ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2007) Volume 18, Issue 3
Case Report: Pre-rupture ultrasound diagnosis of rudimentary horn pregnancy
Papa Dasari*
Department of Obstetrics and Gynaecology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry605 006, India
- Corresponding Author:
- Papa Dasari
Department of Obstetrics & Gynaecology
JIPMER, Pondicherry 605 006, India
Phone: +91-413-241715
FAX: +91-413-372067
e-mail: pdasari ( at ) jipmer.edu
Accepted date: July 25 2007
An young primigravida with initial diagnosis of threatened abortion was diagnosed as missed abortion by USG was planned to terminate pregnancy by extra-amniotic prostadin. As there was difficulty in negotiation of catheter in to the uterus the case was reexamined clinically and was suspected to be rudimentary horn pregnancy which was confirmed by TAS. The findings on repeat USG showed the myometrium of the pregnant horn to be <2mm in thickness and defective at some places suggesting threatening rupture which helped in deciding the case for immediate lapratomy. One should have high index of suspicion in diagnosing rudimentary horn pregnancies and whenever there is difficulty while performing termination of pregnancy surgically, the case should be re-evaluated clinically as well as Ultrasonographically.
Keywords
Missed abortion, Extra-amniotic prostadin, Rudimentary horn pregnancy.
Abstract
An young primigravida with initial diagnosis of threatened abortion was diagnosed as missed abortion by USG was planned to terminate pregnancy by extra-amniotic prostadin. As there was difficulty in negotiation of catheter in to the uterus the case was reexamined clinically and was suspected to be rudimentary horn pregnancy which was confirmed by TAS. The findings on repeat USG showed the myometrium of the pregnant horn to be <2mm in thickness and defective at some places suggesting threatening rupture which helped in deciding the case for immediate lapratomy. One should have high index of suspicion in diagnosing rudimentary horn pregnancies and whenever there is difficulty while performing termination of pregnancy surgically, the case should be re-evaluated clinically as well as Ultrasonographically.
Introduction
Rudimentary horn pregnancy is a rare form of ectopic pregnancy, most of the cases were being diagnosed at laparotomy for haemorrhagic shock or after autopsy for maternal death. Mortality is high as in 90% of the cases, death occurs within 10 to 15 minutes of the onset of symptoms due to massive intraperitoneal haemorrhage [1]. Pre-operative diagnosis was reported only in 5% of the cases [2]. Although the diagnosis prior to rupture is difficult, early detection is essential to avoid a fatal outcome [3]. USG plays an important role in early diagnosis and management.
Case
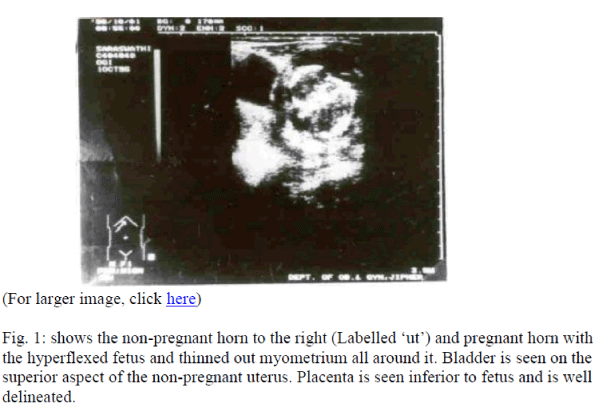
A 20 year old primigravida married since one year presented to our Obstetric Out-patient Department with complaints of irregular bleeding per vaginum of 2 months duration and lower abdominal pain of 3 days duration following 4 months amenorrhea. She was not sure of her last menstrual period but her cycles were regular with average flow. On examination, she had mild pallor with a pulse rate of 82/min and a BP of 110/80 mm Hg. Abdominal examination revealed a 14 week size midline nontender mass arising out of pelvis. Per speculum examination showed altered blood at external os. On per vaginal examination, 14 week soft uterus deviated to left side was felt and right fornix was tender. The case was diagnosed as threatened abortion clinically and an USG performed on the next day reported findings suggestive of intrauterine fetal death. Extra-amniotic prostaglandin injection was planned to induce abortion and Foley’s catheter could not be negotiated inspite of repeated attempts by two different clinicians. Her Hb was 12 gm. bleeding and lotting time within normal limits, blood group RH was O positive. The patient complained of increased pain abdomen and after 48 hours of admission. Her pulse was 96/min, regular, BP was stable. Abdominal examination showed a suprapubic tender mass of 14-week size. Shifting dullness was negative, per vaginal examination revealed cervix movements to be tender and a tensely cystic mass of 10×10 cm was felt through left and anterior fornix. A groove was felt between the mass and cervix. The body of the uterus was felt to the right and posterior side of the mass. With the above clinical findings, rudimentary horn pregnancy was suspected and a TAS performed showed the following findings, viz. normal size uterus with en-dometrial lining to the right of the midline; gestational sac with fetus was seen on the left. Fetus was hyperflexed with biometry corresponding to 13 weeks gestation and fetal cardiac activity was absent. Placenta was inferior to fetus and in close continuity with a thinned out uterine musculature. The myometrium is less than 2 mm in thickness and incomplete at some places (Fig.1).
Laparotomy revealed right-sided normal uterus, tube and ovary. The left side had a rudimentary horn with pregnancy with a thick fibrous band of tissue attaching it to the right horn. Left tube and ovary were attached to the rudimentary horn near fundocornual region. Both kidneys and ureters were normal. Excision of left rudimentary horn (hemihysterectomy) with left partial salphingectomy was carried out. The histopathological examination revealed evidence of haemorrhage into uterine musculature.
Discussion
The incidence of rudimentary horn pregnancy is reported to be 1 in 140,000 deliveries, 89% rupture and 11% proceed to term [4]. The rupture usually occurs during the late first trimester or early second trimester to cause massive intraperitoneal haemorrhage resulting in high maternal morbidity and mortality [3,5]. Haemorrhage is severe and more profuse than in tubal pregnancies because the horn is more thicker and vascular than the fallopian tube [6]. Clinically, no definite signs were reported by which a rudimentary horn pregnancy could be differentiated from that of a normal intrauterine pregnancy. But finding of a pelvic mass during pregnancy should lead to suspicion of rudimentary horn pregnancy [5].
In 1983, Holden and Hart [6] reported the first case of pre-rupture USG diagnosis of rudimentary horn pregnancy where the placental delineation by the thinned out uterine wall helped in diagnosis. They suggested that this feature helps in differentiating it from abdominal pregnancy in which placental delineation is difficult because of the lack of intact chorionic plate and also due to multiple areas of implantation and adhesions with overlying bowel loops. Rudimentary horn pregnancy should also be suspected whenever placenta acreeta was diagnosed by USG as there is a high incidence (13.7%) of this condition associated with rudimentary horn pregnancies [7]. Assessment of myometrial thickness is one of the criteria used to diagnose the prerupture status of rudimentary horn pregnancy as suggested by Gagnon et al [8]. A myometrial thickness of <5 mm was observed by them in prerupture state and this has increased to 9.5 mm after amniodecompression employed to prevent the rupture.
In case, the diagnosis is missed, failure to terminate the pregnancy by extraamniotic injection can be a clue as experienced in this case and by Liang et al [5]. Artificial abortion failed in five cases reported by Guo [9]. Noncommunicating rudimentary horn should be suspected whenever difficulty is encountered during termination of pregnancy as it is easy to miss this condition both clinically and by USG.
Conclusion
Rudimentary horn pregnancy should be suspected whenever difficulty is experienced while terminating a pregnancy and every attempt should be made to rule out the same. Ultrasonography plays an important role in diagnosing rudimentary horn pregnancy especially in pre-rupture state.
References
- De Nicola RR, Peterson MR. Pregnancy in rudimentary horn of uterus. Am J Surg 1947; 73: 381-82.
- Chang JC, Lin YC. Rupture of rudimentary horn pregnancy. Acta Obstet Gynaecol Scand 1992; 71: 236-238.
- Chang WF, Lin HH. Ultrasound diagnosis of rudimentary horn pregnancy in fourteen weeks of gestation: a case report. Ascia-Oceania J Obstet Gynaecol 1994; 20: 279-282.
- O’Leary JL, O’Leary JA. Rudimentary horn pregnancy. Obstet Gynecol 1963; 22: 371-375.
- Liang ST, Woo JSK, Tang LCH, Wong RLC. Advanced pregnancy in the rudimentary horn of a bicornuate uterus. Acta Obstet Gynecol Scand 1985; 64: 447-449.
- Holden R, Hart P. First trimester rudimentary horn pregnancy. Prerupture ultrasound diagnosis. Obstet Gynecol 1983; 61: 565-585.
- Basbug M, Soyller I, Aygen E. Placenta accreta associated with rupture of a rudimentary horn pregnancy Int J Gynaecol Obstet 1997; 57: 199-201.
- Gagnon AL, France G, Williams K. Twin pregnancy with one fetus in a rudimentary horn: a case report of a surviving twin. Br J Obstet Gynaecol 1998; 105: 1326-1328.
- Guo YX. Diagnosis and treatment of rudimentary uterine horn complicating pregnancy. Chinese J Obstet Gynecol 1991; 26: 31-2, 61-62.