ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2015) Volume 26, Issue 3
Changes in serum cytokine levels in hand-foot-and-mouth disease.
3rd Department of Infectious Disease, Beijing You’an Hospital, Capital Medical University, Beijing 100069, China
- *Corresponding Author:
- Tong-Zeng Li
3rd Department of Infectious Disease
Beijing You’an Hospital, Capital Medical University
No. 8 Youanmei West Road Fengtai District
Beijing 100069, China
Accepted date: March 27 2015
The aim of this study was to investigate changes in serum cytokine levels in children with handfoot- and-mouth disease (HFMD) and their clinical significance. Clinical data from 241 children with HFMD, hospitalized between May 2012 and January 2013, were analyzed retrospectively. Patients were divided into a normal case group (n=107) and a severe case group (n=134), and the clinical features of the children were summarized. Concurrently, a etiological examination was performed, and the levels of 5 cytokines were measured: interleukin (IL)-2, IL-6, IL-10, tumor necrosis factor (TNF)-α, and interferon (IFN)-γ. There was no significant difference in the age, sex ratio, length of hospital stay, and the highest temperature between groups. IL-2, IL- 6, IL-10, and TNF-α levels were significantly higher (P<0.05) in the severe case group than in the normal case group; however, there was no significant difference in IFN-γ levels between the 2 groups. Elevated cytokine levels measured in severe cases of HFMD, suggesting that cytokinerelated inflammation and anti-inflammatory responses might be involved in the development of severe HFMD.
Keywords
Hand-foot-mouth disease, cytokines, clinical analysis
Introduction
Hand-foot-and-mouth disease (HFMD) is a common, acute infectious disease caused by enterovirus, which is spread via the digestive tract and the respiratory tract, and often occurs in children under 5 years old. The prognosis is good in most cases; however, complications seen in severe cases include encephalitis, encephalomyelitis, pulmonary edema, circulatory failure, and death. Severe cases are primarily seen in children under 3 years old. The main pathogens causing HFMD are enterovirus 71 (EV71) and coxsackievirus A16 (CA16), with the more severe cases primarily associated with EV71. In these cases, the main cause of death is brain stem encephalitis and neurogenic pulmonary edema (NPE). NPE or pulmonary hemorrhage occurs because of stimulation of the central α-adrenergic receptors, causing vasoconstriction in the systemic circulation, resulting in blood entering the pulmonary circulation in a short period of time and causing pulmonary edema or pulmonary hemorrhage. In addition, studies indicate that abnormal increases in levels of cytokines such as IL-6, IL-10, IL-13, TNF-α, and IFN-γ and lymphocyte depletion are involved in the immunopathological pathogenesis of pulmonary edema [1,2]. The cellular immune status of infected patients is also closely related to the clinical prognosis of HFMD [3]. Recent studies have determined that immune function, particularly cytokine levels, plays an important role in the progressionof diseases. Complications seen in severe cases are often associated with abnormal cytokine levels, activated by a viral infection, resulting in such relevant clinical manifestations as severe systemic inflammatory response, brain stem injury, and increased pulmonary vascular permeability [4]. There has been some research on cytokine levels in HFMD cases in China. We analyzed clinical data from 241 children diagnosed with HFMD, admitted to our hospital between May 2012 and January 2013, to determine changes in serum cytokine levels associated with HFMD.
Subjects and Methods
General Information
We enrolled 241 children, clinically diagnosed with HFMD, admitted into our hospital between May 2012 and January 2013. Of these, 146 were male (60.6%) and 95 were female (39.4%), aged from 2 months to 9 years, with the average age of 25.6±18.7 months. Of these, 205 patients (85.1%) were children under 3 years old.
All 241 patients presented with a fever and rash, specific symptoms of the nervous system were poor spirit, lethargy, easily frightened, headache, vomiting, delirium, coma, limb shaking, myoclonus, nystagmus, ataxia, and eye movement disorders. Physical examination revealed positive pathological symptoms such as meningeal irritation, and a weak or disappearing tendon reflex.
Methods
Patients were divided into two groups, the normal case group (NC, n=107) and the severe case group (SC, n=134), following guidelines described in "A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD)" issued by the World Health Organization and the Regional Emerging Diseases Intervention Centre in 2011 [5].
General information and cytokine levels were compared between the 2 groups. The Luminex Liquid Chip Adoption Bio-Plex Human 8-plex cytokine assay kit (Bio-Rad, Hercules, CA, USA) was used to measure the levels of 5 cytokines: IL-2, IL-6, IL-10, TNF-α, and IFN-γ.
Statistical Analysis
Data were analyzed using SPSS version 17.0 statistical software. Normally distributed data are presented as mean ± SD, and non-normally distributed data are presented as the median (interquartile range, IQR); the χ2 test was used for intergroup comparison of count data; normally distributed data were compared using the independent sample t-test, while the non-normally distributed data were compared using the Mann-Whitney U test; all tests were two-sided, with the significance level set at P<0.05.
Results
Clinical Characteristics
All 241 cases presented with rash and fever, the fever generally appeared 3 days before rash and had a duration of 5 to 7 days; the average maximum body temperature was 39.1±0.7 °C. Of the 241 cases admitted, 107 cases were in the NC group (44.4%) and 134 cases were in the SC group (55.6%). SC group cases presented with symptoms such as meningitis, encephalitis, encephalomyelitis, pulmonary edema, and circulatory disorders following the initial onset of HFMD [1]. Of the 134 severe cases, there were 112 cases of hyperarousal and/or limb shaking (83.6%), 83 cases of headache and/or vomiting (61.9%), 32 cases of listlessness and/or lethargy (23.8%), 13 cases of amyosthenia (9.7%), 15 cases of convulsion (11.2%), 11 cases of restlessness (8.2%), 5 cases of staring (3.7%), and 1 case of coma (0.7%). Among all cases, 240 were cured/the symptoms improved and the patients were discharged, and 1 patient died (0.4%).
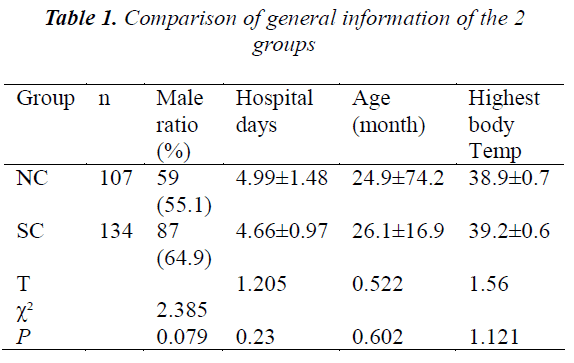
There was no significant difference in any of the general information categories, gender, age, length of hospital stay, or the highest body temperature, between the normal and severe group (Table 1).
Laboratory Examination
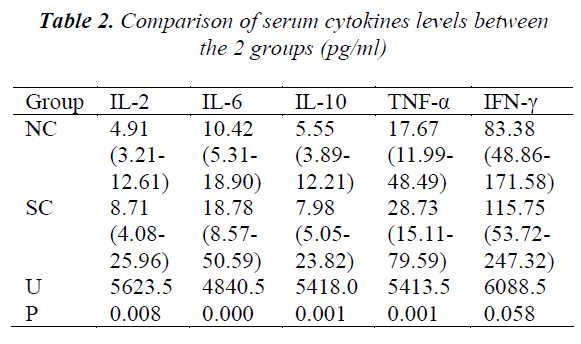
There was a significant difference in levels of IL-2, IL-6, IL-10, and TNF-α between the 2 groups. There was, however, no significant difference in the levels of IFN-γ between the 2 groups (Table 2).
Discussion
HFMD is primarily caused by a viral infection, including EV71, CoxA, and echovirus (Echo), of which EV71 is the most common. EV71 is a highly neurotropic virus that can cause an imbalance of vasoactive substances, cytokines, and other substances, producing a series of nervous system-related syndromes, which in some individuals can become critical, and even life threatening, because of the involvement of heart and lung functions. The mechanism involved is not completely clear; however, the role of cytokines in its pathogenesis has attracted much attention. Lin found that patients with EV71 infection-related neurogenic pulmonary edema showed hypercytokinemia, with levels of nervous system cytokines also significantly increased, and the symptoms exhibited were related to the presence of large numbers of inflammatory cytokines [4]. It has been shown that the interactions between proinflammatory and anti-inflammatory cytokines play an important role in the process of HFMD, and that systemic inflammatory response syndromes are an important factor in the development of critical conditions [6]. Our study retrospectively analyzed the data of 241 children diagnosed with normal or severe cases of HFMD. While there were no significant differences in gender, age, the highest temperature, and the length of hospital stay between the groups, there was a significant difference in levels of IL- 2, IL-6, IL-10, and TNF-α. There was, however, no significant difference in IFN-γ levels between the 2 groups.
TNF-a and IL-6 are produced by activated monocytesmacrophages. They are cytokines capable of regulating immune response, and important mediators of immune protection; however, under certain conditions they may also be involved in autoimmune responses. Under normal circumstances, serum concentrations of TNF-a and IL-6 are low, and they are involved with in physiological processes such as regulating responses and promoting cell growth and differentiation. When a bacterial or viral infection occurs, the monocytes-macrophages produce and release large amounts of cytokines, among which TNF-a is the first multifunctional factor produced, mediating many pathophysiological processes of the inflammatory response. TNF-a acts primarily on the vascular endothelial cells to promote adhesion, migration, and invasion of the inflammation cells, and the degranulation of neutrophilic granulocytes. Concurrently, it may act on the monocyte-macrophage cell itself to release inflammatory mediators, thereby exacerbating the inflammatory response, and causing a local immune response and even system damage. Previous studies have reported that HFMD patients, with combined nervous dysfunction or pulmonary edema, had significantly increased levels of IL-6 and TNF-a [7]. Lin stated that IL-6 and TNF-a levels were significantly higher in HFMD patients with pulmonary edema than in patients without those complications. In addition, IL-6 can further intensify the biological activities of IL-1ß and TNF-a, and IL-6 levels >70 pg/ml are the best predictors of EV71-related-encephalitisinduced pulmonary edema [4].
Levels of IL-6 and TNF-a are also increased in the cerebrospinal fluid (CSF) of HFMD patients, especially in patients infected with EV71 infection complicated with encephalitis and pulmonary edema [2]. In the present study, we found that the TNF-a levels in the SC group were significantly higher than the NC group, suggesting that TNF-a may be involved in the pathological progression of HFMD. Excessive TNF-a levels may cause, and increase, tissue damage in the central nervous system, providing an early detection method for severe cases, and guiding the therapy and recovery.
Our study found that the serum levels of IL-6 in the SC group were significantly higher than the NC group, suggesting that IL-6 might play a specific role in the progression of HFMD. After viral infection, the dendritic cells of HFMD patients release large amounts of IL-6. IL-6 is a cytokine with wide range of biological activities, includingregulation of cell growth and differentiation in various tissues. Being the major regulator of the inflammation reaction, IL-6 is involved in biological processes such as vascular inflammation, immune response, hematopoiesis, and tumor progression. Constituting the complex cytokine network together with other factors, IL-6 is able to adjust the immune and stress response, and is closely associated with the pathological changes of many clinical diseases. In infectious diseases, the release of IL-6 helps fight the infection; animal experiments have shown that IL-6 reduces the viral load of EV71 in mice [8], but in the course of infection and inflammation, IL-6 delays the phagocytosis of phagocytic cells towards the aged and dysfunctional neutrophilic granulocytes, thus exacerbating the generation of the inflammatory mediators. The large release of IL-6 is a dangerous sign of infection, experiments have shown that 3-6 days after infection with EV71, anti-IL-6 given to neutralize the antibodies improved the prognosis of experimental animals without decreasing viral load [9]. This suggests that lowering serum IL-6 levels may improve the prognosis of patients with severe cases of HFMD.
IL-10 is an anti-inflammatory cytokine with multiple effects. Its primary biological activities are immune inhibition: inhibiting the synthesis of pro-inflammatory cytokines and chemokines by monocytes and neutrophils, inhibiting the releasing of IL-6 and TNF-a, inhibiting antigen- stimulated cellular immune response, and delaying the apoptosis of T cells and B cells. Studies have shown that IL-10 is closely related to the release of catecholamines [10]. We found that following HFMD infection, along with a massive release of the inflammatory factors and inflammatory inhibitors, IL-10 levels in the SC group were significantly higher than those in the NC group. Whether IL-10 levels are decreased in HFMD patients accompanied with cardiopulmonary dysfunction still requires further study.
IFN-γ is primarily produced by CD4+T lymphocytes, cytotoxic CD8+T lymphocytes, and natural killer cells, and plays an important role in both inherent immunity and acquired immunity. IFN-γ may reduce the endothelial barrier and increase the vascular permeability, leading to pulmonary edema and pulmonary hemorrhage. Previous studies have shown that serum IFN-γ levels in patients with HFMD combined with brainstem encephalitis or pulmonary edema are significantly increased compared to normal HFMD patients. Similar conclusions have been reached in CSF studies [11]. Our study, however, did not reveal a significant difference in IFN-γ levels between SC and NC patients, which may have been because few patients in our study had HFMD accompanied with severe pulmonary edema and pulmonary hemorrhage. Increased IFN-γ levels could have been more obvious in children with HFMD accompanied with pulmonary edema and pulmonary hemorrhage, suggesting that more cases are required in future studies.
Abnormal levels of cytokines also exist in enteroviral meningitis. Studies have shown that in the acute phase of the disease, when the CSF contains viral gene fragments, IL-6, IL-8, and IFN-γ levels in the CSF are significantly increased. Levels subsequently return to normal during the recovery period, when the virus is undetectable, and levels of the anti-inflammatory cytokine IL-10 are increased. In the acute phase, the increasing cytokine levels in the CSF manifest earlier than the increase in leukocytes [12], showing that there exists an interaction of proinflammatory and anti-inflammatory cytokines in the enteroviral central nervous system infection. Another study found that after EV71 infection, IL-6 levels gradually increase with the exacerbation, and that IL-6 levels in CSF are higher than in plasma. This suggests that IL-6 is a major factor in promoting the exacerbation [13].
Because abnormal cytokine levels may be a risk factor leading to the exacerbation, it is implied that levels of cytokines may be adjusted to improve the prognosis of infected patients. Studies involving animals infected with the H5N1 virus confirm that immunomodulatory therapy can indeed reduce the levels of inflammatory factors, in vivo, and improve prognosis [14]. Currently, severe HFMD cases are primarily treated with intravenous human immunoglobulin (IVIG), a polyclonal immunoglobulin collected from human blood that is used to treat a variety of serious viral infections. However, the mechanism by which IVIG works may interfere with the Fc receptor, induce apoptosis, and interfere with the inflammatory process of cytokines [15]. IVIG may also reduce plasma catecholamine levels, realizing the effects of myocardial protection [16]. In 2013, a study involving avian influenza H7N9-infected critically ill patients in China determined that increased cytokine levels, for example, IL-6, was one of the factors leading to the critical condition of the patients, and that plasma exchange reduced the levels of cytokines, thereby improving the prognosis [17]. This provides new thinking in the treatment of the "cytokine storm" associated with critically ill patients following viral infection.
In addition to abnormal levels of cytokines, researchers have summarized other risk factors that could be used for prognostic prediction. A prospective study found that the occurrence of 2 of 3 criteria: peak body temperature greater than 38.5°C, fever lasting longer than 3 days, or drowsiness, may indicate that nervous system involvement might occur [18]. A retrospective study from Singapore suggested that vomiting, absence mouth sores, and increased serum leukocytosis were risk factors for critical conditions [19]. A Korean retrospective study also suggested that a fever over 4 days, a body temperature peak greater than 39.0°C, headache, vomiting and neurological symptoms, and blood sugar >100 mg/dl were the risk factors for the occurrence of neurological complications [20]. In addition, heart rate variability index was considered to be an effective predictor, which would decrease significantly 7 hours before the heart failure; the sensitivity and specificity of the diagnosis of HFMD accompanied with encephalitis, heart and lung dysfunction, and circulatory dysfunction were 100% and 71.4%, respectively [21]. Another study found that HFMD cases resulting in death, presented with non-ischemic myocardial damage and the reduced ejection fraction. The myocardial damage in the children was caused by an increase in serum troponin I, which could be used as a predictor for poor prognosis [22]. The above factors and cytokine levels taken together constitute the most common indicators predicting the prognosis of clinically severe HFMD cases.
In conclusion, our study found that the levels of cytokines IL-6, IL-10, and TNF-a were significantly higher in patients with severe HFMD compared to normal cases. These findings imply that these factors may be involved in the worsening of the disease, suggesting that further studies are required to determine the role of cytokines in disease progression, and to further examine the regulation of cytokine levels in critically ill patients to improve prognosis. Severe HFMD cases combined with heart and lung failure were few; therefore, future studies with a larger sample size are required to deepen our knowledge, in order to improve the diagnosis of HFMD.
Conflicts of interest
All of the authors declare that they have no conflicts of interest regarding this paper
References
- Lin TY, Chang LY, Huang YC, Hsu KH, Chiu CH,Yang KD. Different proinflammatory reactions in fatal and non-fatal enterovims71 infections: implications for early recognition and therapy. ActaPaediatr 2002; 91: 632-635.
- Wang SM, Lei HY, Huang KJ, Wu JM, Wang JR, Yu CK, Su IJ, Liu CC. Pathogenesis of enterovirus 71 brainstem encephalitis in pediatric patients: roles of cytokines and cellular immune activation in patients with pulmonary edema. J Infect Dis 2003; 188: 564-570.
- Chang LY, Hsiung CA, Lu CY, Lin TY, Huang FY, Lai YH, Chiang YP, Chiang BL, Lee CY, Huang LM. Status of cellular rather thanhumoral immunity is correlated with clinical outcome of enterovirus 71. Pediatr Res 2006; 60: 466-471.
- Lin TY, Hsia SH, Huang YC, Wu CT, Chang LY.Proinflammatorycytokine reactions in enterovirus 71 infections of the central nervous system.Clin Infect Dis 2003; 36: 269-274.
- World Health Organization Regional Office for the Western Pacific and the Regional Emerging Diseases Intervention (REDI) Centre. A Guide to Clinical ManLi/ agement and Public Health Response for Hand, Foot and Mouth Disease (HFMD). 2011, http://www.wpro.who.int/publications/PUB_9789290615255/en/.
- Nishimura Y, Shimojima M, Tano Y, Miyamura T, Wakita T, Shimizu H. Human P-selectin glycoprotein ligand-1 is a functional receptor for enterovirus 71. Nat Med 2009; 15: 794-797.
- Wang SM, Lei HY, Huang MC, Su LY, Lin HC, Yu CK, Wang JL, Liu CC. Modulation of cytokine production by intravenous immunoglobulin in patients with enterovirus 71-associated brainstem encephalitis. J ClinVirol 2006; 37: 47-52.
- Lin YW, Wang SW, Tung YY, Chen SH. Enterovirus71 infection of human dendritic cells. ExpBiol Med (Maywood) 2009; 234: 1166-1173.
- Khong WX, Foo DG, Trasti SL, Tan EL, Alonso S. Sustained high levels of interleukin-6 contribute to the pathogenesis of enterovirus 71 in a neonate mouse model. J Virology 2011; 85: 3067-3076.
- Ng PC, Li K, Wong RP, Chui K, Wong E, Li G, FokTF. Proinflammatory and anti-inflammatory cytokine responses in preterm infants with systemic infections. Arch Dis Child Fetal Neonatal Ed 2003; 88: F209- F213.
- Wang SM, Lei HY, Yu CK, Wang JR, Su IJ, Liu CC. Acute chemokine response in the blood and cerebrospinal fluid of children with enterovirus 71-associated brainstem encephalitis. J Infect Dis 2008; 198: 1002- 1006.
- Sato M, Hosoya M, Honzumi K, Watanabe M, NinomiyaN, Shigeta S, Suzuki H. Cytokine and cellular inflammatory sequence in enteroviral meningitis. Pediatrics 2003; 112: 1103-1107.
- Wang SM, Lei HY, Su LY, Wu JM, Yu CK, Wang JR, Liu CC. Cerebrospinal fluid cytokines in enterovirus 71 brain stem encephalitis and echovirus meningitis infections of varying severity. ClinMicrobiol Infect 2007; 13: 677-682.
- Zheng BJ, Chan KW, Lin YP, Zhao GY, Chan C, Zhang HJ, Chen HL, Wong SS, Lau SK, Woo PC, Chan KH, Jin DY, Yuen KY. Delayed antiviral plus immunomodulator treatment still reduces mortality in mice infected by high inoculum of influenza A/H5N1 virus. ProcNatlAcadSci U S A 2008; 105: 8091-8096.
- Elovaara I, HietaharjuA. Can we face the challenge of expanding use of intravenous immunoglobulin in neurology? Acta Neurol Scand 2010; 122: 309-315.
- Kishimoto C, Takamatsu N, Kawamata H, Shinohara H, Ochiai H. Immunoglobulin treatment ameliorates murine myocarditis associated with reduction of neurohumoralactivity and improvement of extracellular matrix change. J Am CollCardiol 2000; 36: 1979-1984.
- Chen Y, Liang W, Yang S, Wu N, Gao H, Sheng J, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet 2013; 381: 1916-1925.
- Ooi MH, Wong SC, Mohan A, Podin Y, Perera D, Clear D, del Sel S,Chieng CH, Tio PH, Cardosa MJ, Solomon T. Identification and validation of clinical predictors for the risk of neurological involvement in children with hand, foot, and mouth disease in Sarawak. BMC Infect Dis 2009; 9: 3.
- Chong CY, Chan KP, Shah VA, Ng WY, Lau G, TeoTE, Lai SH, Ling AE. Hand, foot and mouth disease in Singapore: a comparison of fatal and non-fatal cases. ActaPaediatr 2003; 92: 1163-1169.
- Kim SJ, Kim JH, Kang JH, Kim DS, Kim KH, Kim YH, et al. Risk factors for neurologic complications of hand, foot and mouth disease in the Republic of Korea, 2009. J Korean Med Sci 2013; 28: 120-127.
- Lin MT, Wang JK, Lu FL, Wu ET, Yeh SJ, Lee WL, Wu JM, Wu MH. Heart rate variability monitoring in the detection of central nervous system complications in children with enterovirus infection. J Crit Care 2006; 21: 280-286.
- Huang YF, Chiu PC, Chen CC, Chen YY, Hsieh KS, Liu YC, Lai PH, Chang HW. Cardiac troponin I: a reliable marker and early myocardial involvement with meningoencephalitis after fatal enterovirus-71 infection. J Infect 2003; 46: 238-243.