ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2017) Volume 28, Issue 1
Avascular necrosis of vertebral body with fracture of unilateral posterior facet at the level of insertion of interspinous device
Kangnam Sacred Heart Hospital, College of Medicine, Hallym University, Korea
- *Corresponding Author:
- Kook Jin Chung
Kangnam Sacred Heart Hospital
College of Medicine
Hallym University
Korea
Accepted date: May 25, 2016
This report shows a rare case of avascular necrosis of vertebra body after insertion of interspinous device after insertion of interspinous device and its plausible cause. A 82-year-old woman presented with severe back pain for 1 week without injury. In her history, she had undergone decompression and implantation of L4-5 interspinous device for the relief of neurogenic claudication at 4 year ago. Magnetic resonance image demonstrated signal change suggesting avascular necrosis of L5 vertebra body and fracture of posterior facet after insertion of interspinous device. In this case, avascular necrosis of lumbar vertebra body was documented with simple radiograph and MRI and symptom was satisfactorily relieved with conservative treatment. Avascular necrosis of lumbar vertebra body can occur as a complication of interspinous process device. Surgeons always must consider the possibility of avascular necrosis of vertebral body in patients with osteoporosis after insertion of interspinous device.
Keywords
Avascular necrosis, Fracture, Posterior facet, Lumbar vertebra, Interspinous device
Introduction
Avascular necrosis (AVN) is not a common disease in musculoskeletal system. In 1895, Kummell disease represents a failure of the fracture healing process, for which there are no good non-operative treatments [1]. AVN of vertebra is usually considered as the result of non-union due to poor blood supply after vertebral compression fracture and is thought to be the consequence of an insult to anterior segment of vertebral body, with either traumatic or non-traumatic mechanism. Avascular necrosis of vertebral body may occur from medical diseases such as Gaucher disease, sickle cell anaemia and radiation therapy, chemotherapy and steroid use. Although several cases of avascular necrosis of vertebral body have been reported followed by minimally invasive spine surgery, but as far as we know, there have been no reports documenting avascular necrosis of vertebral body at the level of insertion of interspinous device. Therefore we describe a case of avascular necrosis of lumbar vertebral body after insertion of interspinous device without injury.
Case Report
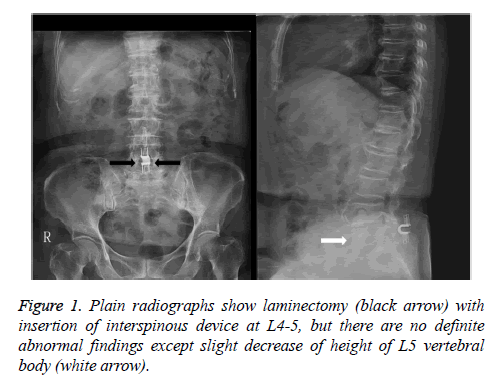
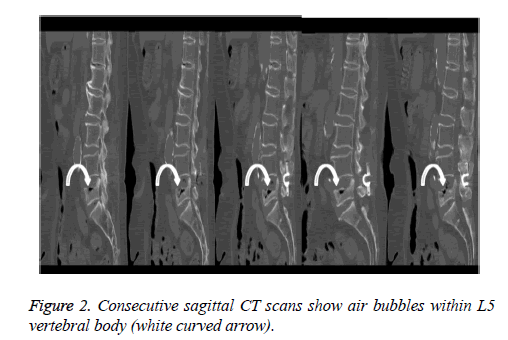
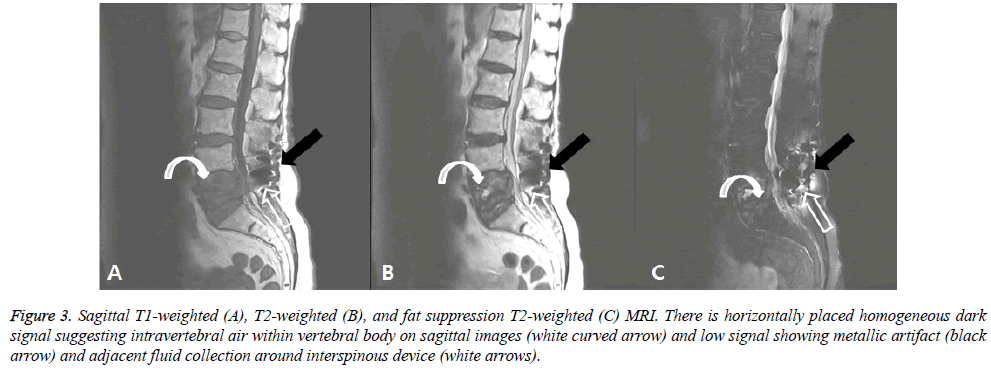
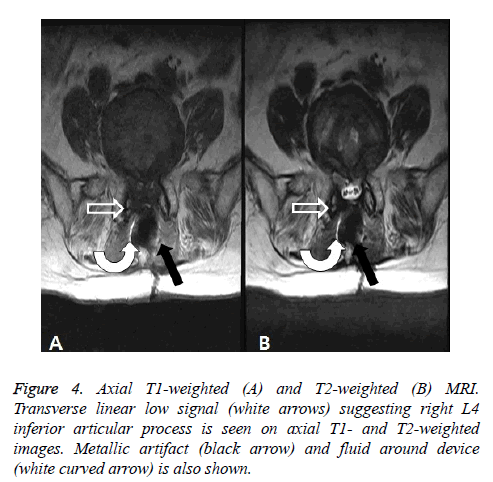
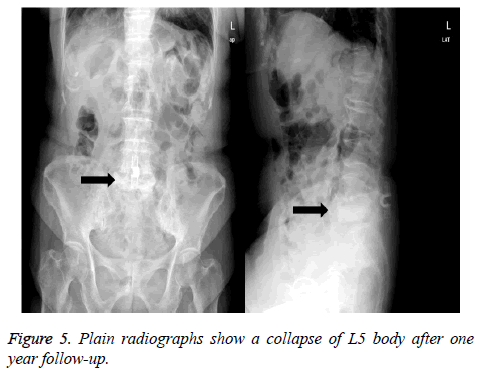
A 82-year-postmenopausal woman presented with sudden onset of severe low back pain for a week. In her history, she was diagnosed as spinal stenosis at L4-L5 10 years ago and she got an operation with decompressive laminectomy with instrumentation of interspinous device for the relief of neurogenic claudication at other clinic. After operation, she was satisfied with surgical result and performed activity of daily living without any restriction. 4 years later after operation, she visited our hospital complaining of severe back pain aggravated by movement without radiating pain and claudication There was no past history of recent trauma, systemic medical illness, steroid use, radiation therapy and chemotherapy without except medication of antihypertensive agents. She was not able to walk and even to move on the bed without support. Plain radiographs showed implantation of interspinous device at L4-5 with laminectomy and slight decrease of height of body of 5th lumbar vertebra (Figure 1). Computed tomography (CT) showed intravetebral vacuum cleft on body of L5 (Figure 2). On Magnetic resonance imaging (MRI), intravertebral air revealing signal intensity void was found on both T1- and T2- weighted images. Intravertebral fluid showed low signal intensity on T1- weighted images and high signal intensity on T2-weighted images (Figure 3). Besides these findings of avascular necrosis of L5 body, transverse linear low signals suggesting fracture of inferior articular process of L4 are found on axial scans of T1 and T2-weighted images (Figure 4). Metastatic work-up did not reveal any abnormal findings. We recommended surgical treatments but patient and their family did not want surgical treatment. Right after admission, she could not move on the bed and not change body position by herslef. With orthosis and medication, physical therapy, back pain was relieved gradually and then she moved and got out of the bed and walked without any support 2 weeks later. Vertebral collapse of L5 was shown on plain radiographs at 1 year after diagnosis (Figure 5) and now she spent daily life complaining of moderate back pain controlled with analgesics without severe disability.
Figure 3: Sagittal T1-weighted (A), T2-weighted (B), and fat suppression T2-weighted (C) MRI. There is horizontally placed homogeneous dark signal suggesting intravertebral air within vertebral body on sagittal images (white curved arrow) and low signal showing metallic artifact (black arrow) and adjacent fluid collection around interspinous device (white arrows).
Discussion
AVN is often found in scaphoid, talus, head of femur, where blood supply of end artery is disrupted. But, AVN of the vertebral body is not common and most likely associated with abundant blood supply [2]. Delayed post-traumatic vertebral collapse, the mechanism of AVN of vertebral body, proposed by Kummell is that the nutritional status of the affected vertebral body is injured by the minor trauma, so that resorption of the vertebra occurs resulting in a late collapse [1]. The collapse usually occurs at the junction of anterior one-third and posterior two-thirds which was confirmed by angiographic study that shows a watershed area of circulation [3]. The patients with AVN of vertebral body usually middle aged or elderly men or women and the lower thoracic and upper lumbar vertebral bodies mostly involved [4]. Single vertebra or rarely, multiple vertebrae are involved and the interval between acute trauma and vertebral collapse can vary from days to years [5]. In this case, patient had no history of recent trauma without operation with decompressive surgery using interspinous device for the symptomatic relief of spinal stenosis 4 years ago. Interspinous device had the advantage that it helps to lessen buckling of soft tissue, narrowing of spinal canal. Also it decreases facet loading and unloads the intervertebral discs at the instrumented level [6] and does not change kinematics of the motion segments adjacent to the instrumented level. Lindsey et al. [7] reported that the range of motion on flexion and extension was significantly reduced at the instrumented level. There have been many reports about load transmission of posterior facet joints. Nachemson [8] reported that the removal of arches and joint processes increases the intradiscal pressure on the average by 18% through experimental studies using post-mortem materials. According to the experimental study by Schendel et al. [9] 5 to 8% compressive axial load was transferred to posterior facet. But, if arthritis occurs on the facet joint, the load could be increased as high as 47% [10].
A few cases of AVN of lumbar vertebral body have been reported after minimally invasive spine surgery such as intradiscal electrothermal therapy and percutaneous laser discectomy [11,12] and even idiopathic [13]. It is not easy to confirm the exact etiology and time of onset in every case of AVN of vertebral body. Also we first reported the stress fractures of bilateral posterior facets after the insertion of interspinous implant [14]. On the current study, it is not clear whether the interspinous device affects the occurrence of AVN of lumbar vertebral body and unilateral fracture of inferior articular facet. Based on the results by Lindsey et al., we hypothesized that range of motion of posterior facet was reduced after the insertion of interspinous device and arthritic change of facet joint with repetitive loading was aggravated and finally fracture of facet occurred. Involuntary movements to reduce pain caused by facet fracture may make vertebra body loaded and cause avascular necrosis. In this respect, we suggest that treatment with interspinous device must be prudent especially in geriatric patients. There have been no long term results following the insertion of interspinous device. Further studies will be needed about the biomechanical changes of vertebral body, intervertebral disc and facet joints after insertion of interspinous device. But, this report is didactic and helpful to the surgeons who consider the insertion of interspinous device to the patients with osteoporosis.
References
- McKiernan F, Facszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum 2003; 48: 1414-9.
- Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ. Vertebral osteonecrosis: MR imaging findings and related changes on adjacent levels. Am J Neuroradiol 2007; 28: 42-47.
- Stojanovic J, Kovac V. Diagnosis of ischemic vertebral collapse using selective spinal angiography. Rofo 1981; 135: 23-29.
- Huang SL, Shio W, He XJ. Avascular necrosis of a vertebral body. Chin J Traumatol 2009; 12: 125-8.
- Resnick D, Niwayama G. Ostepnecrosis: diagnostic techniques, specific sites and complications. Philadelphia; Saunders, 1995: 3496-3558.
- Swanson KE, Lindsey DP, Hsu KY. The effects of an interspinous implant on intervertebral disc pressures. Spine (Phila Pa 1976) 2003; 28: 26-32.
- Lindsey DP, Swanson KE, Fuchs P. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine (Phila Pa 1976) 2003; 28: 2192-7
- Nachemson A. Lumbar intradiscal pressure. Experimental studies on post-mortem material. Acta Orthop Scand Suppl 1960: 43; 1-104.
- Shendel MJ, Wood KB, Buttermann GR, Lewis JL, Ogilvie JW. Experimental measurement of ligament force, facet force and segment motion in human lumbar spine. J Biomech 1993; 26: 427-38.
- Yang KH, King AI. Mechanism of facet laod transmission as a hypothesis for low-back pain. Spine (Phila Pa 1976) 1984; 9: 557-65.
- Scholl BM, Theiss SM, Lopez-Ben R, Kraft M. Vertebral osteonecrosis related to intradiscal electrothermal therapy: a case report. Spine (Phila Pa 1976) 2003; 28: E161- E164.
- Tonami H, Kuginuki M, Kuginuki Y, Matoba M, Yokota H, Higashi K, Yamamoto I, Nishijima Y. MR imaging of subchondral osteonecrosis of the vertebral body after percutaneous laser discectomy. Am J Roentgenol 1999; 173: 1383-1386.
- Chou LH, Knight RQ. Idiopathic avascular necrosis of a vertebral body. Case report and literature review. Spine (Phila Pa 1976) 1997; 22: 1928-1932.
- Chung KJ, Hwang YS, Koh SH. Stress fracture of bilateral posterior facet after insertion of interspinous implant. Spine (Phila Pa 1976) 2009; 34: E380-383.