ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 9
Contractile response of lipopolysaccharide-treated rat thoracic aortas to adrenaline or noradrenaline with or without local anaesthetic agents
1Department of Anaesthesiology, Graduate School of Dentistry, Kanagawa Dental University, Kanagawa, Japan
2Department of Dental Anaesthesiology, Faculty of Dental Science, Kyushu University, Fukuoka, Japan
3Department of Health and Medical Engineering School of Science and Engineering, Kokushikan University, Tokyo, Japan
4Department of Dental Anaesthesiology, Institution of Biomedical Sciences, Tokushima University Graduate School, Tokushima, Japan
- *Corresponding Author:
- Shigeki Fujiwara
Department of Anaesthesiology
Graduate School of Dentistry
Kanagawa Dental University, Japan
Accepted on January 24, 2017
Aim: In our previous study, we demonstrated that the vasoconstrictive action of lidocaine occurs at a concentration of 10-4 mol/L. Furthermore, we found that lidocaine enhanced contractile responses produced by low concentrations of adrenaline (10-8-10-7 mol/L). In this study, the responses of isolated rat thoracic aorta preparations to local anaesthetic solutions containing either prilocaine or mepivacaine were examined in the presence of adrenaline or noradrenaline.
Methods: We isolated thoracic aorta from Wister rats. The arteries were cut into ~3 mm long rings that were stretched by a pair of hooks in an organ bath filled with Krebs-Henseleit solution. After 1 μg/ml lipopolysaccharide treatment, vasoconstrictors (either adrenaline or noradrenaline) were applied in a cumulative manner between concentrations of 10-9–10-5 mol/L of either prilocaine or mepivacaine (10-4 mol/L). Changes in isometric vasocontractions were continuously recorded with an amplifier system using the PCD-30A computer system.
Results: The contractile response to both prilocaine and mepivacaine significantly decreased at low concentrations of adrenaline (10-8-10-7 mol/L). The contractile response to mepivacaine also significantly decreased at low concentrations of adrenaline (10-9-10-8 mol/L). In contrast, with the exception of prilocaine at a low concentration of adrenaline (10-8 mol/L), neither prilocaine nor mepivacaine significantly decreased the contractile responses. In a model of blood vessel inflammation under 6 h lipopolysaccharide treatment, prilocaine and mepivacaine enhanced contractile responses produced by 10-9-10-7 mol/L noradrenaline.
Conclusion: Noradrenaline should be administered when injecting inflamed tissues with prilocaine or mepivacaine.
Keywords
Lipopolysaccharide, Mepivacaine, Prilocaine, Vasoconstrictors.
Introduction
Local anaesthetic administration in acutely inflamed tissues often fails to achieve satisfactory analgesia. The effects of low pH and vasodilation in the inflamed area are among some of the hypotheses that have been proposed to explain this phenomenon [1]. Vasodilation can increase local blood flow, resulting in the rapid removal of local anaesthetic from the injection site. In order to prolong the duration of anesthesia, vasoconstrictors are typically administered with local anaesthetics; however, their effects (when combined with local anaesthetics) on dilated vessels in inflamed tissues are poorly understood. In our previous study, we indicated that lidocaine partially increased contractile responses produced by low concentrations of 10-8 mol/L adrenaline in the aorta treated with Lipopolysaccharide (LPS) [2]. Two local anaesthetic agents in the amide class, prilocaine and mepivacaine, are often administered in dental treatment. The contractile responses of inflammatory vessels to Adrenaline (AD) and Noradrenaline (NA), combined with prilocaine and mepivacaine, have not been fully investigated.
Therefore, to investigate the effects of vasoconstrictors and local anaesthetics on inflamed vessels, we measured the contractile responses of inflamed rat thoracic aortas to AD or NA administered with or without prilocaine or mepivacaine.
Materials and Methods
Animals
Sixteen 6-8 weeks-old male Wistar rats were used in the experiments. The study protocol was reviewed and approved by the Institutional Animal Care Committee of Asahi University (Gifu, Japan).
Functional experiments
Rats were anesthetized via inhalation of sevoflurane and killed via decapitation. Thoracic aortas were then isolated for functional experimentation, and 3-mm rings were carefully prepared from the thoracic aortas using a dissecting microscope, as previously described [2-4]. Thoracic aorta rings were placed in Krebs-Henseleit solution (KRB; pH 7.4) containing 118 mmol/L NaCl, 4.7 mmol/L KCl, 25 mmol/L NaHCO3, 1.2 mmol/L KH2PO4, 1.2 mmol/L MgSO4, 2.5 mmol/L CaCl2, and 11.5 mmol/L glucose. Each ring was carefully suspended in an organ chamber containing 5 ml KRB bubbled with 95% O2/5% CO2 at 37°C, and the changes in tension were recorded isometrically. A resting tension of 1.0 g was applied, and the rings were allowed to equilibrate for 60 min, with readjustment of the passive tension when required. During this period, the rings were washed every 20 min with fresh bubbled and warmed KRB. Changes in isometric vasocontractions were recorded continuously using an amplifier system and the PCD-30A computer system (KYOWA, Tokyo, Japan) [2]. Vasoconstrictions were quantified as the contractile force (mg) divided by the wet tissue weight (mg). These experimental methods were developed based on the methods reported by Yoshida et al. and Kobayashi et al. [5,6].
LPS treatment
The rings were incubated with KRB containing 1 μg/ml LPS at 37°C for 6 h, and AD and NA were applied in a cumulative manner (10-9 mol/L-10-5 mol/L), with or without prilocaine and mepivacaine (10-4 mol/L).
Chemicals
AD, NA, prilocaine, and mepivacaine were purchased from Sigma (St. Louis, MO, USA), and LPS was purchased from Invitrogen (CA, Carlsbad, USA). All other reagents were of analytical grade.
Statistical analysis
All data were expressed as mean ± standard error. The Mann- Whitney U test was used to compare two groups, while the Steel-Dwass test was used to compare several different groups. All analyses were performed using SPSS software (version 16.0; SPSS Inc., Chicago, IL) and Ekuseru-Toukei 2006 software (Social Survey Research Information Co. Ltd., Japan), and P-values<0.05 were considered statistically significant.
Results
Contractile responses of non-LPS-treated aortas to AD and NA with or without prilocaine
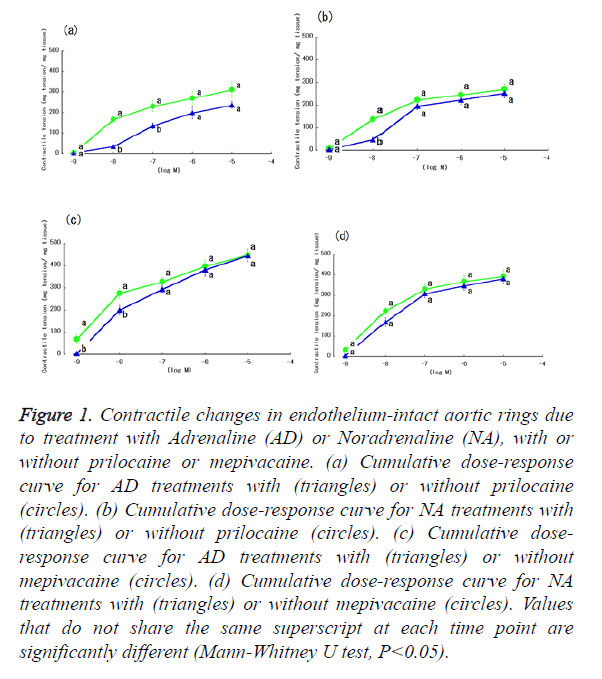
Aortic ring contractile responses to varying concentrations of AD or NA in non-LPS treatment, with or without prilocaine, are shown in Figures 1a and 1b. Gradual increases in AD and NA concentration produced gradual responses in the isolated rat aortas, with the greatest response observed at 10-5 mol/L. Both AD and NA evoked concentration-dependent contractile responses. Figures 1a and 1b show aortic ring contractile responses to varying concentrations of AD or NA in the presence of prilocaine and without LPS treatment. Similar to the experiment without prilocaine, aortic contractile responses in these conditions were the greatest at 10-5 mol/L. The addition of prilocaine (10-4 mol/L) created a small but significant (P<0.05) attenuation in contractions induced at 10-8-10-7 mol/L AD (Figure 1a) and 10-8 mol/L NA (Figure 1b).
Figure 1. Contractile changes in endothelium-intact aortic rings due to treatment with Adrenaline (AD) or Noradrenaline (NA), with or without prilocaine or mepivacaine. (a) Cumulative dose-response curve for AD treatments with (triangles) or without prilocaine (circles). (b) Cumulative dose-response curve for NA treatments with (triangles) or without prilocaine (circles). (c) Cumulative doseresponse curve for AD treatments with (triangles) or without mepivacaine (circles). (d) Cumulative dose-response curve for NA treatments with (triangles) or without mepivacaine (circles). Values that do not share the same superscript at each time point are significantly different (Mann-Whitney U test, P<0.05).
Contractile responses of non-LPS-treated aortas to AD and NA in the presence of prilocaine
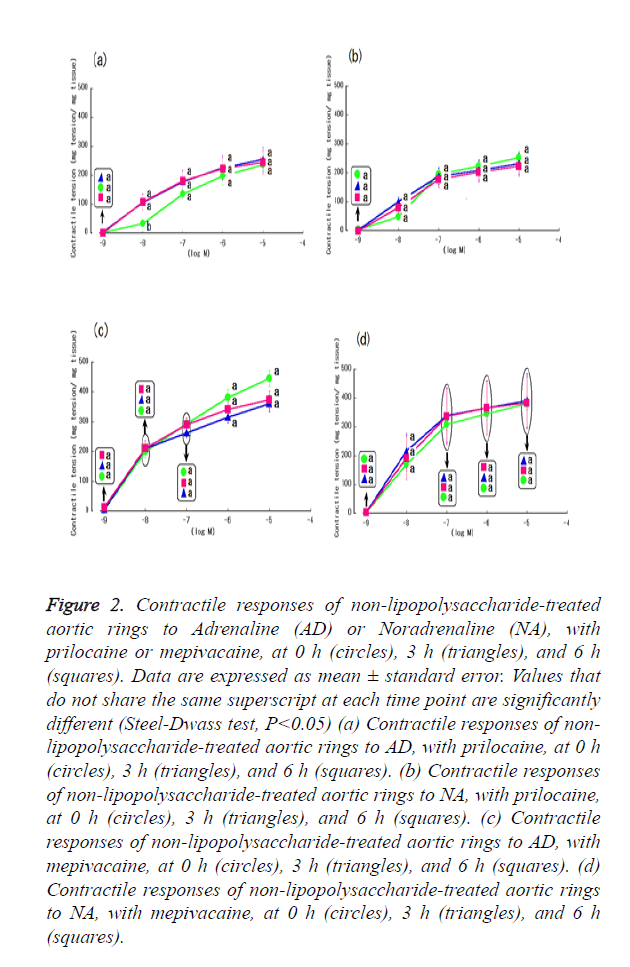
Contractile responses to AD or NA with 6 h prilocaine treatment and without LPS treatment are shown in Figures 2a and 2b. Although prilocaine did not reduce non-LPS-treated aortic ring contractile responses to high concentrations of either AD or NA (10-5 mol/L) after 0, 3, and 6 h prilocaine treatment, it significantly reduced responses (P<0.05) at low concentrations of AD (10-8 mol/L) without prilocaine treatment (Figure 2a). In contrast, the contractile response in response to prilocaine was not decreased at low concentrations of AD (10-8 mol/L) (Figure 2b).
Figure 2. Contractile responses of non-lipopolysaccharide-treated aortic rings to Adrenaline (AD) or Noradrenaline (NA), with prilocaine or mepivacaine, at 0 h (circles), 3 h (triangles), and 6 h (squares). Data are expressed as mean ± standard error. Values that do not share the same superscript at each time point are significantly different (Steel-Dwass test, P<0.05) (a) Contractile responses of non-lipopolysaccharide- treated aortic rings to AD, with prilocaine, at 0 h (circles), 3 h (triangles), and 6 h (squares). (b) Contractile responses of non-lipopolysaccharide-treated aortic rings to NA, with prilocaine, at 0 h (circles), 3 h (triangles), and 6 h (squares). (c) Contractile responses of non-lipopolysaccharide-treated aortic rings to AD, with mepivacaine, at 0 h (circles), 3 h (triangles), and 6 h (squares). (d) Contractile responses of non-lipopolysaccharide-treated aortic rings to NA, with mepivacaine, at 0 h (circles), 3 h (triangles), and 6 h (squares).
Contractile responses of LPS-treated aortas to AD and NA in the presence of lidocaine
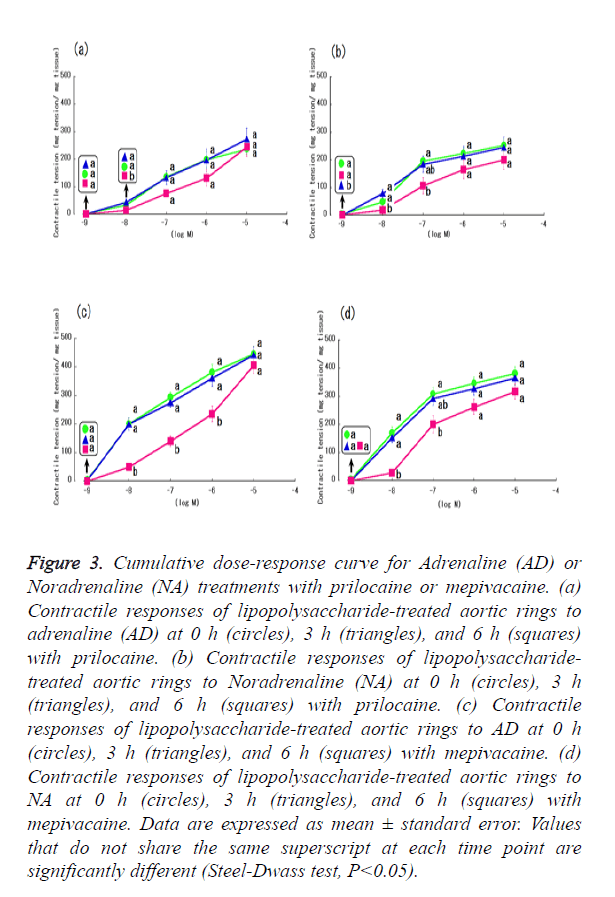
Figures 3a and 3b show LPS-treated aortic ring time-dependent contractile responses to AD or NA. AD treatment at a concentration of 10-8 mol/L resulted in significant differences after 6 h prilocaine treatment (Figure 3a). However, no significant differences (P>0.05) in responses over time were observed with AD concentrations of 10-9 mol/L and 10-7-10-5 mol/L (Figure 3a). In contrast, NA treatment at 10-8 and 10-7 mol/L significantly reduced (P<0.05) the effects of 6 h prilocaine treatment (Figure 3b). Moreover, at a concentration of 10-7 mol/L, contractile responses to 3 h prilocaine treatment were significantly reduced (Figure 3b).
Figure 3. Cumulative dose-response curve for Adrenaline (AD) or Noradrenaline (NA) treatments with prilocaine or mepivacaine. (a) Contractile responses of lipopolysaccharide-treated aortic rings to adrenaline (AD) at 0 h (circles), 3 h (triangles), and 6 h (squares) with prilocaine. (b) Contractile responses of lipopolysaccharide-treated aortic rings to Noradrenaline (NA) at 0 h (circles), 3 h (triangles), and 6 h (squares) with prilocaine. (c) Contractile responses of lipopolysaccharide-treated aortic rings to AD at 0 h (circles), 3 h (triangles), and 6 h (squares) with mepivacaine. (d) Contractile responses of lipopolysaccharide-treated aortic rings to NA at 0 h (circles), 3 h (triangles), and 6 h (squares) with mepivacaine. Data are expressed as mean ± standard error. Values that do not share the same superscript at each time point are significantly different (Steel-Dwass test, P<0.05).
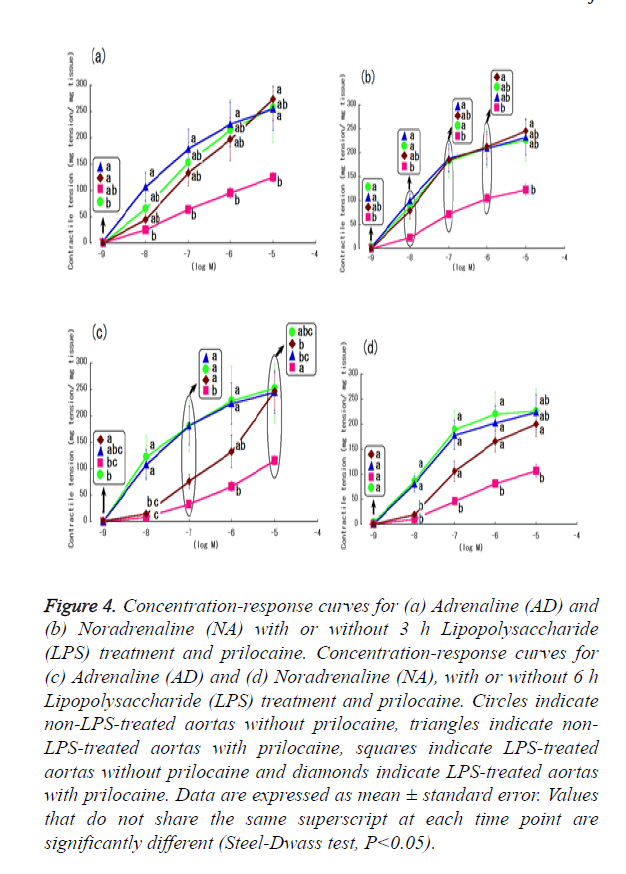
Contractile responses of aortas to AD and NA according to prilocaine and 3 h LPS treatment
Contractile responses to AD or NA, with or without 3 h LPS treatment and prilocaine are shown in Figures 4a and 4b. Prilocaine did not reduce non-LPS-treated aortic ring contractile responses to any of the examined concentrations of AD and NA (10-9-10-5 mol/L). In contrast, prilocaine with LPS-treatment partially increased aortic ring contractile responses to low concentrations of NA (10-7 mol/L) (Figure 4b).
Figure 4. Concentration-response curves for (a) Adrenaline (AD) and (b) Noradrenaline (NA) with or without 3 h Lipopolysaccharide (LPS) treatment and prilocaine. Concentration-response curves for (c) Adrenaline (AD) and (d) Noradrenaline (NA), with or without 6 h Lipopolysaccharide (LPS) treatment and prilocaine. Circles indicate non-LPS-treated aortas without prilocaine, triangles indicate non- LPS-treated aortas with prilocaine, squares indicate LPS-treated aortas without prilocaine and diamonds indicate LPS-treated aortas with prilocaine. Data are expressed as mean ± standard error. Values that do not share the same superscript at each time point are significantly different (Steel-Dwass test, P<0.05).
Contractile responses of aortas to AD and NA according to prilocaine and 6-h LPS treatment
Contractile responses to AD or NA with or without 6 h LPS treatment and prilocaine are shown in Figures 4c and 4d. Prilocaine did not reduce non-LPS-treated aortic ring contractile responses to any of the examined concentrations of AD and NA. In contrast, with LPS-treatment, prilocaine partially increased the contractile responses of the aortic rings to high concentration of AD and NA (10-5 mol/L), in particular at 10-7 mol/L AD (Figures 4c and 4d).
Contractile responses of non-LPS-treated aortas to AD and NA with or without mepivacaine
Aortic ring contractile responses to varying concentrations of AD or NA, in non-LPS treatment with or without mepivacaine, are shown in Figures 1c and 1d (circles). Gradual increases in AD and NA concentrations produced gradual responses in the isolated rat aortas, with the greatest response observed at concentrations of 10-5 mol/L. Both AD and NA evoked concentration-dependent contractile responses. Figures 1c and 1d (triangles) present aortic ring contractile responses to varying concentrations of AD or NA in the presence of mepivacaine and without LPS treatment. Similar to the experiment without mepivacaine, aortic contractile responses in these conditions were greatest at concentrations of 10-5 mol/L. The addition of mepivacaine (10-4 mol/L) created a small but significant (P<0.05) attenuation in contractions that were induced at 10-9-10-8 mol/L of AD (Figure 1c).
Contractile responses of non-LPS-treated aortas to AD and NA in the presence of mepivacaine
Contractile responses to AD or NA without LPS with 6 h mepivacaine immersion are shown in Figures 2c and 2d. Mepivacaine did not reduce non-LPS-treated aortic ring contractile responses to any concentration of AD and NA at 0, 3, or 6 h mepivacaine immersion (Figures 2c and 2d).
Contractile responses of LPS-treated aortas to AD and NA in the presence of mepivacaine
Figures 3c and 3d show LPS-treated aortic ring time-dependent contractile responses to AD or NA. AD treatment at concentrations of 10-8-10-6 mol/L resulted in significant differences following 6 h mepivacaine immersion (Figure 3c). However, no significant differences in responses over time were observed at AD concentrations of 10-9 and 10-5 mol/L (Figure 3c). In contrast, NA treatment at concentrations of 10-8-10-7 mol/L was significantly reduced with 6 h mepivacaine immersion (Figure 3d).
Contractile responses of aortas to AD and NA according to mepivacaine and 3-h LPS treatment
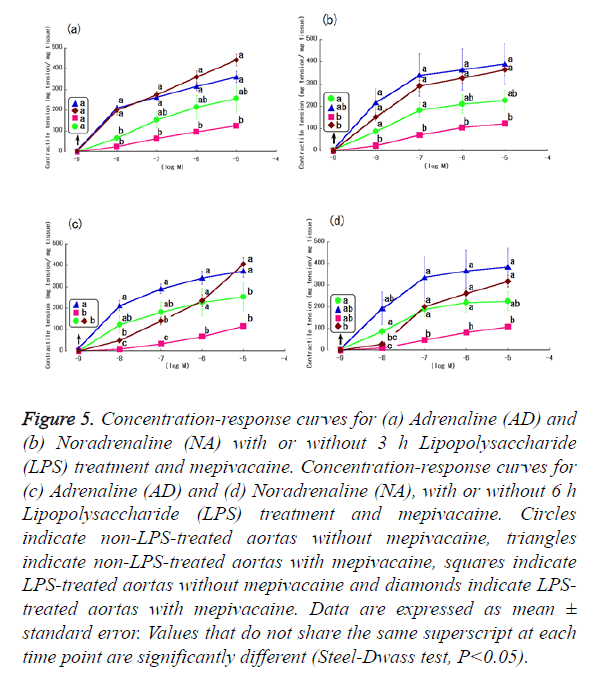
Contractile responses to AD or NA with or without 3 h LPS treatment and mepivacaine are shown in Figures 5a and 5b. Mepivacaine did not reduce non-LPS-treated aortic ring contractile responses to any of the examined concentrations of NA (10-9-10-5 mol/L) (Figure 5b). In addition, with non-LPS-treatment, mepivacaine partially increased the contractile responses of the aorta rings to low concentrations of AD (10-8 mol/L) (Figure 5a).
Figure 5. Concentration-response curves for (a) Adrenaline (AD) and (b) Noradrenaline (NA) with or without 3 h Lipopolysaccharide (LPS) treatment and mepivacaine. Concentration-response curves for (c) Adrenaline (AD) and (d) Noradrenaline (NA), with or without 6 h Lipopolysaccharide (LPS) treatment and mepivacaine. Circles indicate non-LPS-treated aortas without mepivacaine, triangles indicate non-LPS-treated aortas with mepivacaine, squares indicate LPS-treated aortas without mepivacaine and diamonds indicate LPS-treated aortas with mepivacaine. Data are expressed as mean ± standard error. Values that do not share the same superscript at each time point are significantly different (Steel-Dwass test, P<0.05).
In contrast, mepivacaine with LPS treatment increased aortic ring contractile responses to 10-8-10-5 mol/L concentrations of both AD and NA (Figures 5a and 5b).
Contractile responses of aortas to AD and NA according to mepivacaine and 6-h LPS treatment
Contractile responses to AD or NA with or without 6 h LPS treatment and mepivacaine are shown in Figures 5c and 5d.
Mepivacaine did not reduce non-LPS-treated aortic ring contractile responses to any of the examined concentrations of AD and NA. In addition, with non-LPS-treatment, mepivacaine partially increased the contractile responses of the aortic rings to a high concentration of AD (10-5 mol/L).
In contrast, mepivacaine increased LPS-treated aortic ring contractile responses to 10-8-10-5 mol/L of AD and 10-7-10-5 mol/L of NA. However, the differences in responses were not significant (P>0.13) at the lowest concentration of AD (10-9 mol/L) or NA (10-9-10-8 mol/L) (Figures 5c and 5d).
Discussion
In this study, we utilized a LPS-induced aortic inflammation model and evaluated alterations in aortic ring contractile responses to AD or NA, in the presence or absence of prilocaine and mepivacaine. Our findings reveal that the contractility evoked by AD and NA was partially maintained in the presence of both prilocaine and mepivacaine (although responses to both vasoconstrictors decreased after 6 h of LPS treatment). LPS treatment is believed to reduce vessel contractile responses through increased expression of inducible Nitrous Oxide Synthase (iNOS) in the vascular smooth muscle, or through the massive production of Nitrous Oxide (NO) in the vascular endothelium [7-9]. Assuming that this hypothesis is correct, our data indicate that iNOS expression reaches a maximum within 6 h after administering LPS. Therefore, AD and NA with prilocaine or mepivacaine may help modulate LPS-induced effects on iNOS/NO in inflamed aortas, and thereby preserve contractile response in these tissues. Although aorta vasoconstrictive responses to low concentrations of AD and NA with prilocaine or mepivacaine were not significantly different after 6 h of LPS treatment, the response was partially preserved in the presence of prilocaine or mepivacaine.
Local anaesthetics have an antioxidant action [10]. Vascular responsiveness recovery is expected in response to oxidation material produced by LPS, as a form of antioxidant action. The results of the present study support this hypothesis Furthermore, mepivacaine is expected to produce a vasoconstriction action such as non-inflammation; this is also supported by our findings, although the reasons for this are unclear. However, Takaishi and Kitahata et al. published in vitro results indicating that the inhibitory effects of local anesthesia (e.g., procaine and lidocaine) on NO production were partially due to suppression of L-arginine uptake [11].
Lidocaine is known to constrict vessels at low concentrations and relax vessels at high concentrations [12-14]. In our previous study, lidocaine at a concentration of 10-4 mol/L had a minor effect on the observed contractile response to AD, the vasoconstrictive action of lidocaine itself may have been involved [2]. In the present study, prilocaine and mepivacaine did not result in a vasoconstrictor response compared with nonprilocaine and non-mepivacaine. Prilocaine significantly decreased contractile responses to low concentrations of AD (10-8-10-7 mol/L), as did mepivacaine (to 10-9-10-8 mol/L of AD). In addition, prilocaine significantly decreased contractile responses to a low concentration of NA (10-8 mol/L). Mepivacaine did not significantly decrease their contractile responses to any examined concentration of NA. In previous study, it was reported that a low-concentration of lidocaine and prilocaine induced vasoconstriction responses to AD, but did not influence vasoconstriction responses to NA [15]. Our present study also indicated that vasoconstriction response to AD was strongly maintained in comparison with NA and prilocaine. This tendency was particularly evident with mepivacaine.
This study has several limitations. First, we used rat thoracic aortic rings, which were not under the control of the autonomic nervous system. However, it is thought that peripheral vessels (arterial/venous) are sufficiently contracted under local anesthesia with 1:80,000-200,000 AD injected into rat and human local tissue [2,16,17]. Second, the pH within inflamed tissues is known to be<7.4; however, the present results were obtained at a pH of 7.4 [1]. Third, we administered prilocaine and mepivacaine at a concentration of 10-4 M, which is approximately equivalent to 0.01%, because it was the maximum concentration at which the contractile response of the rat aortas did not disappear (data not shown). Fourth, we tested endothelium-dependent vasorelaxation in vessels that were preconstricted using phenylephrine, based on the response to the muscarinic receptor agonist (acetylcholine) [18,19]. Consequently, we did not measure NO concentrations in the present study; this parameter should therefore be evaluated in future studies. Fifth, we used rat thoracic aortas; generally, the vasopressor added in a local anaesthetic acts on micro vessels. It would have been valuable to examine this mechanism for the arteries around the oral cavity, although these specific arteries have not been evaluated in detailed studies. Therefore, we used rat aortas in the present study because these have been used in numerous other model-based studies and their properties are clearly understood. Sixth, since this was a model-based study, it is unclear whether our results will be reflected in the real clinical situation. Further studies are needed to evaluate our findings in the clinical setting (e.g., for the inferior alveolar artery and lingual artery). In addition, it may have not been possible to completely reproduce an inflammatory state in vivo because this inflammatory state was caused by LPS treatment in vitro. Therefore, an established experimental system using in vivo micro vessels is necessary in future studies.
In conclusion, we utilized a model of LPS-induced vessel inflammation to test the effects of AD or NA administered with or without prilocaine and mepivacaine. Our results indicate that LPS-treated vessels’ contractile responses to NA of 10-7-10-5 mol/L significantly increased in the presence of prilocaine and mepivacaine. Therefore, we conclude that NA is the optimal vasoconstrictor for prolonging prilocaine and mepivacaine-induced analgesic effects in inflamed tissues.
Acknowledgements
A part of this study was presented at the 56th Annual Meeting of Japan Society of Anaesthesiology (Kobe, Japan, August 2009). We thank Editage for editing the manuscript. Asahi University provided financial support.
References
- Punnia-Moorthy A. Evaluation of pH changes in inflammation of the subcutaneous air pouch lining in the rat, induced by carrageenan, dextran and Staphylococcus aureus. J Oral Pathol 1987; 16: 36-44.
- Fujiwara S, Noguchi A, Tsukamoto M, Ito S, Imaizumi U, Morimoto Y, Yoshida KI, Yokoyama T. The effect of adrenaline or noradrenaline with or without lidocaine on the contractile response of lipopolysaccharide-treated rat thoracic aortas. Biomed Res 2016; 27: 453-457.
- Takakura K, Xiaohong W, Takeuchi K, Yasuda Y, Fukuda S. Deactivation of norepinephrine by peroxynitrite as a new pathogenesis in the hypotension of septic shock. Anesthesiology 2003; 98: 928-934.
- Takakura K, Mizogami M, Fukuda S. Protamine sulfate causes endothelium-independent vasorelaxation via inducible nitric oxide synthase pathway. Can J Anaesth 2006; 53: 162-167.
- Yoshida K, Okabe E. Selective impairment of endothelium-dependent relaxation by sevoflurane: oxygen free radicals participation. Anesthesiology 1992; 76: 440-447.
- Kobayashi Y, Yoshida K, Noguchi M, Wakasugi Y, Ito H, Okabe E. Effect of enflurane on contractile reactivity in isolated canine mesenteric arteries and veins. Anesth Analg 1990; 70: 530-536.
- Julou-Schaeffer G, Gray GA, Fleming I, Schott C, Parratt JR, Stoclet JC. Loss of vascular responsiveness induced by endotoxin involves L-arginine pathway. Am J Physiol 1990; 259: 1038-1043.
- Busse R, Mulsch A. Induction of nitric oxide synthase by cytokines in vascular smooth muscle cells. FEBS Lett 1990; 275: 87-90.
- Vo PA, Lad B, Tomlinson JA, Francis S, Ahluwalia A. Autoregulatory role of endothelium-derived nitric oxide (NO) on lipopolysaccharide-induced vascular inducible NO synthase expression and function. J Biol Chem 2005; 280: 7236-7243.
- Zimmerman JJ. Redox/radical repertoire rapport: pathophysiology and therapeutics. Acta Anaesthesiol Scand 1998; 42: 1-3.
- Takaishi K, Kitahata H, Kawahito S. Local anaesthetics inhibit nitric oxide production and L-arginine uptake in cultured bovine aortic endothelial cells. Eur J Pharmacol 2013; 704: 58-63.
- Johns RA, DiFazio CA, Longnecker DE. Lidocaine constricts or dilates rat arterioles in a dose-dependent manner. Anesthesiology 1985; 62: 141-144.
- Turan NN, Demiryürek AT, Celebi H. Effects of lidocaine on rabbit isolated thoracic aorta. Pharmacol Res 2000; 42: 453-458.
- Jernbeck J, Samuelson UE. Effects of lidocaine and Calcitonin Gene-Related Peptide (CGRP) on isolated human radial arteries. J Reconstr Microsurg 1993; 9: 361-365.
- Gerke DC, Frewin DB, Waterson JG. The effects of commercial local anaesthetic solutions on the isolated rabbit ear artery. Aust Dent J 1977; 22: 289-294.
- Shoroghi M, Sadrolsadat SH, Razzaghi M, Farahbakhsh F, Sheikhvatan M, Sheikhfathollahi M, Abbasi A. Effect of different epinephrine concentrations on local bleeding and hemodynamics during dermatologic surgery. Acta Dermatovenerol Croat 2008; 16: 209-214.
- Chen YW, Tzeng JI, Pan HJ, Hung CH, Chen YC, Wang JJ. Co-administration of memantine with epinephrine produces a marked peripheral action in intensifying and prolonging analgesia in response to local skin pinprick in rats. Neurosci Lett 2014; 574: 59-63.
- Iaccarino G, Ciccarelli M, Sorriento D, Cipolletta E, Cerullo V. AKT participates in endothelial dysfunction in hypertension. Circulation 2004; 109: 2587-2593.
- Santulli G, Wronska A, Uryu K, Diacovo TG, Gao M, Marx SO, Kitajewski J, Chilton JM, Akat KM, Tuschl T, Marks AR, Totary-Jain HJ. A selective microRNA-based strategy inhibits restenosis while preserving endothelial function. Clin Invest 2014; 124: 4102-4114.