ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 7
Clinical efficacy comparison of arthroscopic subacromial smooth polishing and acromioplasty in treating of rotator cuff tears
Chao Sun, Zhaoxun Pan*, Xiaoming Yang, Zhongli Pang, Dekai Du and Xiaojun Min
Department of Joint Surgery, the Eighty-Ninth Hospital of People's Liberation Army, Weifang, China
- *Corresponding Author:
- Zhaoxun Pan
Department of Joint Surgery
The Eighty-Ninth Hospital of People's Liberation Army, China
Accepted date: December 3, 2016
Many physicians perform traditional Acromioplasty (AMP) in arthroscopic Rotator Cuff Repair (RCR) surgery. However, this surgery might cause shoulder pain, or joint instability postoperation. We compared the clinical efficacies of Arthroscopic Subacromial Smooth Polishing (ASSP) and AMP in RCR. The clinical data of 74 patients performed ARCR were retrospectively analysed, among who 36 patients were performed intraoperative SSP, and 38 patients were performed traditional AMP. The clinical efficacies of the two groups were compared, evaluated, and statistically analysed using VAS, Constant-Murley shoulder Score (CMS), and MRI before the surgery (T1), 3 months after the surgery (T2), and in the last follow-up (T3). The patients were followed up 18-36 months (average 26.9 months). The postoperative VAS and CMS of the two groups were statistically significantly different from those at T1 (P<0.001). The comparison of VAS and CMS between the two groups at T2 and T3 showed statistically significant differences (P<0.001), but the rotator cuff healing time showed no significant difference (P>0.05). SSP can significantly reduce postoperative shoulder pain and improve joint functions than AMP, but it cannot shorten the rotator cuff healing time.
Keywords
Polishing, Acromion, Rotator cuff, Shoulder impingement syndrome, Arthroscopy.
Introduction
Rotator Cuff Tears (RCTs) is common in the elderly, with the incidence rate more than 50% in people over 65 years old [1], and its risks can be greatly increased in athletes engaged in overhead sports and young people engaged in special labors, etc. [2]. RCTs is the main reason of shoulder pain in these populations, and the functions of shoulder joint can be lost in severe cases [3-6].
Due to the hypothesis of Neer impingement syndrome, many physicians perform AMP toward some type II and most type III acromion in rotator cuff repair so as to make it become flat type I acromion. However, this surgery might damage the coracoacromial ligament and dead center of deltoid. Gartsman et al. believed that: the resection of the coracoacromial ligament will easily result in the instability of shoulder joints, and the repeated friction and impacts at this state will cause lasting chronic pain [7,8]. Sanchez et al. reported one case of artificial humeral head replacement caused by glenohumeral arthritis combined with extensive RCTs, and found that the incidence of postoperative anterosuperior shoulder instability was 21% (7/33), exhibiting significant correlation with previous AMP histories (P<0.05) [9]. Tibone et al. performed AMP to 35 athletes with shoulder impingement syndrome, and 20% of the patients still exhibited postoperative mild to severe pain [10]. In the similar cases reported by Post et al. [11], 11% of the patients still had significant pain after AMP, 56% of the patients with preoperative symptoms of asthenia remained asthenia, and 29% of patients with motion limitation still had postoperative motion limitation; their the results showed that the proportion of the patients that could return to high-level sport was very low. Williams et al. [12] performed humeral head prosthesis replacement plus coracoacromial ligament conservation toward 21 patients with glenohumeral arthritis plus extensive RCTs, and the postoperative follow-up revealed that no shoulder instability or pain occurred.
We retrospectively analysed the clinical data of the patients performed ASSP or AMP in our department from July 2012 to May 2014, aiming to explore the clinical efficacies of ASSP.
Patients and Methods
General information
A total of 74 patients underwent arthroscopic rotator cuff repair in our department from July 2012 to May 2014 were retrospectively studied, 44 males and 30 females, aging 19-59 years (mean 47.3 years), including 48 cases of supraspinatus muscle tear, 9 cases of infraspinatus muscle tear, and 17 cases of complex tear. 36 patients were performed ASSP (the experiment group), and 38 patients were performed traditional AMP (the control group). This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of the Eighty-Ninth Hospital of People's Liberation Army. Written informed consent was obtained from all participants.
Inclusion criteria
1) confirmed as RCTs by MRI and physical examination; 2) type II or type III acromion displayed in X ray; 3) without shoulder joint adhesion, and passive shoulder activities were unrestricted; 4) in generally good health, without other diseases, and could tolerate the surgery; 5) with good compliance for the postoperative rehabilitation process.
Exclusion criteria
1) asymptomatic RCTs; 2) with obvious osteoporosis, which could easily lead to the instability of the fixing materials; 3) associated with other shoulder injuries, such as SLAP injury, Bankart injury, fractures around the shoulder joint ; 4) with a history of years of smoking; 5) with a history of hormone injection after shoulder injuries.
Surgical methods
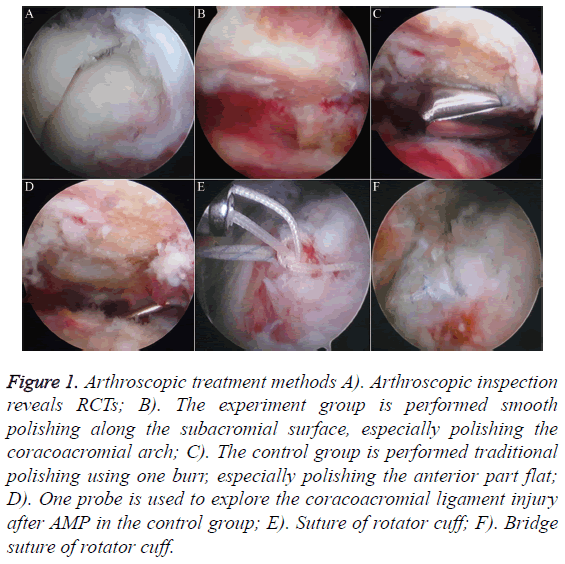
The surgery used the posterior, lateral, and anterior approaches, the arthroscope and surgical instruments were placed into using one puncture cone; firstly, the glenohumeral joint was inspected to display the ruptured rotator cuff (Figure 1A). After cleaning the glenohumeral joint and properly trimming the lateral sides of rotator cuff capsule, the scope was then placed into the subacromial space for different surgical methods, respectively.
Figure 1: Arthroscopic treatment methods A). Arthroscopic inspection reveals RCTs; B). The experiment group is performed smooth polishing along the subacromial surface, especially polishing the coracoacromial arch; C). The control group is performed traditional polishing using one burr, especially polishing the anterior part flat; D). One probe is used to explore the coracoacromial ligament injury after AMP in the control group; E). Suture of rotator cuff; F). Bridge suture of rotator cuff.
ASSP
One disposable planer (Smith and Nephew, U.S.) was used to polish the site 1/3 in front of the acromion so as to remove the subacromial soft tissue (using radio frequency (JC Medical Inc., US) for the removal if necessary); when the subacromial bones were revealed, one burr was placed via the lateral approach (Smith and Nephew, U.S.), and then trimmed the subacromial surface from the front to the rear according to the curvature of coracoacromial arch to achieve its smooth transition with the coracoacromial ligament (Figure 1B). When stopped the perfusion fluid, bleeding could be seen on the bone surface. The coracoacromial ligament was then explored, and if uneven downward-projected osteophytes were found in the anterior ligaments of the acromion, which might easily cause friction, one burr could be used to gently wipe them away, but the osteophytes in deep ligaments could be disregarded. The lateral side of acromion was then processed and polished to smooth arch using the burr. The proliferated osteophytes in the greater tuberosity could be polished and smoothened using the burr so as to reduce the postoperative friction and impact.
AMP
The 1/3 inferior surface before the acromion was firstly onestep processed using one planer until the acromial bones were revealed. One drill was then placed via the lateral shoulder approach and polished the acromion following the order of from the front to the back, as well as from the outside to the inside; secondly, the drill was re-placed via the anterior approach for the second time polishing, keeping the drill pipe appropriately parallel to the inferior acromial surface and polishing the anterior acromial part flat (Figure 1C) to make it become type I acromion. The result analysis showed that: during the polishing processing, the dead center of coracoacromial ligament in 18 cases was completely cut off (46%), 1/2-cut off in 13 cases (33%), and 1/3-cut off in 7 cases (Figure 1D). The fabric dead center in front of the deltoid was damaged to various degrees (30-50%) during AMP. When the surgery was completed, one planer was used to clean the floating part at the coracoacromial ligament and deltoid.
Rotator cuff repair
After completing the acromion processing, RCR could then be performed. We used the same procedure for each group with Healix anchors (Johnson and Johnson, U.S.) and Versalok anchors (Johnson and Johnson, U.S.) (Figure 1F).
Postoperative treatments
Shoulder activities within the first 6 weeks should mainly be passive, and changed to active 6 weeks later assisted with passive motions; the range of motion should be increased gradually. The follow-up was performed one month after the surgery and every 3 months later, and the follow-up contents included: 1) shoulder VAS score; 2) shoulder Constant-Murley score; 3) MRI to assess the rotator cuff healing; 4) developing and guiding further rehabilitation programs.
Statistical analysis
SPSS 17.0 (IBM, USA) software package was used for the statistical analysis. First, the measurement data were performed the normal distribution test, and if they were normally distributed, the data were then expressed as (?x ± s), and the intergroup comparison used the two-sample t test; otherwise, the multiple independent sample rank sum test was used, with P<0.05 considered as statistically significant difference.
Results
The 74 patients of the two groups were followed up via the way of hospital visit, and the average follow-up lasted 26.9 months (18-36 months). No postoperative neurological injury and postoperative joint adhesion occurred.
Comparison of postoperative pain improvement between the two groups
The postoperative shoulder pain in the two groups were significantly reduced than before (Table 1); at T3, the VAS score of the experiment group was decreased from 5.61 ± 0.94 preoperatively to 0.19 ± 0.40 points (P<0.001), and that in the control group was reduced from 5.67 ± 0.96 preoperatively to 1.50 ± 1.35 points (P<0.001); the intergroup comparison showed statistically significant difference (F=50.89, t=5.70, P<0.001).
| Group | VAS Score | ||
|---|---|---|---|
| Pre-operation | 3 months post-operation | Final followed up | |
| Trial Group | 5.61 ± 0.94 | 0.62 ± 0.71 | 0.19 ± 0.40 |
| Control Group | 5.67 ± 0.96 | 1.46 ± 0.82 | 1.50 ± 1.35 |
| P Value | P>0.05 | t=4.86 | t=5.70 |
| P<0.001 | P<0.001 | ||
Table 1: VAS scores at T1, T2, and T3.
Among the patients in the two groups, one patient in the experiment group was found anterior shoulder pain in the 6 month follow-up, which was caused by biceps tendinitis, and the symptoms were remitted after administrated prednisolone; 9 patients in the control group appeared pain and tenderness when performing shoulder anteflexion and abduction, and this was considered to be related with the injuries of deltoid and coracoacromial ligament as well as postoperative scarring; the patients were given oral anti-inflammatory analgesic drugs and physical therapy, and the pain in one patient was remitted, and partially reduced in the rest eight patients (21.0%), but activityassociated pain at this site still existed at T3.
Comparison of postoperative CMS scores
The postoperative CMS scores of the two groups were increased than those before the surgery (Table 2). At T2, CMS in the experiment group was improved from 66.18 ± 5.53 preoperatively to 84.62 ± 3.73 points (P<0.001), and that in the control group was improved from 68.41 ± 4.83 preoperatively to 83.80 ± 3.16 points (P<0.001); there was no statistically significant difference between the two groups (t=1.107, P=0.275); at T3, CMS in the experiment group was 91.53 ± 1.63 points, and that in the control group was 88.13 ± 2.06 points, and there was a statistically significant difference between the two groups (F=5.26, t=7.89, P<0.001).
| Group | CMS Score | ||
|---|---|---|---|
| Pre-operation | 3 months post-operation | Final followed up | |
| Trial Group | 66.18 ± 5.53 | 84.62 ± 3.73 | 91.53 ± 1.63 |
| Control Group | 68.41 ± 4.83 | 83.80 ± 3.16 | 88.13 ± 2.06 |
| P Value | P>0.05 | t=1.107 | t=7.89 |
| P=0.275 | P<0.001 | ||
Table 2: CMS scores at T1, T2, and T3.
At T2, the patients in both groups exhibited wider ranges of shoulder abduction, as well as pain and various degrees of motion limits when performing anteflexion and exterior and interior rotation; after the continuous rehabilitation, all the patients in the experiment group exhibited free shoulder movements at T3 and no shoulder numbness. 55.3% of the patients in the control group (21/38) exhibited limited shoulder anteflexion, abduction, or muscle strength reduction. The middle- and long-term recovery of shoulder functions in the experiment group was better than the control group.
Comparison of rotator cuff healing time in MRI images
When MRI images displayed the structural integrity, good continuity, and oedema-free tendons at the repair site of the rotator cuff, it could be considered as the rotator cuff healed [13]. At T3, the two groups showed no re-RCTs. The MRI images of the experiment group showed the healing time as 5.83 ± 0.81 months, and those of the control group showed the healing time as 5.87 ± 0.88 months; there is no statistical significance between the two groups (F=0.289, t=0.179, P=0.859), indicating that the comparison between ASSP and AMP showed no significant difference in rotator cuff healing time.
Discussion
Coracoacromial arch is a concave curved smooth surface, and composed of the lower surface of the anterior acromion and coracoacromial ligament; when the shoulder joints move, the rotator cuff glides along it, thus constituting the humerusscapula joint. It provides a powerful anterosuperior support for the shoulder joints [14,15].
Damages to the dead center of deltoid muscle in AMP are also the main reason of persistent pain and abductor strength reduction. Tendons in the front part of deltoid muscle directly attach to the anterolateral part of the acromion, so partial tendon fibers will be inevitably being destroyed in AMP. Torpey et al. [16] found that in arthroscopic AMP, if 4 mm of anterior acromial bone is cut off, 43% of the dead center of deltoid will be damaged, and cutting off 6 mm will destroy 72%. In this study, we found that in AMP, together with opening the deltoid fascia, the dead center of deltoid would be damaged, so it would impact the early rehabilitation, and the postoperative contracture and adhesion of deltoid scars were prone to causing shoulder pain and motion restriction.
In order to avoid damaging the coracoacromial arch and deltoid in AMP, many scholars chose the subacromial decompression instead of AMP so as to expand the subacromial volume and to avoid the friction and impact of acromion on rotator cuff. Budoff et al. [17] and Fenlin et al. [18] had confirmed in their own studies that simple arthroscopic subacromial decompression and greater tubercleplasty have good excellent rate in long-term follow-up in treating RCTs. Verhelst et al. [19] performed reverse subacromial decompression when treated 33 elderly RCTS patients, and followed up for a mean 38 months; the results showed that the shoulder functions were significantly increased than those before the surgery. The achievements of these good surgical results are closely related to intra-operatively increasing the subacromial volume, and reducing the compressive stress and friction between the humerus and scapula.
In this study, ASSP is one improvement based on this type of surgery, and its essence is still the subacromial decompression; meanwhile, it pays more emphasis on smoothly repairing the humerus-scapula motion interface, so the postoperative repeated impact and friction caused by motions can be minimally reduced, thus reducing the ischemia, oedema, and pain of the rotator cuff. After two-year postoperative recovery, the AMP group still has 21.5% (8/38) of the patients existing anterior shoulder pain at T3, but the pain in the ASSP group has been obviously relieved, so it also confirms the important roles of coracoacromial arch in maintaining the glenohumeral stability and restoring the shoulder functions.
Studies have found that a variety of cell growth factors can promote the proliferation, collagen synthesis, and vascularization of tendon cells, thus promoting the tendon regeneration and bone healing after rotator cuff repair [20,21], such as platelet-derived growth factors, fibroblast growth factors, etc. [22]. Many animal studies all suggested that these factors can contribute to the bone healing after rotator cuff repair [23,24]. In this study, ASSP and AMP both caused bone bleeding on the subacromial surface, thus promoting the releasing of blood marrow growth factors and their attachment onto the rotator cuff surface, and the results showed there was no statistically significant difference in the rotator cuff healing time between the two groups.
Contributions
Chao Sun was responsible for writing the paper and summarizing all the data, Zhaoxun Pan provided ideas and performed operation; Xiaoming Yang, Zhongli Pang, Dekai Du and Xiaojun Min were responsible for physical examination, enrolled and following up patients.
Conflict of Interest
All the authors of this study have no objection to the author ranking order; there is no conflict of interest between the authors and their institutional affiliations; the fees of MRI inspection were funded by the Dean foundation of overhead sports-caused shoulder injury Research in our hospital.
References
- Stevenson JH, Trojian T. Evaluation of shoulder pain. J Fam Pract 2002; 51: 605-611.
- Akbar M, Brunner M, Ewerbeck V, Wiedenhofer B, Grieser T. Do overhead sports increase risk for rotator cuff tears in wheelchair users? Arch Phys Med Rehabil 2015; 96: 484-488.
- Geary MB, Elfar JC. Rotator cuff tears in the elderly patients. Geriatr Orthop Surg Rehabil 2015; 6: 220-224.
- Aumiller WD, Kleuser TM. Diagnosis and treatment of cuff tear arthropathy. JAAPA 2015; 28: 33-38.
- Roedl JB, Morrison WB, Ciccotti MG, Zoga AC. Acromial apophysiolysis: superior shoulder pain and acromial nonfusion in the young throwing athlete. Radiology 2015; 274: 201-209.
- Shaffer B, Huttman D. Rotator cuff tears in the throwing athlete. Sports Med Arthrosc 2014; 22: 101-109.
- Gartsman GM, OConnor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elbow Surg 2004; 13: 424-426.
- McCallister WV, Parsons IM, Titelman RM, Matsen FA. Open rotator cuff repair without acromioplasty. J Bone Joint Surg Am 2005; 87: 1278-1283.
- Sanchez-Sotelo J, Cofield RH, Rowland CM. Shoulder hemiarthroplasty for glenohumeral arthritis associated with severe rotator cuff deficiency. J Bone Joint Surg Am 2001; 83-83A: 1814-22.
- Tibone JE, Jobe FW, Kerlan RK, Carter VS, Shields CL. Shoulder impingement syndrome in athletes treated by an anterior acromioplasty. Clin Orthop Relat Res 1985; 134-140.
- Post M, Cohen J. Impingement syndrome. A review of late stage II and early stage III lesions. Clin Orthop Relat Res 1986; 126-132.
- Williams GR, Wong KL, Pepe MD, Tan V, Silverberg D, Ramsey ML, Karduna A, Iannotti JP. The effect of articular malposition after total shoulder arthroplasty on glenohumeral translations, range of motion, and subacromial impingement. J Shoulder Elbow Surg 2001; 10: 399-409.
- Saccomanno MF, Cazzato G, Fodale M, Sircana G, Milano G. Magnetic resonance imaging criteria for the assessment of the rotator cuff after repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 2015; 23: 423-442.
- Moorman CT, Warren RF, Deng XH, Wickiewicz TL, Torzilli PA. Role of coracoacromial ligament and related structures in glenohumeral stability: a cadaveric study. J Surg Orthop Adv 2012; 21: 210-217.
- Yamamoto N, Muraki T, Sperling JW, Steinmann SP, Itoi E, Cofield RH, An KN. Contact between the coracoacromial arch and the rotator cuff tendons in nonpathologic situations:a cadaveric study. J Shoulder Elbow Surg 2010; 19: 681-687.
- Torpey BM, Ikeda K, Weng M, van der Heeden D, Chao EY, McFarland EG. The deltoid muscle origin. Histologic characteristics and effects of subacromial decompression. Am J Sports Med 1998; 26: 379-383.
- Budoff JE, Rodin D, Ochiai D, Nirschl RP. Arthroscopic rotator cuff debridement without decompression for the treatment of tendinosis. Arthroscopy 2005; 21: 1081-1089.
- Fenlin JM, Chase JM, Rushton SA, Frieman BG. Tuberoplasty: creation of an acromiohumeral articulation-a treatment option for massive, irreparable rotator cuff tears. J Shoulder Elbow Surg 2002; 11: 136-142.
- Verhelst L, Vandekerckhove PJ, Sergeant G, Liekens K, Van Hoonacker P, Berghs B. Reversed arthroscopic subacromial decompression for symptomatic irreparable rotator cuff tears: mid-term follow-up results in 34 shoulders. J Shoulder Elbow Surg 2010; 19: 601-608.
- Edwards SL, Lynch TS, Saltzman MD, Terry MA, Nuber GW. Biologic and pharmacologic augmentation of rotator cuff repairs. J Am Acad Orthop Surg 2011; 19: 583-589.
- Oliva F, Via AG, Maffulli N. Role of growth factors in rotator cuff healing. Sports Med Arthrosc 2011; 19: 218-226.
- Hee CK, Dines JS, Dines DM, Roden CM, Wisner-Lynch LA, Turner AS, McGilvray KC, Lyons AS, Puttlitz CM, Santoni BG. Augmentation of a rotator cuff suture repair using rhPDGF-BB and a type I bovine collagen matrix in an ovine model. Am J Sports Med 2011; 39: 1630-1639.
- Tokunaga T, Shukunami C, Okamoto N, Taniwaki T, Oka K, Sakamoto H, Ide J, Mizuta H, Hiraki Y. FGF-2 stimulates the growth of tenogenic progenitor cells to facilitate the generation of tenomodulin-positive tenocytes in a rat rotator cuff healing model. Am J Sports Med 2015; 43: 2411-2422.
- Street M, Thambyah A, Dray M, Amirapu S, Tuari D, Callon KE, McIntosh JD, Burkert K, Dunbar PR, Coleman B, Cornish J, Musson DS. Augmentation with an ovine fore stomach matrix scaffold improves histological outcomes of rotator cuff repair in a rat model. J Orthop Surg Res 2015; 10: 165.