ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 2
Assessment of recovery of endovascular stenting in patients with vertebral and basilar artery stenosis by BEAM and transcranial doppler
1Department of Cerebrovascular intervention, Cangzhou People's Hospital, Cangzhou, PR China
2Department of Neurosurgery, Xingtai people's hospital, Xingtai, PR China
3Department of Nerve Electrophysiology, Cangzhou Central Hospital, Cangzhou, PR China
4Third Department of Ultrasonography, Cangzhou Central Hospital, Cangzhou, PR China
5Department of Anatomy, Cangzhou Medical College, Cangzhou, PR China
6Otolaryngological Department, Cangzhou People's Hospital, Cangzhou, PR China
*These authors contributed equally and thus shared the corresponding authorship
- *Corresponding Author:
- Zhanqiang Wang
Department of Cerebrovascular Intervention
Cangzhou People's Hospital Cangzhou, PR China
- Jie Huang
Department of Cerebrovascular Intervention
Cangzhou People's Hospital Cangzhou, PR China
Accepted on July 25, 2016
Objective: Vertebral and basilar artery stenosis is one of the main reasons causing posterior circulation ischemia. In this study, we evaluated the effectiveness of Brain Electrical Activity Mapping (BEAM) and Transcranial Doppler (TCD) in assessing the functional improvement of the vertebral basilar artery stenosis after endovascular stenting.
Methods: Forty patients with vertebral and basilar artery stenosis treated with endovascular stenting and forty normal healthy controls between November 2010 and November 2011 were included in this study. Patients were evaluated with BEAM and TCD preoperatively and 6-months postoperatively. BEAM and TCD results of normal controls were also collected.
Results: The function improvement of patients were significantly detected by using brain electrical activity mapping and transcranial doppler.
Conclusion: Our findings showed that brain electrical activity mapping and transcranial doppler combined with digital subtraction angiography are valuable in the assessment of the function improvement of the vertebral basilar artery stenosis patients after endovascular stenting.
Keywords
Electrical activity mapping, Transcranial doppler, Artery stenosis, Endovascular stenting.
Introduction
Vertebral basilar artery stenosis is one of the major reasons that cause the Posterior Circulation Ischemia (PCI), the death rate of which can be as high as 89%. In the United States, intracranial arterial stenosis causes approximately 10% of PCI [1-5]. As indicated by previous studies [6], insufficient collateral blood supply results in a reduced perfusion pressure in the area downstream of the carotid obstruction, leading to auto regulatory dilation of cerebral arterioles. The collateral pathways consist of two parts: the anterior and posterior communicating arteries of the circle of Willis as the primary one and the ophthalmic and leptomeningeal anastomoses as the secondary one. Their activation can be associated with a reduction of cerebrovascular reserve capacity [6]. Vertebral or basilar artery is used to be treated by drug therapy, however, since 1990’s; Percutaneous Brace Implantation (PBI) has drawn a lot of attention in treating the vertebral or basilar artery. The study of Dubas revealed the relatively high safety and effectiveness of this treatment [7]. Most common techniques used to assess the degree of angiostenosis or the collateral circulation after PBI are Magnetic Resonance Angiography (MRA), Computed Tomographic Angiography (CTA), and Sphagitides Color Doppler Ultrasound (SCDU) [8,9]. However, most of these techniques have the shortcomings of high cost and complications, and are poorly popularized in primary hospitals. Some non-invasive, explicit methods are imperative.
Brain Electrical Activity Mapping (BEAM) and Transcranial Doppler (TCD) are important tests in assess the function improvement of the patient’s with vertebral or basilar artery stenosis treated with endovascular stenting, both with the advantages of non-invasiveness, high effectiveness, and low cost. The TCD is the test that measures the velocity of blood flow through the brain’s blood vessels and has been used to help the diagnosis of emboli, stenosis, and vasospasm from a subarachoid haemorrhage, and other problems [4]. The equipment request of TCD is relatively low and it is possible for a patient to travel to a hospital, doctor’s office or nursing home for both inpatient and outpatient studies. However, TCD should be in conjunction with other test such as Digital Subtraction Angiography (DSA), which is the golden standard of vertebral or basilar artery stenosis, to confirm the scanning results [9].
BEAM is the technique based on the Quantitative Electroencephalogram (qEEG) and has always been used to quantitatively detect the brain electrical activities [11,12]. This test can exhibit the activities in a certain area of brain directly, which is a significant breakthrough in the field of brain activity. Compared with CT or MRI, which can only detect the symptoms with organic lesions, BEAM reveals the abnormality in function of the brain tissue. This gives BEAM advantage in diagnosing the PCI over other tests.
In this study, both TCD and BEAM were chosen to evaluate the effect the function improvement of the patient’s with vertebral or basilar artery stenosis treated with PBI. Our results showed that TCD combined with DSA is valuable in detecting the brain blood flow before and after PBI. The change of all kinds of parameters with the improvement of brain blood shortage can be clearly identified. BEAM is also feasible for assessing patients’ brain function and the parameters change with the improvement of the brain blood input quality after the surgery. Both TCD and BEAM can be used as safe and effective methods to evaluate brain blood flow input after the PBI of vertebral or basilar artery stenosis.
Materials and Methods
Patients
A total of 40 patients with vertebral and basilar artery stenosis at Cangzhou Central Hospital between November 2010 and November 2011 were included in this study. The diagnosis of vertebral and basilar artery stenosis was determined using multi-slice spiral CTA or digital DSA of the head and neck. The patients consisted of 23 males and 17 females. The mean age of the patients was 57.5 ± 6.2 years old. Patients with heart, liver and kidney disease, other systemic disease, neuropsychic diseases, and history of trauma, surgery, and severe disease were excluded from this study. Patients who could not tolerate the DSA or PBI were also excluded. CT or MR imaging of the cervical vertebrae was conducted to exclude the possibility of vertebral and basilar artery stenosis caused by other factors such as intervertebral disc compression, osteoproliferation or transverse foramen stenosis. All patients were evaluated by TCD with DSA and BEAM before the operation and six months after the operation.
40 normal healthy subjects were selected as controls. TCD and BEAM results of these subjects were also collected.
The study was approved by local ethics committee and conducted in accordance with the declaration of Helsinki. The ethics committee approved the related screening, inspection, and data collection of the patients, and all subjects signed a written informed consent form.
DSA
DSA were conducted on a DFP-2000A angiographic unit (Toshiba, Kawasaki, Japan). The patients were placed in the supine position. After local anesthetization with 10 mL 1% lidocaine, the patient's right femoral artery was accessed using a modified Seldinger technique. A 5-French introducer sheath (Terumo Radifocus, Tokyo, Japan) was then placed within the artery. Contrast agent (containing iodine 350 mg/ml) was injected into the arcus aortae, bilateral common carotid artery, internal carotid, vertebral and basilar artery with a highpressure syringe (5 mL/sec; total, 7 mL), respectively.
TCD
Grading of stenosis was performed using type 0646 TCD Detector (DWL, Sipplingen, Germany). The patients were placed in the lateral decubitus position with the head flexed anteriorly. Attention should be paid to avoid excessive headdown position which may affect the examination results. A 2.0 MHz probe was placed at pillow window or window beside the pillow. Blood flow parameters of vertebral and basilar artery such as Systolic Velocity (Vs), Diastolic Velocity (Vd), Pulsatility Index (PI), and Resistance Index (RI) were all detected. Observations were also carried out on mode of frequency spectrum, direction of blood flow and frequency tone. The standard of diagnosis was established according to standard protocol [13].
BEAM
Three days before surgery, sedative, hormones, and vasorelaxant drugs should be forbidden in all subjects to avoid drug-induced artifact. Patients’ scalp surface lipid should be removed before examination to help to debug the electrode impedance. Additionally, patients should be instructed to exclude emotional tension, body movement, and deglutition and eye movement which may cause artifacts. The 16-channel electroencephalograph system was used (Quntian Shanghai). The 16 scalp electrodes were placed according to the standard 10-20 System. The EEG was recorded from Fp3 to 4, C3 to 4, T3 to 4, and O1 to 2 using linked earlobes as reference. Reference electrodes were placed on the left and right ear. EEG data were amplified and filtered (high pass filter 30 Hz; low pass filter 0.5) and then digitized to 12 bits at a sampling rate of 30 Hz and using an A/D converter. The EGG signals were converted into power diagram mapping which could be quantified and located. The spectrum was divided into 5 frequency bands: δ (0.5-3.9 Hz), θ (4.0-7.9 Hz), α1 (8.0-9.9 Hz), α2 (10.0-12.9 Hz), and β (13.0-30 Hz). The scale range was 32. The absolute power in each of 5 frequency bands was obtained for each monopolar lead. The mean absolute power in each band of the patient’s recording was then determined for each sampling time at 16 sites. The conditions of patients were analysed according to the research of Huang [14]. The baseline EEGs were considered abnormal if intermittent slow activity (including lateralized or generalized intermittent d activity- IDA), and persistent slow activity with or without paroxysmal epileptogenic abnormalities. The abnormal EEG patterns were divided into generalized, lateralized, and generalized with onesided dominance, if findings were prominent in one hemisphere.
Data analysis
Data analysis was performed by using SPSS 16.0 (SPSS, Chicago, IL, USA). All the data were expressed as mean ± SD. One-way ANOVA was conducted. Multiple comparisons were conducted using the LSD’s multiple range test (α=0.05). A pvalue of less than 0.05 was considered as statistically different.
Results
DSA results
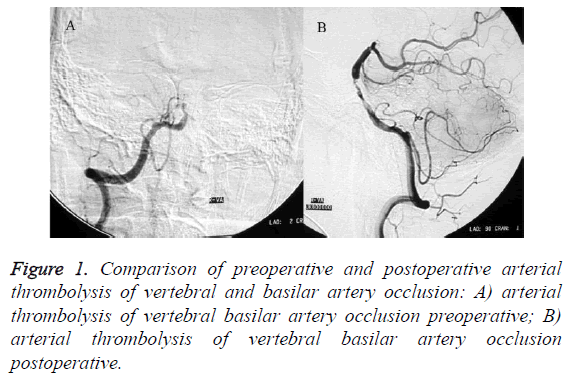
Prior to PBI, DSA examinations showed that of the all patients included in the study, there were 21 patients having basilar artery stenosis, 5 patients having bilateral vertebral artery and basilar artery stenosis, and 8 patients having unilateral vertebral artery and basilar artery stenosis. After PBI, DSA examinations showed that 20 patients achieved revascularization without any complications, 11 patients recovered presenting complications, while the remaining 3 patients died due to failure of thrombolysis. The improvement of DSA was shown in Figure 1.
TCD results
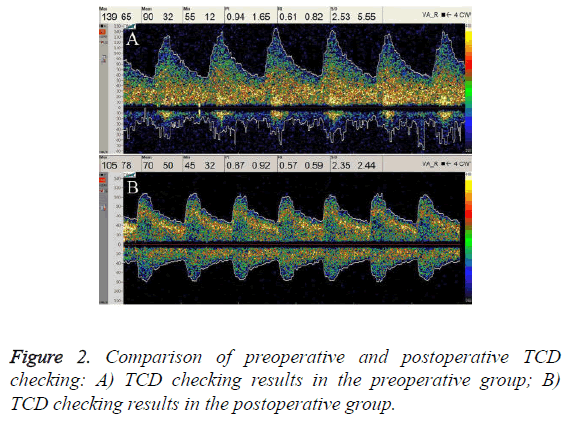
Prior to PBI, TCD results showed that patients had accelerated or decelerated peak blood flow velocity, disordered frequency spectrum, increased PI and RI compared to healthy controls. The atlas of TCD checking disordered with coarse or sharp noise. The abnormal rate of TCD examinations of the patients was 100% before surgery. Six months after PBI, patients recovered to normal blood flow parameters, blood flow frequency spectrum and sound frequency signals. The blood flow parameters regarding Vs, Vd, PI, and RI of patients with VA and BA stenosis at six months after PBI were significantly improved than that of their preoperative values as shown in Table 1. These results indicated a good improvement in the function of blood flow after PBI. Figure 2 shows the preoperative and postoperative TCD radiographs of one of the patient in this study.
| Groups | Location | Blood flow index | ||||
|---|---|---|---|---|---|---|
| Vs | Vd | PI | RI | |||
| Control group (n=40) | VA | 52.4 ± 13.3 | 22.5 ± 7.2 | 0.87 ± 0.22 | 0.57 ± 0.10 | |
| BA | 60.1 ± 11.3 | 26.8 ± 6.1 | 0.83 ± 0.21 | 0.55 ± 0.09 | ||
| Case group (n=40) | VA | Pre | 118.9 ± 27.9a | 48.1 ± 14.8a | 0.96 ± 0.26 | 0.60 ± 0.08 |
| Post | 57.4 ± 10.4b,c | 29.7 ± 5.3b,c | 0.70 ± 0.11b,c | 0.49 ± 0.05b,c | ||
| BA | Pre | 126.3 ± 31.5a | 52.7 ± 16.8a | 0.92 ± 0.24 | 0.58 ± 0.08 | |
| Post | 63.5 ± 13.0b | 31.4 ± 7.7bc | 0.74 ± 0.10b,c | 0.51 ± 0.04b,c | ||
Vs: Systolic Velocity; Vd: Diastolic Velocity; PI: Pulsatility Index; RI: Resistance Index. A:P<0.01, compared to controls; B:P<0.01, compared to preoperative values; C:P<0.01, compared to controls.
Table 1. Multiple comparisons of TCD spectrum value.
BEAM results
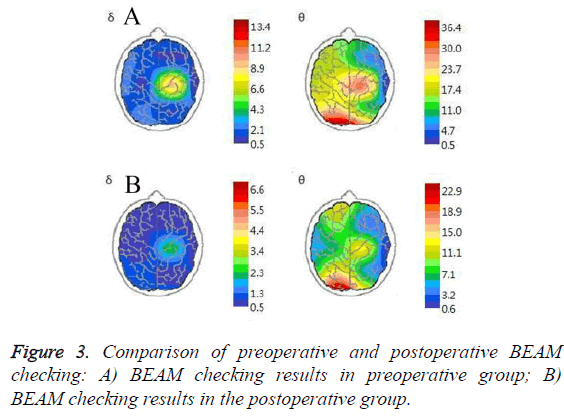
The BEAM checking showed that before PBI, the activity of α wave weakened or even disappeared and were replaced by high powered δ or θ wave as shown in Figure 3. BEAM scans showed that patients had weakened or nearly disappeared α waves before PBI which were replaced by extensive low amplitude, and low-power θ waves or δ waves and transient high-power θ waves or δ waves mainly occurring at the temporal and parietal lobes. In such a context, there exists high-power α waves (mainly α1) after PBI and the power values of previous transient θ waves or δ waves decreased. The detailed BEAM results were shown in Table 2. BEAM results showed that there were statistical significant differences between the postoperative and preoperative values with regard to the power values of α1α2θ frequency bands of the left lobulus auriculae and α1θδ frequency bands of the right lobules auriculae in the case group. When compared to the control group, the case group had statistical significant differences with regard to the preoperative power values of α1,α2, θδ frequency bands of the bilateral lobules auriculae, the postoperative power values α1 frequency bands of the left lobulus auriculae, and the postoperative power values α1 and α2 frequency bands of the right lobulus auriculae. The results suggested that BEAM could clearly reveal the changes in power values resulting from function improvement in most frequency waves.
| Location | Group | Frequency Range | ||||
|---|---|---|---|---|---|---|
| α1 | α2 | β | θ | δ | ||
| Left Side | Control group | 85.3 ± 7.9 | 84.6 ± 7.9 | 18.0 ± 4.6 | 11.4 ± 3.1 | 5.6 ± 2.0 |
| Case group Pre | 66.3 ± 20.7a | 68.0 ± 19.0a | 20.4 ± 6.2 | 22.3 ± 10.5a | 8.9 ± 3.1a | |
| Case group Post | 81.4 ± 7.6b,c | 81.4 ± 7.7b | 19.8 ± 5.0 | 10.9 ± 2.7b | 5.4 ± 1.8 | |
| Right Side | Control group | 85.1 ± 7.1 | 84.6 ± 7.9 | 18.0 ± 4.3 | 11.5 ± 3.3b | 5.8 ± 1.9 |
| Case group Pre | 62.3 ± 23.1a | 60.4 ± 19.8a | 17.0 ± 6.0 | 21.9 ± 10.1a | 7.7 ± 2.9a | |
| Case group Post | 81.9 ± 7.1b,c | 56.2 ± 31.8c | 18.7 ± 5.2 | 11.1 ± 2.6b | 5.3 ± 1.8b | |
Table 2. Multiple comparisons of the mean power among each BEAM frequency wave (μV2).
Discussion
In this study, we selected both TCD and BEAM to elucidate the changes in the function of brain blood flow in the patient with vertebral or basilar artery stenosis treated by PBI. Our results showed that TCD and BEAM have the potential to clearly reveal the function improvement in the blood flow resulting from PBI.
Vertebrobasilar arterial system consists of bilateral vertebral artery, basilar artery and other complex branches [15]. This system mainly supports the parts beneath the tentorium cerebelli, such as brainstem and cerebellum. The stenosis of the arteries in this system always results in Posterior Circulation Ischemia (PCI), which is always observed in aged people with high death rate [16-18]. The techniques used to detect the vertebral or basilar artery stenosis include MRA, CTA, SCDU, and DSA [13-14]. However, those methods have the shortcoming of invasiveness, high cost, and risk of having complications, which makes these methods inapplicable in primary hospitals. Compared with these methods, the technique adopted in the present study are non-invasive and explicit in exhibiting the function changes.
For the TCD checking, Luo et al. [19] found that the sensitivity of TCD in detecting Ischemic Cerebrovascular Disease (ICVD) was 82.3%, which was comparable to that of DA. The in the present study, the method could detect the abnormality in blood flow function before the PBI by 100%. The results of the TCD checking also clearly elucidate the difference in blood flow induces before and after PBI, moreover, the checking of patients treated with PBI had no difference compared with control groups, , which was also indicative of the potential of TCD in detecting function improvement of patients treated with PBI. However, TCD may underestimate the degree of angiostenosis, overlook the stenosis, and be unable to investigate the blood flow condition in small branches. Moreover, the results of TCD may be influenced by the thickness of skull. All the factors above make TCD should be combined with other techniques such as BEAM. In the research of Liu et al. [20], the positive rate of BEAM checking for patient with cerebral infarction was 99.8% while the positive rate of CT was only 52%. This is because BEAM can detect the function change of brain at the early stage of cerebral infarction while CT can only observe the organic lesions. In the present study, the results of BEAM checking showed that detection rate of vertebral or basilar artery stenosis before the PBI was 88.1%; after the PBI, significant different was clearly revealed compared with the values before PBI for the five wave bands. However, among the 40 patients in our study, no matter whether the stenosis was eliminated completely, the brain blood perfusion conditions and the symmetry of brain electrical actively all increased significantly,this might due to the shortage of sampling method and sampling number.
Conclusions
Both of TCD and BEAM exhibited the potential to act as convenient and inexpensive methods to detect the function improvement after PBI for patient with vertebral or basilar artery stenosis. Combined together, these two methods showed satisfactory detection rate before the PBI and were sensitive enough for the tests after the PBI. Based on our study, the checking method combing TCD and BEAM can be used in the vertebral or basilar artery stenosis and long term monitory for the patient. Further studies with a larger number of samples are warranted.
Conflict of Interest
The authors have declared no conflict of interest.
References
- Hass WK, Fields WS, North RR, Kricheff II, Chase NE, Bauer RB. Joint study of extracranial arterial occlusion II. Arteriography, techniques, sites, and complications. JAMA 1968; 203: 961-968.
- Sacco RL, Kargman D, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The northern manhattan stroke study. Stroke 1995; 26: 14-20.
- Weisberg LA. Clinical characteristics of transient ischemic attacks in black patients. Neurol 1991; 41: 1410 -1414.
- Wityk R, Lehman D, Klag M, Coresh J, Ahn H, Litt B. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke 1996; 27: 1974-1980.
- National Stroke Association. Brain attack statistics. NSA 1995.
- Reinhard M, Muller T, Guschlbauer B, Timmer J, Hetzel A. Dynamics cerebral autoregulation and collateral flow patterns in patients with severe carotid stenosis or occlusion. Ultrasound Med Biol 2003; 29: 1105-1113.
- Eberhardt O, Naegele T, Raygrotzki S, Weller M, Ernemann U. Stenting of vertebrobasilararteties in symptomatic atherosclerotic disease and acute occlusion:case series and review of the literature. J VascSurg 2006; 43: 1145-1154.
- Li SH, Li JR, Yu YH. Stent-assisted angioplasty for the treatment of vertebral-basilar artery stenosis (Translated from Chinese). Clinic Focus 2008 16: 1177-1178.
- Zhao L, Liu ZJ, Wang TT. Digital subtraction angiography and stenting for the diagnosis and treatment of vertebral and basilar artery stenosis. Clinic Focus 2006; 21: 877-879.
- Aaslid R, Markwalder TM, Nornes H. Non-invasive transcranial doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg 1982; 57: 769-774.
- Duffy FH, Hughes JR, Miranda F, Bernand P, Cook P. Status of quantitative EEG (QEEG) in clinical practice. ClinElectroencephal 1994; 25: 6-8.
- Jonkman EJ, Poortvliet DC, Veering MM, Weerd AWD, John ER. The use of neurometrics in the study of patients with cerebral ischaemia. ElectroencephalogrClinNeurophysiol 1985; 61:333-341.
- Gao S, Huang JX. Clinical application of transcranial doppler. Un Cult Un Sci 2004.
- Huang YG, Wu SL. Clinical electroencephalography 1984.
- Schneider JL, Olshaker JS. Vertigo, vertebraobasilar disease, and posterior circulation ischemic stroke.Emerg Med Clin N Am 2012; 30: 681-684.
- Amin-Hanjani S, Rose-Finnell L, Richardson D, Ruland S, Pankey D, Thulborn KR. Vertebrobasilar flow evaluation and risk of transient ischemic attack and stroke (VERiTAS) Study.Rationl DesInt J Stroke 2010; 5: 499-505.
- Gulli G,Khan S,Markus HS. Vertebrobasilar stenosis predicts high early recurrent stroke risk in posterior circulation stoke and TIA. Stroke 2009; 40: 2732-2737.
- Marquardt L, Kuker W, Chandratheva A, Geraghty O, Rothwell PM. Incidence and prognosis of > or =50% symptomatic vertebral or basilar artery stenosis:prospective population-based study. Brain 2009; 132: 982-988.
- Luo GJ, He GH, Zhang XD. Diagnostic value of transcranial doppler for intracranial artery stenosis in ischemic cerebrovascular disease. ChinJ Rehabil 2005; 217-219.
- Liu MS, Ma P, Liu QR. Contrast study on CT and BA in acute cerebrovascular diseases. J Mod Electrophysiol 2003;10: 84.