ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2022) Volume 33, Issue 6
Effect on ischemia modified albumin in lipitensive patients.
Kuldip Singh*
Department of Biochemistry, Government Medical College, Patiala, Punjab, India
- Corresponding Author:
- Kuldip Singh
Department of Biochemistry
Government Medical College
Patiala
Punjab
Accepted date: August 24, 2022
Background: Lipitensive are well established leading causes of morbidity and mortality worldwide. A prompt diagnosis and treatment of lipitensive is pivotal for a better health care. Albumin is the most important protein synthesized by the liver. Posttranscriptional changes occur in the molecular structure of albumin due to various factors and isoforms arise. Ischemic Modified Albumin (IMA) is one such isoform.
Aim: The aim of the study was to evaluate the changes in serum ischemia modified albumin in lipitensive patients.
Materials and Methods: 30 lipitensive patients (study group) and equal number of healthy normal subjects as a control group were recruited from the rural and urban community of Punjab origin after taken prior consent of participants. After overnight fasting, venous blood samples were taken from lipitensive and healthy control subjects for the estimation of ischemia modified albumin along with complete lipid profile, fasting glucose and HbA1C levels.
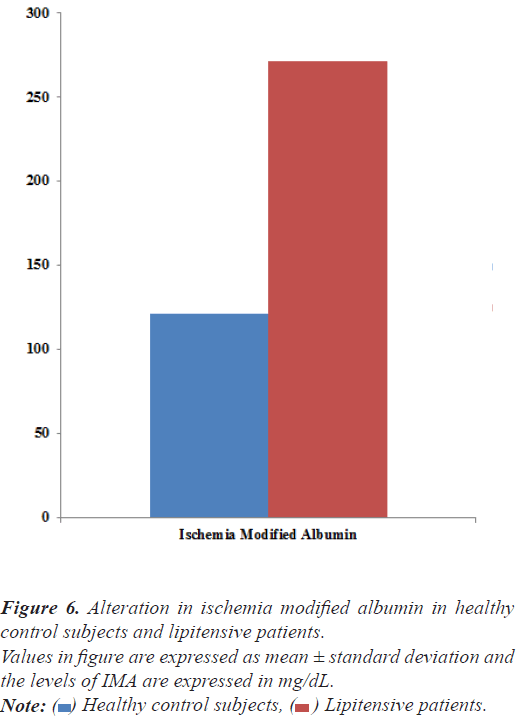
Results: IMA was significantly increased from 121.15 ± 19.36 μM/L to 277.67 ± 21.98 μM/L by 129.19% in lipitensive patients in comparison to healthy normal subjects.
Conclusion: A progressive enhancement in serum IMA level suggested that IMA as a sensitive and early biomarker might be useful for optimal treatment of the lipitensive patients.
Keywords
Hypertension, Hyperlipidemia, Lipitension, Ischemia Modified Albumin (IMA).
Introduction
A cardiovascular disease like atherosclerosis Acute Myocardial Infarction (AMI) is the major cause of death all over the world. The most common symptom of AMI The most common symptoms of AMI are pain in the chest, back, jaw, and other areas of the upper body that lasts more than a few minutes or that goes away and comes back, shortness of breath, sweating, nausea, vomiting, anxiety, feeling like you’re going to faint, a fast heart rate and sense of impending doom etc. Chest pain is the most commonly reported symptom among both women and men. However, women are a bit more likely than men to have more of the “atypical” symptoms, such as shortness of breath, jaw pain, upper back pain, lightheadedness, nausea, vomiting. In fact, some women who have had a heart attack report that their symptoms felt like the symptoms of the flu [1,2].
The patients suffering with symptoms of acute MI are currently assessed by performing myoglobin, cardiac troponins-T, troponins-I, creatine kinase, and lactate dehydrogenase in clinical practice. These usual biomarkers are sensitive and specific for the detection of myocardial necrosis, an increase occurs approximately 3 to 6 hours after the onset of myocardial cell injury. Therefore, patients could wait before they are diagnosed and treated in the emergency room [3,4].
Recently, biochemical biomarkers used to detect myocardial ischemia like ischemia-modified albumin, soluble CD- 40 ligand; fatty acid binding protein, myeloperoxidase, choline and cystatin C are currently being evaluated in the setting of acute myocardial infarction. IMA is the most thoroughly investigated markers among these new markers [5,6].
It has been observed that the affinity of the N-terminus of human albumin for cobalt is reduced in the setting of acute myocardial ischemia with detectable changes in binding. Interestingly, these changes are occurring within minutes. The sensitivity of IMA is 83% in myocardial ischemia during the very early period of ischemia and its high negative predictive value i.e. 96% make IMA a promising marker for the immediate detection of ischemia before myocardial necrosis.
The pursuit of new markers is rapidly progressing, which markers will become clinically useful depends on several factors, including clinical efficacy, assay availability and cost-effectiveness. So, the present study was designed to evaluate the ischemia Modified Albumin (IMA) along with complete lipid profile like total cholesterol, triacylglycerol, HDL-Cholesterol, LDL-Cholesterol, VRDL-Cholesterol and free fatty acids, fasting glucose and HbA1C in patients with hypertensive patients.
Materials and Methods
Study and selection criteria
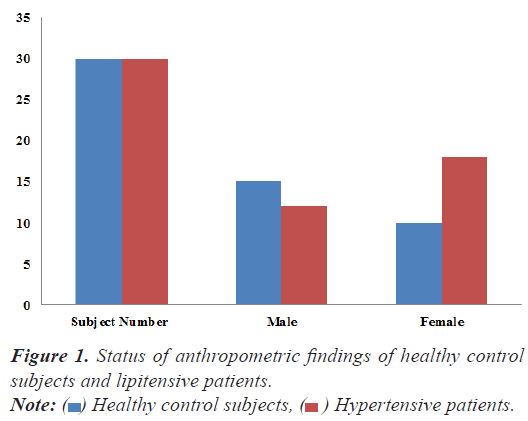
A total of 30 hypertensive patients suffering with hyperlipidemia and equal number (n=30) of healthy normal subjects of both gender (Male and Female) were recruited from the rural and urban society of Punjab region in the study. The lipitensive patients were recruited on the bases of their raised systolic and diasystolic blood pressure i.e. above 180/90 mm Hg with hyperlipidemia (Figure 1).
Inclusion criteria
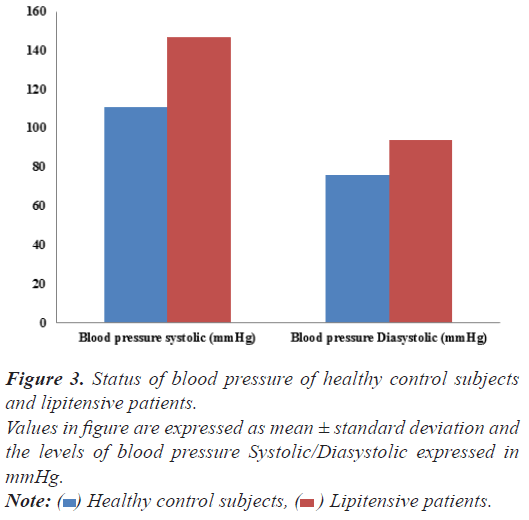
All subjects recruited for the study were vegetarian, non-smokers and non-alcoholic, with no positive family history of non-communicable chronic diseases like diabetes, arthritis, Cardiovascular Diseases (CVD) etc. Data was obtained from subjects using an interviewer- based questionnaire where the detailed information on their lifestyle, medical history, diet etc. and after obtaining the consent from the patients and their relatives attending the patients were considered for the study. Blood Pressure was measured 3 times a day in sitting position, using a mercurial sphygmomanometer and appropriately sized cuffs on the right arm after a resting period of 5 min.
Exclusion criteria
The patients on medication that can influence the results of the study, the presence of the metabolic disorders (diabetes, obesity), renal and neurological pathologies, acute and chronic inflammatory processes etc., are excluded from the study.
Study design
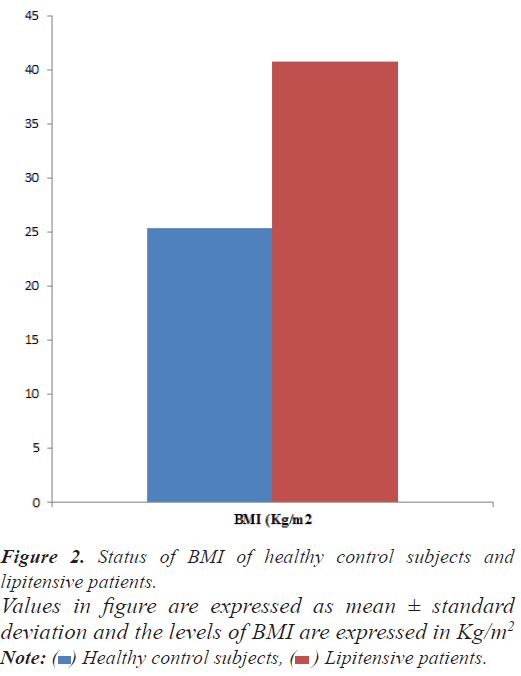
This study was a case control cross-sectional prospective study. A detailed history, physical and systemic examination including measurement of height, weight, heart rate, blood pressure in the sitting position, Body Mass Index (BMI), fasting glucose along with HbA1C and Ischemia Modified Albumin (IMA) and Ischemia Modified Albumin: Albumin Ratio (IMAR) of every patient/subject was recorded who entered the study (Figure 2).
Data collection
Measurements of anthropometric parameters: Height (meter) and Weight (kg) were measured while subjects were wearing light clothing without shoes. The Body Mass Index (BMI) was calculated by the formula weight (Kg)/ height (m2). The Blood Pressure (BP) was measured in the sitting position using a mercurial sphygmomanometer and appropriate cuff size on the right arm after a resting period of 5 min.
Specimen collection, specimen (serum/plasma) preparation and storage: A volume of 5 ml of peripheral venous blood was collected by vein puncture using a dry, disposable syringe between 8 and 9 AM after an overnight fast from both groups (Control and PCOS subjects) in potassium oxalate and sodium fluoride vial (2 ml) and plain (3 ml) vial. The blood of potassium oxalate and sodium fluoride vial was immediately centrifuged at 4000 rpm for 10 minutes for the preparation of plasma and the blood collected in plain vial was kept at 37°C for half an hour after that the blood samples were centrifuged at 4000 rpm for 15 minutes for the separation of serum. The plasma and serum was used for various biochemical assays as under
Biochemical assays
Estimation of glucose: Glucose was estimated spectrophotometrically using an enzymatic test kit base by the method based on GOD-POD method supplied by Transasia Bio-Medicals Ltd. Solan (HP); in technical collaboration with ERBA diagnostic Mannheim, Germany.
Estimation of Glycosylated Hemoglobin (HbA1C): HbA1C was analyzed by using kit supplied by Transasia Bio-medicals Ltd. Solan (HP); in Technical collaboration with ERBA agnostic Mannheim, Germany based onion- exchange resin method in which a hernolyzed preparation of the whole blood is mixed continuously for 5 ruin with a weak binding cation exchanges resin. During this time, non-HbAlc binds to the resin. After the mixing period a filter is used to separate the supernatant containing the glycohemoglobin from the resin. The glycohemoglobin percent is determined by measuring the absorption at 415 nm of the glycohemoglobin fraction and the total hemoglobin fraction. The ratio of the two absorbances gives the percentage glycohemoglobin.
Estimation of lipid profile: The total cholesterol, triglyceride, high density lipoprotein cholesterol, were analyzed by using commercial available kits procured from Transasia Biomedical Private Limited, Mumbai (India). Low density lipoprotein-cholesterol levels were estimated by the primary measurements by using the empirical equation of Bates and Warren, 1989 [7].

Estimation of albumin: Albumin in urine was measured using standardized albumin kit supplied by Transasia Bio- Medicals Ltd. Solan (HP); in Technical collaboration with ERBA diagnostic Mannheim, Germany.
Estimation of Ischemia Modified Albumin (IMA): IMA measurements were done by Albumin Cobalt Binding (ACB) test. In this test, Cobalt (Co) is added to the serum sample to measure the binding capacity of albumin. Free cobalt is stained with a protein named Dithiothreitol (DTT) and spectrophotometric measurements are done. DTT cannot react with the albumin that binds to Co. As a consequence, the free Co amount also reflects the IMA level [8]. Serum IMA measurements were performed as follows: 50 μL of 1 g/L cobalt chloride solution was added to 200 μL of patient serum and kept at room temperature for 10 min after a gentle shake. Then 50 μL of 1.5 g/L DTT solution was added and mixed. After 2 min, 1 mL of 9.0 g/L NaCl solution was added. Absorbances of test mixtures were measured at 470 nm by a spectrophotometer and calorimetric method. Results were obtained in approximately 30 min and reported as Absorbance Units (ABSU).
Statistical analysis
The data was expressed as Mean ± SD and analyzed with the SPSS 16.0.7 statistical software package. Differences between the lipitensive and healthy control subjects were evaluated using the Student’s independent samples “t” test. Differences were considered statistically significant at P<0.05.
Results
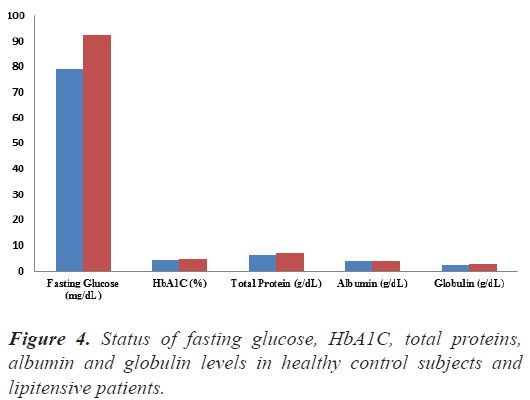
Fasting glucose and HbA1C: The results of fasting glucose and HbA1C are summarized in Figure 3. A nominal increase was observed in the plasma fasting glucose (from 79.19 ± 4.17 mg/dL to 92.32 ± 9.88 mg/ dL) and HbA1C (from 4.30 ± 0.45% to 4.89 ± 1.72%) levels by 16.58% and 13.72% respectively in hypertensive patients with respect to healthy control subjects.
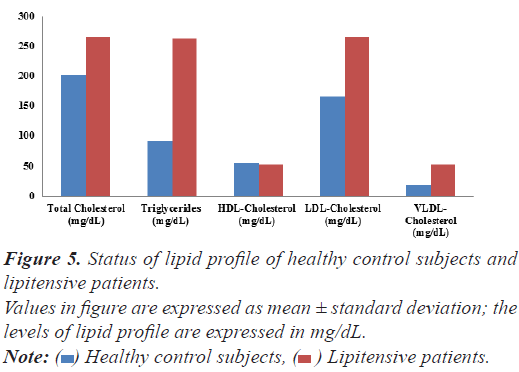
Lipid profile: The serum total cholesterol, TG and LDL-cholesterol and very-LDL-cholesterol level were significantly increased in hypertensive patient from 202.19 ± 32.11 mg/dl to 265.19 ± 32.18 (by 31.15%), 90.96 ± 15.52 mg/dl to 263.22 ± 16.29 mg/dl (189.38% ); 165.47 ± 13.52 mg/dl to 265.89 ± 9.52 mg/dL (by 60.68%) and 18.19± 3.11 mg/dL to 52.644 ± 2.53 mg/dL (by 189.41%) with respect to control subjects respectively whereas the level of serum HDL-cholesterol was non-significantly decreased from 54.91 ± 11.52 mg/dl to 51.94 ± 14.35mg/ dL by 5.40% w. r. t. in healthy control subjects.
Total proteins, albumin and globulin: The summary of serum total protein, Albumin and Globulin depicted in Figure 4. A non-significantly increase in the proteins albumin and globulin was recorded in hypertensive patients from 2.17± 0.36 g/dL to 6.94 ± 1.11w.r.t healthy control subjects.
Figure 4: Status of fasting glucose, HbA1C, total proteins, albumin and globulin levels in healthy control subjects and lipitensive patients.
Values in figure are expressed as mean ± standard deviation and the levels of glucose are expressed in mg/dL, HbA1C are expressed in percent (%) and total proteins, Albumin and globulin levels are expressed in g/dL. Note:  Healthy control subjects,
Healthy control subjects,  Lipitensive patients.
Lipitensive patients.
Ischemia modified albumin: IMA was significantly increased by 129.19 % (from 121.15 ± 19.36 μM/L to 277.67 ± 21.98 μM/L) in lipitensive patients in comparison to healthy normal subjects (Figure 5).
Discussion
Acute Myocardial Infarction (AMI) is one of the major causes of mortality and morbidity in the world. The most common cause of an AMI is atherosclerotic coronary artery with erosion or rupture of a plaque causing transient, partial or complete arterial occlusion. Heart cannot continue to function without adequate blood flow and if it is severely compromised, death is inevitable. Several risk factors for coronary heart disease have been well recognized, including hyperlipidemia, hypertension etc [9-12].
Dyslipidemia is one of the strong predictors of cardiovascular disease, causes endothelial damage and loss of physiological vasomotor activity. The damage may manifest as elevated systemic Blood Pressure (BP). Cross- sectional studies have suggested a link between abnormal lipids and hypertension. Dyslipidemic patient having serum total cholesterol, TG and LDL-cholesterol and very- LDL-cholesterol level 31.15%, 189.38%, 60.68% and 189.41% higher than the healthy control subjects suffering with hypertension were recruited in the present (Figure 6). Delving into the literature reports that dyslipidemia and hypertension contributes to various cardiovascular diseases like atherosclerosis and the resultant vascular risk, through its effects on the level of the endothelium [13-17].
Patients seek care in the emergency department because of chest pain or other symptoms suggesting an acute coronary syndrome but only 10% are subsequently confirmed to have AMI. The criteria for the diagnosis of myocardial infarction have been redefined recently, as reported in a consensus document of the European Society of Cardiology (ESC) and the American College of Cardiology (ACC) and require at least 2 of the 3 following characteristics: typical symptoms, characteristic rise and fall pattern of a cardiac marker and typical Electrocardiogram (ECG) [17] pattern involving the development of Q waves.
In clinical practice, more attention has been paid to the determination of myocardial markers in the diagnostic of acute myocardial Ischemia, Stratification of acute coronary syndrome risk and differential diagnosis of reversible verses irreversible myocardial ischemia and acute chest pain. Prolonged ischemia can lead to myocardial cell death and is a pre-condition to infarction.
Literature reports revealed that during an acute ischemic event, structural changes occur in the amino terminal of albumin, rapidly reducing its capacity to bind transition metal ions and generate a metabolic variant of the albumin referred as Ischemic Modified Albumin (IMA) [18-20]. IMA has recently been evaluated as new sensitive serum biomarker of cardiac ischemia in contrast to cardiac enzymes, which are released when cardiac necrosis occurs. IMA has already been licensed by the US food and drug administration for diagnosis of suspected myocardial ischemia.
In the present study, IMA level was significantly increased by 129.19% (from 121.15 ± 19.36 μM/L to 277.67 ± 21.98 μM/L) in the lipitensive patients w. r. t healthy control subjects. Our observations of significant increase in IMA levels are in agreement with literature reports [17,21-23] that ischemic events may cause as much/more damage to serum albumin and the surrounding tissue as ischemia itself. Different mechanisms have been postulated for generation of IMA early after cardiac ischemia. Either ischemia or reperfusion may include hypoxia, acidosis, free radical damage, membrane energy-dependent sodium and calcium pump disruptions, and free iron and cupper ion exposure. Most of these conditions occur in vivo within minutes after the onset of acute myocardial ischemia. Therefore, IMA can be used as an alternative biochemical parameter to aid as an early marker for clinical diagnosis.
Conclusion
Aforementioned observations of significant (P ≤ 0.01) enhancement by 129.19% (from 121.15 ± 19.36 μM/L to 277.67 ± 21.98 μM/L) in serum IMA levels in hypertensive patients suffering with dyslipidemia (Study Group) with respect to healthy control subjects (Control Group) suggested that ischemia modified albumin as a sensitive and early biomarker might be useful for optimal treatment of lipitensive patients for their early clinical diagnosis to prevent risk of other cardiovascular diseases like atherosclerosis. Further studies with large sample size are needed to establish the cutoff values of serum ischemia modified albumin levels for stratification of patient.
Acknowledgment
I thank to the faculty of Medicine Department, Government Medical College and Rajindra Hospital, Patiala for providing patients and their cooperation. My thanks to participants for giving me opportunity for being the part of this study. I would like to thank Multi-Disciplinary Research Unit (MRU), Government Medical College and Rajindra Hospital- Patiala for providing equipment’s/ machinery to conduct this research work.
Conflict of Interest
None