ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2018) Volume 29, Issue 5
Colonic intussusception caused by an ulcerating lipoma in an adult: A rare case report and literature review
Yingying Zhuang1,2#, Shipeng Liu3#, Yuntao Shi4, Zhonghong Wang3, Wei Huang2, Daoyan Lu2, Jiandong Zhang2, Dan Kong2 and Bin Wang5*
1Shandong Medical Imaging Research Institute, Shandong University, No. 324, Jingwu Road, Jinan, Shandong, PR China
2Department of Medical Imaging, Huai’an First People’s Hospital, Affiliated to Nanjing Medical University, No. 6, Western Beijing Road, Huaiyin District, Huai’an, Jiangsu, PR China
3Department of Gastroenterology, Hongze Huai’an District People’s Hospital, No.102, Dongfeng Road, Hongze District, Jiangsu, PR China
4Department of Gastroenterology, Huai’an First people’s Hospital, Affiliated to Nanjing Medical University, No. 6, Western Beijing Road, Huaiyin District, Huai’an, Jiangsu, PR China
5Medical Imaging Research Institute, Binzhou Medical University, No.346, Guanhai Road, Laishan District, Yantai, Shandong, PR China
#These authors contributed equally to these work
- *Corresponding Author:
- Bin Wang
Medical Imaging Research Institute
Binzhou Medical University, PR China
Accepted on December 7, 2017
DOI: 10.4066/biomedicalresearch.29-17-1660
Visit for more related articles at Biomedical ResearchIntestinal lipomas are rare nonepithelial tumors that are typically small in size and detected incidentally. Colonic intussusception is an uncommon complication of colonic lipoma. A 56 y old woman visited our emergency room with sudden onset of intermittent abdominal cramps. A CT scan showed a 5.0 cm, nodular, homogenous, hypodense structure in the hepatic flexure of the colon as the lead point of an intussusception. The hypodense structure was suggestive of a colonic lipoma, and the tumor was suspected to be the cause of the intestinal intussusception. Laparoscopic exploration was performed, and the pathology demonstrated a mature submucosal colonic lipoma. In addition to the case report, we discuss the role of imaging modalities in diagnosing neoplasms and for assessing the clinical behavior of lipomas when symptomatic.
Keywords
Intussusception, Lipoma, Computed tomography.
Introduction
Colonic lipoma is a rare benign tumor with a reported incidence ranging from 0.15% to 4.4% [1]. The most common position of colonic lipoma is the right hemicolon, followed by the descending and transverse colon. Although the majority of colonic lipomas are small and asymptomatic, some cause symptoms such as abdominal pain, diarrhea, bowel obstruction and intussusception [1,2]. Here, we present a case report of a giant colonic lipoma causing ascending-colonic intussusception and discuss the role of imaging modalities for diagnosing neoplasms to assess the clinical behavior of lipomas when symptomatic.
Case Report
The patient described in this case report provided written informed consent for both the report and the accompanying images.
A 56 y old woman with a 5 y history of obstipation and intermittent abdominal pain was admitted to the emergency department. Her abdominal pain had been exacerbated in the past week and was accompanied by a change in bowel habits. Mucous and blood were present in the stool starting three days prior to admission. Moderate, paroxysmal and cramp-like pain was present in the right hypochondrium and radiated to the back, without signs of peritonitis. She did not report any history of anemia, dyspeptic symptoms, episodes of diarrhea, or rectal bleeding. No disease history was reported. The physical examination was unremarkable. Laboratory test results showed elevated inflammatory parameters and a high
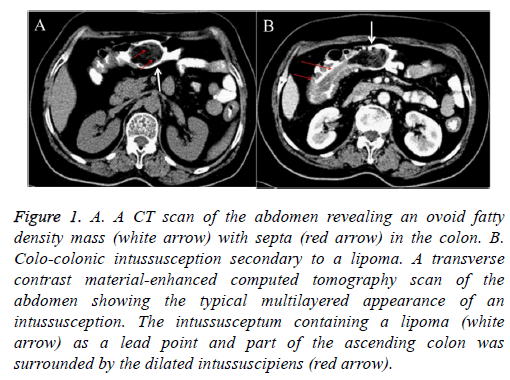
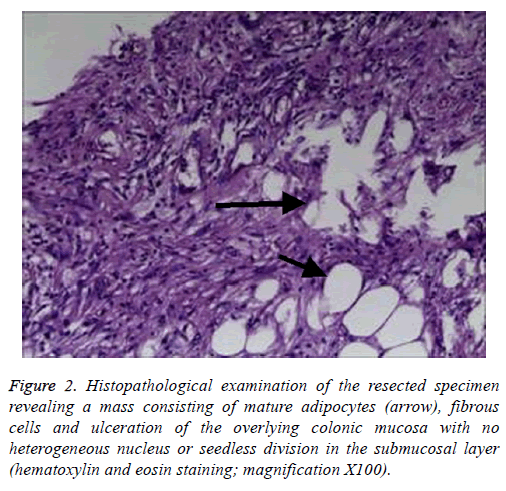
level of C-reactive protein (10.8 mg/l). Tumor makers were within the normal ranges. She also underwent Digital Radiography (DR) and Computed Tomography (CT) examinations of the abdomen. The DR showed no obvious abnormalities. The CT scan showed a 5.0 cm, nodular, homogenous, hypodense structure in the hepatic flexure of the colon, suggestive of a colonic lipoma (Figure 1A), as a lead point of an intussusception (Figure 1B). The lipoma was suspected as the cause of the intestinal intussusception, and laparoscopic exploration was performed. Subsequent histopathological examination confirmed that the mass was a lipoma with ulceration and reactive changes without evidence of malignancy (Figure 2). A segment resection was performed in the hepatic flexure of the colon with end-to-end anastomosis. The postoperative course was uneventful, and the patient was discharged from the hospital on the 7th postoperative day. The patient was in a healthy condition after 1 year of follow-up.
Figure 1: A. A CT scan of the abdomen revealing an ovoid fatty density mass (white arrow) with septa (red arrow) in the colon. B. Colo-colonic intussusception secondary to a lipoma. A transverse contrast material-enhanced computed tomography scan of the abdomen showing the typical multilayered appearance of an intussusception. The intussusceptum containing a lipoma (white arrow) as a lead point and part of the ascending colon was surrounded by the dilated intussuscipiens (red arrow).
Figure 2: Histopathological examination of the resected specimen revealing a mass consisting of mature adipocytes (arrow), fibrous cells and ulceration of the overlying colonic mucosa with no heterogeneous nucleus or seedless division in the submucosal layer (hematoxylin and eosin staining; magnification X100).
Discussion
Lipomas are the most common non-epithelial neoplasms of the gastrointestinal tract and can be found in any part of the gut [1-3]. Colonic lipomas are benign submucosal tumors composed of mature adipose tissue and were first reported by Bauer in 1757 [2,3]. After reviewing the literature for the most recent cases (Table 1) [1-13], we concluded that most lipomas range in size from 2 mm to 30 cm and that the majority of patients are between 50 and 70 y of age, with a female predominance. Colonic lipomas are typically asymptomatic or minimally symptomatic when less than 2.0 cm in size, and they are usually detected during endoscopy, surgery, or autopsy. A prior study indicated that only 32% to 50% of cases are diagnosed preoperatively [4-5]. In contrast, large lipomas generally produce symptoms, including abdominal pain, diarrhea, bowel obstruction, and obstipation. These symptoms are primarily caused by chronic intermittent ileocolonic or colo-colonic intussusceptions [5-8]. Furthermore, large lipomas can have ulcerations and may cause gastrointestinal bleeding as a result of pressure necrosis in the overlying mucosa [4].
| Case | Sex | Age (y) | Symptom | Examination | Tumor location | Size (cm) | Treatment | First author and Journal |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 49 | Intermittent colicky abdominal pain | CT, colonoscopy, barium enema | Hepatic flexure of the colon | 9 | Laparocsopic surgery | Moussa |
| Surg Laparosc Endosc Percutan Tech [1] | ||||||||
| 2 | M | 65 | Altered bowel habits and rectal bleeding | CT, colonoscopy | Sigmoid colon | 4 | Laparocsopic surgery | Moussa |
| Surg Laparosc Endosc Percutan Tech [1] | ||||||||
| 3 | F | 65 | Intermittent abdominal pain | CT, colonoscopy | Transverse colon | 4.0 × 5.0 | Laparotomy | Zhou |
| Oncol Lett [2] | ||||||||
| 4 | F | 47 | Constipation | CT, colonoscopy | Descending colon | 13.0 × 5.0 | Laparocsopic surgery | Bagherzadeh |
| Gastroenterol hepatol Bed ench [3] | ||||||||
| 5 | F | 40 | Mucous and blood present in stool | Colonoscopy, US | Sigmoid colon | 5.0 × 5.0 × 5.0 | Laparotomy | Roy |
| Birdem Med J [4] | ||||||||
| 6 | M | 39 | A mass prolapsed through the anal canal | CT, colonoscopy | Sigmoid colon | 10 × 8 × 7.5 | Laparotomy | Kose |
| Oncol Lett [5] | ||||||||
| 7 | M | 38 | Hypogastric pain, constipation, loss of appetite and weight | CT, colonoscopy | Splenic flexure of the colon | 7.0 × 5.0 × 4.5 | Resection | Zare-Khormizi |
| Pathologica [6] | ||||||||
| 8 | M | 50 | Intermittent abdominal pain | CT | Transverse colon | 6.5 × 4.0 × 4.5 | Laparocsopic surgery | Kwag |
| Ann Coloproctol [7] | ||||||||
| 9 | F | 54 | Severe abdominal pain | CT, colonoscopy | Ascending colon | 6.0 × 4.0 × 3.5 | Laparocsopic surgery | Kwag |
| Ann Coloproctol [7] | ||||||||
| 10 | M | 65 | Rectal bleeding | CT, colonoscopy | Cecum | 3.5 × 2.1 × 2 | Laparocsopic surgery | Boler |
| Am J Case Rep [8] | ||||||||
| 11 | M | 65 | Fatigue and deyspnea, abdominal pain | CT, colonoscopy | Cecum and ileum | 3.3 × 1.8 × 2 | Laparocsopic surgery | Boler |
| Am J Case Rep [8] | ||||||||
| 12 | M | 63 | Abdominal distention and bloody stools | CT, colonoscopy | Transverse colon | 7.8 × 6.5 × 3.5 | Laparocsopic surgery | Boler |
| Am J Case Rep [8] | ||||||||
| 13 | M | 74 | Abdominal pain and discomfort | CT, colonoscopy | Cecum | 7.2 × 6.0 × 5.5 | Laparocsopic surgery | Boler |
| Am J Case Rep [8] | ||||||||
| 14 | F | 34 | Intermittent abdominal pain | CT, barium enema, colonoscopy | Ascending colon | 6 × 5 × 4.5 | Laparotomy | Atmatzidis |
| Case Rep Surg [9] | ||||||||
| 15 | M | 45 | Iron deficiency anemia, flesh rectal bleeding | Colonoscopy | Sigmoid colon | 8 | Endoscopic resection | Khorashad |
| J Res Med Sci [10] | ||||||||
| 16 | M | 38 | Hematochezia, abdominal pain | Colonoscopy , barium enema, CT | Transverse colon | 7.5 × 4.5 | Spontaneous expulsion | Ishiyama |
| Endoscopy 2011 [11] | ||||||||
| 17 | M | 60 | Abdominal pain | Colonoscopy | Sigmoid colon | 3.5 | Endoscopic resection | Geraci |
| Case Rep Gastroenterol [12] | ||||||||
| 18 | M | 31 | Intermittent abdominal pain, rectal bleeding | CT | Descending colon | 5.5 × 5 × 3.5 | Laparotomy | Barchetti |
| Eur Rev Med Pharmacol Sci [13] | ||||||||
| 19 | F | 82 | Abdominal pain | Colonoscopy | Transverse colon | 2 | Endoscopic resection | Tomiki |
| Case Rep Gastroenterol | ||||||||
| 20 | M | 74 | Abdominal pain and melena | Colonoscopy | Transverse colon | 5 | Endoscopic resection | Tomiki |
| Case Rep Gastroenterol | ||||||||
| 21 | F | 36 | Intermittent abdominal pain and diarrhea | CT | Sigmoid colon | 4 × 4 × 3 | Laparotomy | Paul |
| J Case Rep Images Surg | ||||||||
| 22 | M | 41 | Abdominal pain and constipation | Colonoscopy | Descending colon | 5 × 3 × 1.5 | Endoscopic resection | Lee |
| World J Gastroenterol | ||||||||
| 23 | M | 48 | Abdominal pain | Colonoscopy | Ascending colon | 7.5 × 4.5 × 4.0 | Endoscopic resection | Lee |
| World J Gastroenterol | ||||||||
| 24 | M | 35 | Intermittent abdominal pain, rectal bleeding | CT | Sigmoid colon | 2.5 | Laparotomy | Mohamed |
| Int J Surg Case Rep | ||||||||
| 25 | M | 49 | Abdominal pain and constipation | CT | Hepatic flexure of the colon | 5 | Laparotomy | Toumi |
| Tunis Med | ||||||||
| 26 | F | 59 | Progressive colicky abdominal pain | CT | Hepatic flexure of the colon | 6 × 5 | Laparotomy | Toumi |
| Tunis Med | ||||||||
| 27 | F | 73 | Intermittent abdominal pain | CT, colonoscopy | Ileocecal valve | 5.5 × 3.0 × 2.2 | Endoscopic resection | Kasaka |
| Endoscopy | ||||||||
| 28 | F | 34 | Intermittent abdominal pain and constipation | CT, colonoscopy | Descending colon | 5.3 × 4.1 × 4.6 | Laparocsopic surgery | Allos |
| Am J Case Rep | ||||||||
| 29 | F | 68 | Abdominal discomfort | Colonoscopy | Ascending colon | 0.9 | Endoscopic resection | Yeom |
| World J Clin Cases | ||||||||
| 30 | F | 65 | Abdominal discomfort | Colonoscopy | Ileocecal valve | 3 × 3 | Endoscopic resection | Kim |
| Clin Endosc | ||||||||
| 31 | F | 46 | Abdominal discomfort | Colonoscopy | Sigmoid colon | 3 × 3 | Endoscopic resection | Kim |
| Clin Endosc | ||||||||
| 32 | M | 48 | Abdominal discomfort | Colonoscopy | Ascending colon | 4 × 7 | Endoscopic resection | Kim |
| Clin Endosc | ||||||||
| 33 | M | 55 | Severe abdominal pain | US, CT | Ascending colon | 3 × 3 × 4.5 | Laparotomy | Mouaqit |
| BMC Surg | ||||||||
| 34 | F | 54 | Intermittent abdominal pain | US, CT | Descending colon | 6 | Laparotomy | Grasso |
| Ann Ital Chir | ||||||||
| 35 | F | 31 | Abdominal pain | DR, US, CT, colonoscopy | Descending colon | 5.5 | Laparotomy | Bentama |
| Pan African Med J | ||||||||
| 36 | M | 74 | Abdominal discomfort and altered bowel habits | CT, colonoscopy | Hepatic flexure of the colon | 3.3 × 4.3 × 3.4 | Laparocsopic surgery | Coyne |
| JSCR | ||||||||
| 37 | M | 52 | Abdominal pain and constipation | CT | Ascending colon | 5 | Endoscopic resection | Soares |
| Endoscopy | ||||||||
| 38 | M | 31 | Intermittent abdominal pain and rectal bleeding | CT, colonoscopy | Descending colon | 5.5 × 5 × 3.5 | Laparotomy | Barchetti |
| Eur Rev Med Pharmacol Sci | ||||||||
| 39 | M | 48 | Abdominal discomfort | Colonoscopy | Transverse colon | 8 | Endoscopic resection | Jeong |
| Gut Liver | ||||||||
| 40 | F | 47 | Intermittent colicky abdominal pain | CT, colonoscopy | Hepatic flexure of the colon | 5 × 4 × 4 | Laparotomy | Lin |
| Endoscopy |
Table 1. Characteristics of reported cases of adult colonic lipomas.
Intussusception remains a rare condition in adults. Only 5% of intussusceptions are found in the adult population, and 1% of these are bowel obstructions. Approximately 90% of intussusceptions in adults have an organic cause, with primary carcinoma representing 65-70% of all cases [6]. Colonic lipoma as a leading cause is uncommon.
Imaging modalities can aid in the preoperative diagnosis of colonic lipomas. Barium enemas usually show ovoid, welldemarcated filling defects and smooth sub-mucosal masses [7-9]. The "squeeze sign" describes when a lipoma adopts a fusiform appearance with colonic peristalsis; such deformation can result from external pressure or peristalsis. During colonoscopy, colonic lipomas typically appear as a submucosal mass covered by intact mucosa. Elevation of mucosa using biopsy forceps ("tent sign"), indentation of mucosa after pressing on it ("cushion sign"), or extrusion of fat after biopsy ("naked fat sign") are also observed [10-12]. Lipomas can be difficult to differentiate from a malignant lesion due to the associated necrotic mucosa, ulceration, and relatively hard texture of the lesion. When a lesion is actively bleeding, endoscopic biopsy may not be safe or reliable. In most cases, CT can clearly reveal the characteristic fatty densitometric features of lipomas and definitively diagnose intestinal lipomas, avoiding unnecessary endoscopy or surgery. On CT, lipomas usually appear as well-circumscribed submucosal masses with homogeneous fat attenuation and thin fibrous septa. CT can also detect colonic lipoma complications, such as intussusception. However, intussuscepted lipomas may not demonstrate normal fat attenuation and may have a heterogeneous appearance reflective of the degree of infarction and fat necrosis present at the time of radiologic evaluation. If prominent fibrous septa and modularity are evident, the imperative differential diagnosis is liposarcoma [4]. Magnetic Resonance Imaging (MRI) is particularly suited to detecting fatty lesions because signal intensity characteristics typical for adipose tissue are evident on T1-weighted and fat-suppressed images. However, MRI is seldom used for detecting and studying intestinal neoplastic lesions [1-2,13,14].
There is an urgent need for doctors to address symptomatic patients with large lipomas who are developing intussusceptions. Ultrasound is a suitable method for this purpose because it is easy to perform, reproducible, and less invasive than other methods. On ultrasound, an abdominal mass with a “donut” or “target” sign in which the outermost layer represents the sheath and the multilayer ring structure represents the invaginated intestinal segment, is pathognomonic for the presence of an intussusception [13,14]. Recent reports have shown that abdominal CT scanning has a diagnostic sensitivity of 58-100% and a specificity of 57-71%, and this method is considered the “gold standard” for diagnosis [6,7]. CT can clearly reveal the typical characteristics of uniform tumor density with thin septa, clear borders, and no enhancement. Additionally, a “target” sign or “sausageshaped” mass on CT, depending on the angle of the beam relative to the intussusception, represents an inner central area of invaginated intussusceptum that is surrounded by mesenteric fat and associated vasculature, all of which are surrounded by the thick-walled intussuscipiens. In the case of lipoma, the tumor is the lead point within the lumen of the intussuscipiens. Mesenteric vessels within the bowel lumen are also typically observed. Because of the ability to visualize these features, CT findings are very helpful when operating.
Asymptomatic small lipomas may not require intervention. Though spontaneous expulsion of lipomas through the rectum has been reported [5,11,14], a small subgroup requires surgical intervention, including those with suspected malignancy, symptomatic lipomas, surgical emergencies such as intussusceptions, and obstruction with ulceration and bleeding [7]. The management strategy for colonic lipomas mainly depends on the size, clinical symptoms, and preoperative diagnosis.
The indication of endoscopic resection of colonic lipomas is still a subject of controversy [8]. Various endoscopic procedures including snare resection, ESD, and unroofing or the endoloop technique have been introduced recently for safe resection. Khorashad et al. and Geraci et al. suggest that endoscopic removal of colonic lipomas larger than 2 cm, even if is technically difficult because of their vascular nature, large pedicle, and size, is safe, feasible and effective using standard polypectomy technique with the availability of endoloop and hemoclips in case of uneventful complications or to prevent it [10,12].
Recently, laparoscopic procedure and minilaparotomy approach were reported as an alternative to conventional laparotomy used in removal of large colonic lipomas with all the known advantages of minimally invasive procedures [8]. In the article, there is a case about adopting laparoscopic procedures to excise the large colonic lipoma which goes well, and the postoperative recovered well.
Symptomatic colonic lipomas are very rare and present with a variety of symptoms depending on location and size, often leading to misdiagnosis. A correct and timely diagnosis is important to avoid complications. CT can assist in providing confirmatory diagnosis of a colonic lipoma. Surgical resection remains the treatment of choice, with an excellent prognosis and no reports of recurrence.
Acknowledgements
We acknowledge all the doctors who helped with this work. This work was supported by the Science and Technology Bureau of Huai’an, Jiangsu Province, China (HAS2014009-3).
References
- Moussa OM, Tee M, Khan AU, Selvasekar CR. Computerized tomography providing definitive diagnosis of colonic lipoma: a case series. Surg Laparosc Endosc Percutan Tech 2013; 23: 232-234.
- Zhou XC, Hu KQ, Jiang Y. A 4-cm lipoma of the transverse colon causing colonic intussusception: A case report and literature review. Oncol Lett 2014; 8: 1090-1092.
- Bagherzadeh SR, Sadeghi A, Rad N, Safari MT, Barzegar F. Colonic intussusception in descending colon: An unusual presentation of colon lipoma. Gastroenterol Hepatol Bed Bench 2016; 9: 93.
- Roy S, Mondal SK Maitra TK. Intussuscepted sigmoid colonic lipoma mimicking carcinoma rectum. Birdem Med J 2015; 5: 56-58.
- Kose E, Cipe G, Demirgan S, Oguz S. Giant colonic lipoma with prolapse through the rectum treated by external local excision: a case report. Oncol Lett 2014; 8: 1377-1379.
- Zare-Khormizi MR, Moghimi M, Pourrajab F. Giant pedunculated polypoid submucosal lipoma of the splenic flexure of colon: case report and review of the literature. Pathologica 2014; 106: 77-81.
- Kwag SJ, Choi SK, Jung EJ, Jung CY, Jung SH, Park TJ, Ju YT. Surgical strategy for colonic intussusception caused by a giant colonic lipoma: a report of two cases and a review of the literature. Ann Coloproctol 2014; 30: 147-150.
- Boler DE, Baca B, Uras C. Laparoscopic resection of colonic lipomas: When and why? Am J Case Rep 2013; 14: 270-275.
- Atmatzidis S, Chatzimavroudis G, Patsas A, Papaziogas B, Kapoulas S, Kalaitzis S, Ananiadis A, Makris J, Atmatzidis K. Pedunculated cecal lipoma causing colo-colonic intussusception: a rare case report. Case Rep Surg 2012; 2012: 279213.
- Khorashad AK, Hosseini SM, Gaffarzadegan K, Farzanehfar MR, Zivarifar HR. Endoscopic resection of large colonic lipomas assisted by a prototype single-use endoloop device. J Res Med Sci 2011; 16: 1511-1515.
- Ishiyama S, Tashiro Y, Nagayasu K, Niwa K, Ono S, Sugimoto K, Hata M, Kamiyama H, Komiyama H, Takahashi M. Spontaneous disappearance of a giant colonic lipoma after endoscopic biopsy. Endoscopy 2011; 43: 16.
- Geraci G, Pisello F, Arnone E, Sciuto A, Modica G, Sciume C. Endoscopic resection of a large colonic lipoma: case report and review of literature. Case Rep Gastroenterol 2010; 4: 6-11.
- Barchetti F, Al Ansari N, De Marco V, Caravani F, Broglia L. Giant lipoma of descending colon diagnosed at CT: report of a case. Eur Rev Med Pharmacol Sci 2010; 14: 573-575.
- Gollub MJ. Colonic intussusception: clinical and radiographic features. AJR Am J Roentgenol 2011; 196: 580-585.
- Kang B, Zhang Q, Shang D, Ni Q, Muhammad F, Hou L, Cui W. Resolution of intussusception after spontaneous expulsion of an ileal lipoma per rectum: a case report and literature review. World J Surg Oncol 2014; 12: 143.