part of the right portal vein was involved, in which 7 cases had 0.5 cm to 0.8 cm of the initial part of the right branch involved. A wedge cut of 1 cm on the main portal vein at the initial part of the right portal vein was made. Continuous suture was performed by using polin line 0/5 to reconstruct the main portal vein (Figure 2). In the 2 other cases, 0.3 cm of the initial part of the right portal vein was involved, and the involved 0.5 cm trunk at the initial part of the right portal vein was resected to reconstruct the portal vein. In the remaining 5 cases, the hepatic artery with invasion and was surrounded by tumours was resected. Tumour invasion exists in the initial part of the left portal vein of the 11 cases that were subjected to left hemihepatectomy. In the 4 cases with tumour invasion of 0.8 cm into the portal vein, the 1 cm trunk in the initial part of the left portal vein was cut off, and the trunk of the portal vein was reconstructed. In the 3 cases with tumour invasion in 1.3 cm of the portal vein, the initial part and 1.6 cm of the trunk of the left portal vein were cut off, and the main portal vein was anastomosed with the right portal vein from end to end (Figure 3). In the 2 cases with tumour invasion in 0.6 cm of the portal vein and hepatic artery, 1 cm of the trunk in the initial part of the left portal vein was cut off, and the main portal vein was anastomosed with the left portal vein from end to end. Moreover, the hepatic artery was resected (Figure 4). In the remaining 2 cases, the structured hepatic artery, with invasion and was surrounded by tumour, was resected. In some cases, the tumours invading the hepatic artery could be separated to avoid resection or reconstruction of the hepatic artery. In this group, 17 cases had hepatic artery invasion, 5 cases received separation of tumour from the hepatic artery. In the remaining 12 cases, the hepatic artery that was surrounded by the tumour was thinned and resected, and postoperative liver failure did not occur.
Figure 3. A. Invasion of the initial part of the left portal vein and the portal vein trunk; B. Resection the invasion of the initial part of left portal vein and the portal vein trunk; C. Reconstruction of portal vein trunk and right branch following resection of the initial part of left portal vein and the portal vein trunk of 1.6 cm.
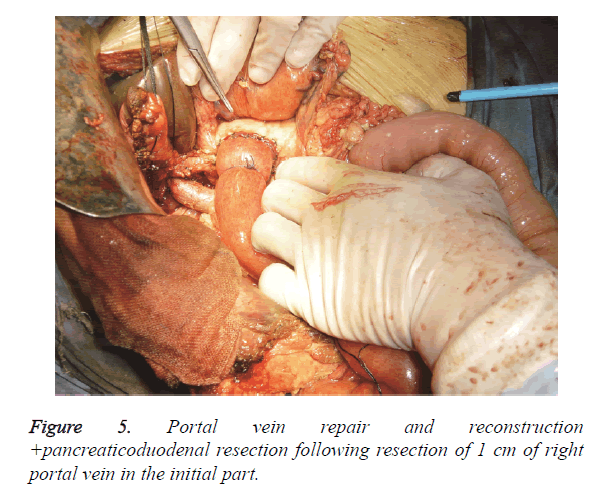
A total of 11 cases had postoperative biliary fistula (44%) and were all self-healed within 5 days to 25 days after operation. A total of 8 cases had subphrenic infection and were cured by drainage. No deaths occurred during hospitalization. Colour Doppler ultrasound examination was routinely conducted for six months after the reconstruction of the portal vein. At the first, second and fourth months, no portal vein stenosis or thrombus was observed. Liver failure was not detected in the patients subjected to hepatic artery resection. In this group, 2 cases received right hemihepatectomy+extrahepatic bile duct resection+pancreaticoduodenal resection+portal vein reconstruction and survived for nine months (Figure 5).
In all cases, the survival rates for one, two, three and five years were 52%, 28%, 12% and 8%, respectively. The average postoperative survival time was 13.5 months (with a range of 8 months to 48 months), and the cause of death was tumour recurrence.
Postoperative pathological results revealed a tumour cell invasion in the initial parts of the left and right portal veins, but no tumour cell invasion was seen at the distal part of the tumour resection. We observed 12 cases of well-differentiated adenocarcinoma, 7 cases of moderately differentiated adenocarcinoma and 4 cases of low-differentiated adenocarcinoma. Moreover, 13 cases had negative bile duct resection margin, in which 6 cases underwent severe atypical dysplasia at the resection margin.
Discussion
Adenocarcinoma of the hepatic duct at its bifurcation (hilar cholangiocarcinoma) was defined by Klatskin [9]. The surgically resectable rate of hilar cholangiocarcinoma is low because of its difficult early diagnosis, the involvement of important structures at the hepatic hilium where the tumour is found, and the complicated regional anatomy. However, with the changes in cure viewpoint, the advancement of operation techniques and the renewed operation methods and procedures, the surgically resectable rate has been substantially improved since the 1990s, and even went up from 48.5% to 74% in the last decade [10-13]. Currently, surgical operation is still the main method for curing hilar cholangiocarcinoma and is still the only effective method to achieve radical cure.
Most studies reported that the resection methods are decided according to Bismuth classification [14,15]. Hilar cholangiocarcinoma is characterized by invasive growth and diffusion into the interspace of the lymphatic tissue around the bile duct, vessels and nerves. Skeletonization resection is the basic method used to cure hilar cholangiocarcinoma.
In recent years, with the better understanding of its biological characteristics and through the pathological and statistical analysis of large-scale cases, hilar cholangiocarcinoma is shown to be diffused along the intrahepatic bile duct, produced many satellite foci and diffused in the surrounding vessels, nerves and lymph vessels in its early stages before the surrounding connective tissues are involved [16,17]. The invasion scale of the hilar cholangiocarcinoma of hepatic bile duct is more serious than that of the duodenum. Thus, resecting the hilar bile duct tumour will result in a high residual tumour margin rate. In this study, hepatectomy of tumour invasion is recommended for hilar cholangiocarcinoma because this approach can increase the radical cure rate of the resection from 58% to 100% compared with the 38% to 45% of the nonhepatectomy. Resection of a quadrate lobe of the liver or part of the liver can expose the branch of hepatobiliary tube clearer, which makes this method convenient for the resection of the tumour and bile duct. However for the Bismuth IIIa, IIIb and IV types, resecting only a quadrate lobe of the liver or part of the liver is not enough. To achieve pathological radical cure (R0), trisegmentectomy of the affected liver should be conducted [18]. Among the 25 cases, 14 cases were subjected to right hemihepatectomy, whereas 11 cases were subjected to left hemihepatectomy. A total of 19 cases obtained negative resection margin (R0), whereas 4 cases had moderate to severe atypical hyperplasia, in which 2 cases had suspected cancer cells of mainly type IV. Given the invasive growth of the hilar cholangiocarcinoma, the vessels are always involved, such that resecting only the affected half liver will not achieve radical cure. The resection of the involved portal vein or hepatic artery is necessary to complete the resection of hilar cholangiocarcinoma. To increase the radical rate of tumour resection, the vessels should be resected and reconstructed [19]. In this study, intraoperative exploration showed that the portal vein and proper hepatic artery or its left and right branch experienced tumour invasion of varying degrees. Hemihepatectomy and vessel resection+reconstruction were carried out to achieve radical cure. Portal vein resection and reconstruction should be performed in cases with the following conditions [20]; 1) tumour invasion in the main portal vein; 2) invasion in the initial part of the left or right branch of the portal vein; and 3) invasion in the left and right bifurcation of the portal vein. The portal vein with tumour invasion appears as a venous wall that is becoming thick, stiff and hoar. If the invasion scale of the venous wall is below 2 cm, the tumour and part of the venous wall of the portal vein are resected. Subsequently, portal vein repair or reconstruction is performed. If the invasive scale of the venous wall is more than 2 cm, the autologous internal jugular vein or vascular prosthesis is used for portal vein reconstruction following the resection of the vessel. The indications for hepatic artery resection are as follows [20]; 1) Hepatic artery has tumour invasion and is surrounded by tumour; and 2) the tumour invasion scale of hepatic artery is more than 2 cm, the cavity is thinned, the wall is thickened and distal artery pulsatility is weakened. Patients with hepatic artery resection need to keep the portal vein expanded to avoid liver failure. In this group, 12 cases received hepatic artery resection and obtained satisfactory postoperative liver function recovery.
Combined liver, bile and pancreaticoduodenal resection is mainly used in patients with diffused cancer invasion in the bile duct of the pancreas and pancreatic head and belongs to hilar cholangiocarcinoma extended radical operation. This surgical method is feasible, but because of the significant surgical trauma and complicated technology, only few cases were reported [21-23]. Additional cases are needed to evaluate the curative effectiveness of the method. Hilar cholangiocarcinoma extended radical operation is commonly preferred over pancreaticoduodenal hemihepatectomy, hemihepatectomy, or liver transplantation. Some scholars are concerned about the extension of the surgical treatment to hilar cholangiocarcinoma because of the serious complications and high operation death rate of the procedure. Cautious use of this operation method should be done and the surgical complications should be considered to achieve radical cure resection. However, no reports are available on large-scale cases of the extended radical operation of hilar cholangiocarcinoma and on prospective comparison on the risk and effectiveness of the treatment. To improve the effect of the surgical treatment, extending the resection scale seems to be an inevitable trend, and frozen section examination during the operation is necessary. The operation must be carefully performed when the surgical condition, experience and adequate preoperative preparation are lacking.
Hilar cholangiocarcinoma is a type of polymorphism disease, and only a few cases present benign tendency. Along with the improvement of the surgical treatment, the perspective on the cure of this disease becomes optimistic, and the operation method becomes standardized. The surgical treatment can prolong the life span and improve the life quality of the patient. However, we are not certain whether the treatment has a longterm curative effect. If the local recurrence rate of the tumour is high, then the long-term survival rate becomes low. Patients with hilar cholangiocarcinoma who were subjected to radical resection survive longer than those subjected to palliative resection (incomplete resection) [24]. Among the 25 cases, 52% (13/25) survived for one year, 28% (7/25) survived for two years, 12% (3/25) survived for three years and 8% (2/25) survived for five years. We must pay active surgical attitude towards the hilar cholangiocarcinoma. In addition, tumour invasion into the portal vein is not an operative contraindication as long as we carefully perform preoperative evaluation and select the right patients. In cases with Bismuth IIIa, IIIb and IV types of hilar cholangiocarcinoma, we applied hemihepatectomy combined with vessel resection +reconstruction and even radical operation to extend the surgical resection scale and to improve the radical curative effect.
Conclusions
In cases with Bismuth IIIa, IIIb and IV types of hilar cholangiocarcinoma, the combined use of hemihepatectomy and vascular resection and reconstruction could increase the radical resection rate of hilar cholangiocarcinoma and to improve the radical curative effect.
References
- Klempnauer J, Ridder GJ, von Wasielewski R, Werner M, Weimann A, Pichlmayr R. Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors. J Clin Oncol 1997; 15: 947-954.
- Bismuth H. Resection or palliation: priority of surgery in the treatment of hilar cancer. World J Surg 1988; 12: 39.
- Baton O, Azoulay D, Adam DV, Castaing D. Major hepatectomy for hilar cholangiocarcinoma type 3 and 4: prognostic factors and long term outcomes. J Am Coll Surg 2007; 204: 250-260.
- Ercolani G, Zanello M, Grazi GL, Cescon M, Ravaioli M, Del Gaudio M. Changes in the surgical approach to hilar cholangiocarcinoma during an 18-year period in a Western single center. J Hepatobiliary Pancreat Sci 2010; 17: 329-337.
- Mansfield SD, Barakat O, Charnley RM, Jaques BC, O'Suilleabhain CB, Atherton PJ. Management of hilar cholangiocarcinoma in the North of England: pathology, treatment, and outcome. World J Gastroenterol 2005; 11: 7625-7630.
- Papoulas M, Lubezky N, Goykhman Y, Kori I, Santo E, Nakache R. Contemporary Surgical Approach to Hilar Cholangiocarcinoma. Isr Med Assoc J 2011; 13: 99-103.
- Zhang BY, Lu Y, Dong Q, Sun CD, Mu P. Surgical treatment and prognostic analysis of 93 cases of hilar cholangiocarcinoma. Am J Med Sci 2010; 39: 221-224.
- Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 1975; 140: 170-178.
- Klatskin G. Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. An unusual tumor with distinctive clinical and pathological features. Am J Med 1965; 38: 241-256.
- Parikh AA, Abdalla EK, Vauthey JN. Operative consideration in resection of hilar cholangiocarcinoma. HPB (Oxford) 2005; 7: 254-258.
- Uesaka K, Maeda A, Matsunaga K, Kanemoto H, Yamaguchi S. Combined resection for hilar cholangiocarcinomal. Nihon Rinsho 2006; 64: 484-487.
- Ito F, Cho CS, Rikkers LF, Weber SM. Hilar Cholangiocarcinoma: Current Management. Ann Surg 2009; 250: 210-218.
- Kobayashi A, Miwa S, Nakata T, Miyagawa S. DIsease recurrence patterns after R0 resection of hilar cholangiocarcinoma. Br J Surg 2010; 97: 56-64.
- Bismuth H, Nakache R, Dialond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg 1992; 215: 31-38.
- Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001; 234: 507-519.
- Ebata T, Nagino M, Kamiya J, Uesaka K, Nagasaka T, Nimura Y. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg 2003; 238: 720-727.
- Song SC, Choi DW, Kow AW, Choi SH, Heo JS, Kim WS. Surgical outcomes of 230 resected hilar cholangicarcinoma in a single centre. ANZ J Surg 2013; 83: 268-274.
- Dinant S, Gerhard MF, Rauws EA, Busch OR, Gouma DJ, van Gulik TM. Improved outcome of resection of hilar cholangicarcinoma (Klatskin tumor). Ann Surg Oncol 2006; 13: 872-880.
- Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci 2010; 17: 476-489.
- Li JG, Li H, Lin ZC. Combined liver, gall, pancreaticoduodenal resection and vessel reconstruction to cure hilar cholangiocarcinoma and pancreatic head carcinoma: one case report. Chin J of Biliary Surg (Chinese)2005; 11: 187.
- Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A. Combined portal vein and liver resection for carcinoma of the biliary tract. Br J Surg 1991; 78: 727-731.
- Shimada H, Endo I, Sugita M, Masunari H, Fujii Y, Tanaka K. Hepatic Resection Combined with Portal Vein or Hepatic Artery Reconstruction for Advanced Carcinoma of the Hilar Bile Duct and Gallbladder. World J Surg 2003; 27: 1137-1142.
- Chen XP, Lau WY, Huang ZY, Zhang ZW, Chen YF, Zhang WG. Extent of liver resection for hilar cholangiocarcinoma. Br J Surg 2009; 96: 1167-1175.
- Alan WH, Kristin M, Ajai K, Baquerizo A, Kim RD. Portal vein resection in management of hilar cholangiocarcinoma. J Am Coll Surg 2011; 212: 604-613.