ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 13
Expression and its correlation with metabolic syndrome of protein tyrosine phosphatase 1B in serum of polycystic ovary syndrome patients
Xuecheng Shao1, Jia Li1, Yu Wang2, Qian Liang1 and Shurong Song1*
1Department of Obstetrics, Tianjin Third Central Hospital, Tianjin, PR China
2Department of Women Health Care, Mentougou Maternal and Child Health Care Hospital of Beijing, Beijing, PR China
- *Corresponding Author:
- Shurong Song
Department of Obstetrics
Tianjin Third Central Hospital, PR China
Accepted date: May 24, 2017
Objective: To investigate the expression of protein tyrosine phosphatase 1B (PTP1B) in serum of Polycystic Ovary Syndrome (PCOS) patients and its correlation with the Metabolic Syndrome (MS).
Methods: ELISA was used to detect the expression of protein tyrosine phosphatase 1B (PTP1B) in the serum. Samples were divided into three different groups: 21 cases in control group; 48 cases in the group of non-MS-PCOS; 15 cases in the group of MS-PCOS.
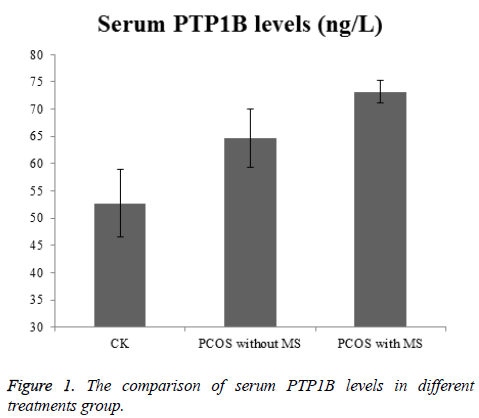
Results: The level of PTP1B in serum of PCOS patients was (66.65 ± 24.30 ng/L) higher than that of control group (52.72 ± 16.20 ng/L),(P<0.05). PTP1B level in serum of MS-PCOS was (73.14 ± 20.07 ng/L) that was higher than that of non-MS-PCOS (64.62 ± 25.33 ng/L, P<0.05). PTP1B was positively correlated with Body Mass Index (BMI), Waist Circumference (WC), Fasting Plasma Glucose (FPG) and homeostatic model assessment insulin resistance (HOMA-IR (P<0.05)).
Conclusion: Elevated serum level of PTP1B is an important factor which caused insulin resistance in PCOS patients. Moreover, PTP1B is related to obese, fasting plasma glucose and insulin resistance of metabolic syndrome, which may play a role in the diagnosis or treatment of PCOS and metabolic syndrome.
Keywords
Polycystic ovary syndrome, Protein tyrosine phosphatase 1B, Metabolic syndrome, Expression
Introduction
Polycystic Ovary Syndrome (PCOS) patients with ovulation or rare ovulation, hyperandrogenism, ovarian polycystic changes as the main performance, accompanied by a serious impact on the quality of life of metabolic abnormalities, such as obesity, insulin resistance, hyperinsulinemia, dyslipidemia and longterm cardiovascular disease. Clinically, PCOS patients can be seen with Metabolic Syndrome (MS) related performance. MS is mainly manifested as obese, accompanied by diabetes or impaired glucose tolerance, blood disorders, high blood pressure. PCOS and MS patients overlap with each other.
Protein tyrosine phosphatase 1B (PTP1B) is associated with most of the risk factors of MS, which is closely related to insulin signal transduction, type 2 diabetes, obesity, and lipid metabolism. PTP1B as a target for the development of PTP1B inhibitors for the treatment of diabetes and metabolic syndrome has opened up new areas and give patients a new dawn. PCOS and MS interact with each other, promote each other, a serious threat to the health of patients and quality of life. This study will discuss the expression of PTP1B in PCOS serum and analysis the relationship with MS, in order to provide new ideas and further evidence for PCOS and MS prevention, diagnosis and treatment.
Materials and Methods
Research objects and grouping
A total of 63 patients with PCOS were selected from January 2010 to March 2011 at the Second Affiliated Hospital of Harbin Medical University. Among them, 15 PCOS patients were selected into a group complicated with metabolic syndrome (MS-PCOS group), aged 21-37 y; 48 cases of PCOS were selected into another group without metabolic syndrome (non-MS-PCOS group), aged 20-37 y. Genital examination and physical examination to exclude congenital adrenal hyperplasia, cushing syndrome, secretion of androgen tumors, hyperprolactinemia, acromegaly, premature ovarian failure and drug-derived (the use of androgen, sodium valproate, cyclosporine or other drugs). The control group (CK) of 21 cases, aged 20-36 y old, for healthy subjects, the normal menstrual cycle, was serum hormone test and uterine attachment B ultrasound examination to exclude polycystic ovarian changes. The selection criteria: waist<80 cm, blood pressure<130/85 mmHg, sugar-free lipid metabolism, no other acute and chronic diseases. Case diagnostic criteria: (1) PCOS diagnosis: in line with the 2003 Rotterdam meeting revised diagnostic criteria [1]. (2) Diagnosis of metabolic syndrome: the inclusion of patients in line with the 2005 International Diabetes Federation to develop a global consensus definition [2].
Specimen collection
Subjects were fasted for 12 h, the next morning to measure blood pressure, height, waist circumference, fasting elbow median venous blood 5 ml, standing for 1 h, on the 3,000 r/min centrifuge, centrifugation 15 min, take sufficient amount of supernatant set to -80°C save.
Experimental method
Fasting Serum Insulin (FIN), Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH) and Testosterone (T) were measured by Bayer's ADVIA CENTAUR Chemiluminescence Analyzer, which was produced by Japan's Dong Cao AIA Co., Ltd. Fasting Blood Glucose (FPG) using glucose kit (oxidase method), by the Shanghai Branch of Biological Engineering Co., Ltd. production. Serum PTP1B was measured by ELISA, and the kit was produced by R&D. ELISA method in strict accordance with the instructions. The linear regression equation of the standard curve is calculated according to the concentration of the standard and the corresponding OD value. The corresponding sample concentration is calculated according to the OD value of the sample on the regression equation.
The calculation of the correlation index
Body mass index (BMI): BMI=body weight/height square (kg/m2)
Steady state model index (HOMA-IR)=fasting insulin (μU/ml) × fasting blood glucose (mmol/L)/22.5
Statistical methods
SPSS l9.0 statistical software was used for analysis. The results were expressed as the mean ± standard deviation (x ± s), and the normality of the test data was normalized without normal distribution. Variance analysis was used for comparison between groups. PTP1B, BMI, HOMA-IR and other related analysis was analyses by Pearson correlation analysis. P<0.05 or P<0.01 means statistically significant.
Results
General situation
As seen from Table 1, there was no significant difference in age between the three groups (P>0.05). Comparison of waist circumference and BMI between the three groups, there was a significant difference between the two groups. MS-PCOS group waist circumference and BMI was significant higher than that of CK group (P<0.05). Moreover, MS-PCOS group waist circumference, BMI was statistical significant higher than non-MS-PCOS group (P<0.05).
| Group | Number | Age | Waistline (cm) | BMI (kg/ m2) |
|---|---|---|---|---|
| CK | 21 | 28 ± 4 | 83.19 ± 6.00 | 24.20 ± 2.04 |
| PCOS without MS | 48 | 26 ± 4 | 85.83 ± 12.80 | 26.18 ± 4.39* |
| PCOS with MS | 15 | 27 ± 4 | 93.37 ± 13.71* | 28.17 ± 5.78* |
| *P<0.05 | ||||
Table 1. The comparison of general cases.
Sex hormones, fasting blood glucose, fasting insulin comparison
We can see form Table 2, there were no significant differences in FSH, LH, T, FPG and FIN between MS-PCOS group and non-MS-PCOS group (P>0.05), how they are statistically significant high than that of CK (P<0.05). There were significant differences in FPG and FIN between MS-PCOS group and non-MS-PCOS group (P<0.05), FPG and FIN in MS-PCOS group was higher than that of non-MS-PCOS group.
| Group | FSH (mIU/ml) | LH (mIU/ml) | T (nmol/L) | FPG (mmol/L) | FIN (µU/ml) |
|---|---|---|---|---|---|
| CK | 2.63 ± 0.95 | 3.28 ± 1.07 | 0.91 ± 0.26 | 5.44 ± 0.53 | 11.08 ± 3.77 |
| PCOS without MS | 4.82 ± 1.59* | 8.07 ± 4.31* | 1.67 ± 0.58* | 5.06 ± 0.50* | 16.99 ± 10.94* |
| PCOS with MS | 5.14 ± 3.23* | 7.69 ± 3.86* | 1.96 ± 0.69* | 6.44 ± 1.21* | 27.73 ± 15.14* |
| *P<0.05 | |||||
Table 2. The comparison of three groups of FSH, LH, T, FPG, FIN levels.
Comparison of serum PTP1B levels
As seen in Figure 1, the PTP1B levels of PCOS patients was higher than the control group, the difference was statistically significant (P<0.05). And interestingly, the level of PTP1B in PCOS group was higher than that in PCOS group without MS group (P<0.05).
PTP1B level and waist circumference, BMI, HOMAIR correlation analysis
The correlation analysis between PTP1B level and waist circumference, BMI, HOMA-IR showed that the correlation coefficients of PTP1B level in serum with waist circumference, BMI and HOMA-IR were 0.481, 0.3080 and 0.814 respectively. There was a positive correlation between PTP1B level and waist circumference, BMI and HOMA-IR (P<0.01), please see Table 3 for details.
| PTP1B | ||
|---|---|---|
| r | P | |
| Waistline | 0.481 | <0.01 |
| BMI | 0.38 | <0.01 |
| HOMA-IR | 0.814 | <0.01 |
| *P<0.05 | ||
Table 3. The correlation between PTP1B and waist circumference, BMI, HOMA-IR.
Discussion
The expression level of PTP1B is associated with insulin resistance. High levels of PTP1B expression in high glucose environment cells can reduce insulin tyrosine phosphorylation by more than 20%, and inhibit insulin-induced gluconeogenesis. The results showed that G-base insertion at the 3-terminal 1484 position of human PTP1B gene could increase the expression of PTP1B, and the genotype of the population was more likely to produce insulin resistance [3].
Polycystic Ovary Syndrome (PCOS) is caused by ovarian dysfunction caused by menstrual disorders or amenorrhea, anovulatory infertility, hyperandrogenism, obesity and other symptoms. Insulin resistance and compensatory hyperinsulinemia is an important pathological basis for abnormal glucose metabolism in PCOS patients and is a major factor in the development and progression of PCOS. Insulin resistance can be closely linked to PCOS at three levels: prereceptor level, receptor level, and post-receptor level, depending on the different stages of insulin-regulated glucose metabolism.
Metabolic Syndrome (MS) is mainly manifested as obesity, accompanied by diabetes or impaired glucose tolerance, with hypertriglyceridemia and high-density lipoprotein cholesterol is characterized by decreased blood quality and hypertension. MS and insulin resistance are closely related, insulin resistance in the occurrence and development of MS play a role. Insulin resistance may be the central part of MS pathogenesis. Due to insulin resistance, adipose tissue triglyceride decomposition strong, so that the liver free fatty acid overload, which further strengthens the formation of hepatic glucose, triglyceride biosynthesis and very low density lipoprotein (cholesterol) Lipopoletal cholesterol, VLDL-C), the increase in VLDL-C in the circulation is a decrease in HDL-C and an increase in small and dense LDL-C particles, and an increase in free fatty acid loading also leads to insulin resistance in the surrounding tissue. There are scholars that insulin resistance and inflammation are closely related. But the specific mechanism is not yet clear.
Insulin resistance and hyperinsulinemia may be a common pathogenesis of PCOS and MS [4]. In the insulin resistance state, hyperinsulinemia by causing fat metabolism and liver fat synthesis caused by lipid disorders, and then lead to MS. Hyperinsulinemia and insulin resistance can also directly affect the glucose metabolism, involved in PCOS and MS occurrence and development. The results of this study, PCOS MS group and PCOS group MS patients with fasting insulin levels than the control group, to a certain extent, also shows that hyperinsulinemia and insulin resistance and PCOS and MS have a certain relationship. Related studies also pointed out that patient with both PCOS and MS, the degree of hyperinsulinemia and insulin resistance is far greater than the simple PCOS patients [5]. The results of this study showed that the level of fasting insulin in PCOS group was higher than that in PCOS group (P<0.05), which was consistent with the conclusion of other scholars. It was further confirmed that PCOS and MS were closely related to insulin resistance, Insulin resistance is a common pathogenesis of both. Previous studies have confirmed the role of PTP1B in insulin resistance, and insulin resistance in PCOS and MS pathophysiology is considered to be the key link. Therefore, we believe that PTP1B in PCOS and MS pathogenesis plays an important role. The expression of PTP1B in PCOS patients was significantly higher than that in the control group. The expression of PTP1B in PCOS group was higher than that in other groups (P<0.05), indicating that PTP1B was significantly higher than that in control group occurred, the occurrence of PCOS and MS, the development does play a role.
The results suggest that PTP1B can be used as a new basis and clinical index for determining insulin resistance in patients with PCOS and MS. It is also possible to detect early insulin resistance by detecting insulin levels in PTP1B reaction in PCOS and MS patients, In order to help us better understand the occurrence of PCOS and MS, the development mechanism and predict the prognosis of PCOS and MS.
PCOS is often associated with central obesity, hyperinsulinemia, insulin resistance, impaired glucose tolerance or (and) type 2 diabetes, dyslipidemia and so on. These metabolic abnormalities are an important part of MS and diagnostic conditions, and in these two syndromes, these metabolic abnormalities have similar characteristics, it is necessary to recognize and actively look for the relationship between this two.
The incidence of MS in PCOS patients was significantly higher than that in the general population. However, the incidence of MS in PCOS patients was not consistent due to the differences in ethnic and dietary patterns in various regions and the diagnostic criteria of MS. Application of the National Cholesterol Education Program Adult Treatment Group III guidelines NECP ATP III diagnostic criteria for the United States PCOS women study found that the United States PCOS women in the incidence of MS was 43% to 46%, significantly higher than the US general population (22.6%) [6-8]. Soares et al. [9] used NECP ATP III diagnostic criteria for PCOS patients in Brazil to study, the results show that Brazil PCOS patients with MS incidence of 28.4%. Carmina et al. [10], respectively, using ATP III and WHO MS diagnostic criteria, found that Italian PCOS patients with MS incidence of 8.9% and 17.3%, significantly lower than the incidence of MSOS patients in the United States, and the Czech Republic PCOS patients MS And the difference between the normal control group was not statistically significant [11]. Weerakiet et al. [12] reported that the incidence of MS in patients with PCOS in Asia was 35.3%.
Of the 63 patients with PCOS collected in this study, 15 patients had PCOS with MS, and MS patients accounted for 23.8% of patients with PCOS, which were lower than those of PCOS patients in Asia [12] The diet and lifestyle are different from those of other Asian countries. Lin et al. [13] on the average age of (25. 6 ± 3.67) years of age in Guangdong, China PCOS patients were studied, the results showed that the incidence of MS was 14.16%, significantly lower than the results of this study, which may be vast with China, Different dietary structure of the north and south and the age of the study. The incidence of MS in patients with PCOS in China, the more accurate data to be a large sample of the population statistics confirmed.
In the study of the relationship between PCOS and MS, elevated androgen levels may also be involved in the pathogenesis of PCOS and MS. There is controversy about the relationship between hyperandrogenism and MS. Some scholars have suggested that hyperandrogenism is a risk factor for MS independent of obesity and insulin resistance [14]. There has been a large number of facts proved [15], hyperandrogenism and hyperinsulinemia on lipid metabolism abnormalities play a vicious cycle. However, there are also studies found that free androgen levels of different PCOS patients, the MS prevalence of no significant difference [16]. The results of this study showed that the experimental group than the control group of male and high, statistically significant (P<0.05), but PCOS MS group and PCOS group MS and androgen compared no significant difference (P>0.05) The Combined with the results of other scholars and the results of this experiment, suggesting that our androgen and MS in the end what kind of relationship need more research to demonstrate. The results of this study also see FSH, LH in the PCOS group than the control group, the difference was statistically significant (P<0.05), which may be PCOS patients with hormonal disease results.
Recent studies have shown that PTP1B has a certain intrinsic relationship with most of the risk factors of MS [17]. PTP1B is associated with obesity, and obesity plays an important role in the development and progression of MS. Obesity is the initiation factor of MS onset. In particular, central obesity is closely related to MS. The new definition of MS revision by International Diabetes Federation (IDF) also highlights the importance of obesity in MS. (BMI) was the central factor in the pathogenesis of MS, and confirmed that obesity was an important factor in the initiation of MS. The experimental data show that PCOS MS group compared with PCOS without MS group and control group BMI, waist circumference increased significantly, consistent with previous studies, also shows that obesity in the pathogenesis of MS important role. The expression of PTP1B is closely related to obesity which was used to measure the amount and activity of PTP1B in adipose tissue of non-diabetic patients (LD), obese non-diabetic patients (OC) and obese diabetic subjects (OD) [18]. The results showed that the level of PTP1B protein in OC group was increased by 3 times compared with LC group, the OD group increased by 5.5 times, and the expression level of PTP1B was positively correlated with BMI (r=0.672, P<0.05). Similarly, the expression level of PTP1B was positively correlated with BMI and waist circumference, and it was confirmed that PTP1B was closely related to obesity. Immunoblotting confirmed that the number of PTP1B decreased with weight loss. This suggests that PTP1B is closely related to obesity and that PTP1B plays an important role in the development of obesity. In this experiment, PTP1B in PCOS MS group compared with PCOS without MS group and control group was statistically significant (P<0.05), which indicated that PTP1B and MS the occurrence and development of close contact, which for the prevention and treatment of MS provide a new way of thinking. This also suggests that in clinical work, can be through the MS patients’ serum PTP1B detection, analysis and judgment of the incidence of MS and MS prognosis assessment to provide new clinical indicators.
Animal activity confirmed that fructose-fed mouse liver cells, PTP1B activity was significantly increased, apolipoprotein B and very low density lipoprotein microparticle synthesis increased [19]. And PTP1B gene knockout mice did not show very low density lipoprotein increased, suggesting that PTP1B has the role of promoting very low density lipoprotein secretion [20]. Analysis of the lipoprotein profile of PTP1B knockout mice showed that the content of apolipoprotein B in plasma decreased and its very low density lipoprotein content was downregulated [21]. Hyperglycemia obese mice treated with PTPlB antibody, the level of PTP1B in fat decreased, the degree of obesity decreased, the level of triglyceride in adipocytes was also affected, which was associated with down regulation of genes associated with adipogenesis [22]. Sterol regulatory element binding protein-1 (SREBP-1) is an important regulator of postprandial triglyceride levels. Shimizu and so on with fructose for 8 w, found that PTP1B and SREBP-1 mRNA expression levels were significantly increased; PTP1B in liver cells overexpression can promote SREBP-1, fatty acid mRNA synthesis. Studies have confirmed that PTP1B membrane localization is necessary for the expression of the SREBP-1 gene [23]. In addition, it has been found that PTP1B is associated with a series of lipid metabolism-related genes such as peroxisome Proliferator- Activated Receptor (PPAR) gamma, fatty acid synthetase and the like. The study also found that liver PTP1B activity can cause hypertriglyceridemia [24].
In addition, people's research on lipid metabolism is also increasingly concerned about the fat factor, and found that fat factor and PCOS relationship is very close. The adipokines are a class of cytokines secreted mainly by adipose tissue, including adiponectin, 1eptin, visfatin, resistin, tumor necrosis factor, TNF-α. Researchers have suggested that the reduction in serum adiponectin may be a central factor in the pathogenesis of insulin resistance in PCOS patients [25]. It has also been suggested that adiponectin is an independent risk factor for the pathogenesis of MS and is likely to play an important role in the pathogenesis of PCOS [26]. Zhang successfully cloned rat obesity gene and human homologous sequence using site cloning technique, and elucidated the protein product of obese gene-leptin [27,28]. Studies have shown that high insulin and insulin resistance in patients with PCOS may be the cause of elevated serum leptin levels, suggesting that there is not only insulin resistance in PCOS patients, but there may be leptin resistance [29]. Madhavi et al. confirmed that serum leptin levels in PCOS patients significantly increased, leptin and BMI also related to [30]. Vifatin This protein is highly expressed in human and mouse visceral fats. The levels of visfatin in patients with PCOS were higher than those in normal controls, and the levels of visfatin in PCOS group were positively correlated with BMI [31]. Studies of Kowalska et al. [32] showed a negative correlation between serum visfatin and insulin sensitivity in PCOS patients.
The above data show that the relationship between fat factor and PCOS is very close, and this also strongly confirmed the lipid metabolism in PCOS MS important role. Therefore, we study the relationship between PTP1B and PC in PCOS, and can fully understand the pathogenesis and related factors of dyslipidemia in PCOS, and further open up a new way for the prevention and treatment of PCOS and MS.
In summary, PCOS patients with elevated serum PTP1B levels, is caused by PCOS patients with insulin resistance is an important factor. At the same time serum PTP1B and MS certain factors such as obesity, fasting blood glucose, insulin resistance was positively correlated with serum PTP1B levels and the occurrence and development of MS. It is possible to better understand the intrinsic relationship between PCOS and MS and to predict the occurrence, development and prognosis of PTP1B by detecting the expression of PTP1B in serum, and to explore the relationship between the expression of PTP1B in the pathogenesis of PCOS and MS. Treatment of PCOS and MS provides new convenient and economical means of assisting.
References
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod 2004; 19: 41-47.
- Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome--a new worldwide definition. Lancet 2005; 366: 1059-1062.
- Di Paola R, Frittitta L, Miscio G. A variation in 3 UTR of PTP1B increases specific gene expression and associates with insulin resistance. Am Hum Genet 2002; 70:806-812.
- Carmina E. Metabolic syndrome in polycystic ovary syndrome. Minerva Ginecol 2006; 58: 109-114.
- Magnotti M, Futterweit W. Obesity and the polycystic ovary syndrome. Med Clin North Am 2007; 91: 1151-1168.
- Glueck CJ, Papanna R,Wang P. Incidence and treatment of metabolic syndrome in newly referred women with confirmed polycystic ovarian syndrome. Metabolism 2003; 52: 908-915.
- Apridonidze T, Essah PA, Iuorno MJ, Nestler JE. Prevalence and characteristics of the metabolic syndrome in women with polycystic ovary syndrome. J Clin Endocrinol Metab 2005; 90: 1929-1935.
- Essah PA, Nestler JE. Metabolic syndrome in women with polycystic ovary syndrome. Fertil Steril 2006; 86: 18-19.
- Soares EMM, Azevedo GD, Gadelha RGN. Prevalence of the metabolic syndrome and its components in Brazilian womenwith polycystic ovary syndrome. Fertil Steril 2008; 89: 649-655.
- Carmina E, Napoli N, Longo RA. Metabolic syndrome in polycystic ovary syndrome (PCOS): Lower p revalence in southern Italy than in the USA and influence of criteria for the diagnosis of PCOS. Euro J Endocrinol 2006; 154: 141-145.
- Vrbíkova J, Vondra K, Cibula D, Dvorakova K, Stanicka S. Metabolic syndrome in young Czech women with polycystic ovary syndrome. Hum Reprod 2005; 20: 3328-3332.
- Weerakiet S, Bunnag P, Phakdeekitcharoen B. Prevalence of the metabolic syndrome in Asia women with polycystic ovary syndrome: Using the International Diabetes Federation criteria. Gynecol Endocrinol 2007; 23: 153-160.
- Apridonidze T, Essah Paiuorno MJ, Nestler JE. Prevalence and characteristics of the metabolic syndrome in women with polycystic ovary syndrome. J Clin Endocrinol Metabol 2005; 90: 1929-1935.
- Diamanti-Kandarakis E,Christakou C,Kandarakis H. Polycystic ovary syndrome :the commonest cause of hyperandrogenemia in women as a risk factor for metabolic syndrome. Minerva Endocrinol 2007; 32: 35-47.
- Bi-Bo LU, Zhou YW, Xie XZ. Research progress of the main reproductive hormone receptors in poultry testis. J Domestic Animal Ecol 2016.
- Weerakiet S, Bunnag P, Phakdeekitcharoen B. Prevalance of the metabolic syndrome in Asian women with polycystic ovary syndrome: using the International Diabetes Federation criteria. Gynecol Endocinol 2007; 23: 153-160.
- Maison P, Day NE, Byme CD. Do different dimensions of the metabolic syndrome change together over time? evidence supporting obesity as the central feature. Diabetes Care 2001; 24: 1758-1763.
- Cheung A, Kusari J, Jansen D. Marked impairment of protein tyrosine phosphatase 1B activity in adipose tissue of obese subjects with and without type 2 diabetes mellitus. J Lab Clin Med 1999; 134: 115-123.
- Taghibiglou C, Rashid-kolvear F, Van Idersfine SC. Hepatic very low density lipoprotein-ApoB overproduction is associated with attenuated hepatic insulin signaling and overexpression of proteintyrosine phosphatase lB in a fructose-fed hamster model of insulin resistance. Biol Chem 2002; 277: 793-803.
- Klaman LD, Boss O, Peroni OD. Increased energy expenditure, decreased adiposity,and tissue-specific insulin sensitivity in proteintyrosine phosphatase 1B-deficient mice. Mol cell Bid 2000; 20: 5479-5489.
- Qiu w, Avram RK, Dube N. Hepatic PIP1B expression regulates the assembly and secretion of apolipoprotein B-containing lipoproreins:evidece from proteintyrosine phosphatase 1B overexpression knockout and RNAi studies. Diabetes 2004; 53: 3057-3066.
- Rondinone CM, Trevillyan JM, Clampit J, Gum RJ, Berg C. Protein tyrosine phosphatase 1B reduction regulates adiposity and expression of genes involved in lipogenesis. Diabetes 2002; 51: 2405-2411.
- Kun S, Ugi S, Shimizu S. Membrane location of protein-tyrosine phosphatase 1B is essential for its activation of sterol regulatory element-bindingprotein-1 gene expressen. Biol Chem 2007; 363: 626-632.
- Satoshi U, Kun Shi, Shimizu S. Membrane localization of protein-tyrosine phosphatase 1b is essential for its activation of sterol regulatory element-binding protein-1 gene expression and consequent hypertriglyceridaemia. Biol Chem 2009; 146: 541-547.
- Louise MH, Henrik L, Joel K. Adipose tissue has aberrant morphology and function in PCOS: enlarged adipocytes and low serum adiponectin, but not circulating sex steroids, are strongly associated with insulin resistance. J Clin Endocrinol Metab 2011; 96: 304-311.
- Leustean L, Fica S, Preda C. Adiponectin and metabolic syndrome in PCOS patients- beyond obesity. Endocrine Abstracts 2011; 26: 117.
- Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med 1995; 1: 1155-1161.
- Zhang Y, Hufnagel C, Eiden S. Mechanisms for LEPR-mediated regulmion of leptin expression in brown and white adipocytes in rat pups. Physiol Genomics 2001; 19: 189-199.
- Kim JB, Sarraf P, Wright M, Yao KM, Mueller E. Nutritional and insulin regulation of fatty acid synthetase and leptin gene expression through ADD1/SREBP1. J Clin Invest 1998; 101: 1-9.
- Madhavi P, Pervin M, Jyotsna G. Obesity and polycystic ovary syndrome: association with androgens, leptin and its genotypes. Gynecol Endocrinol 2010; 26: 874-882.
- Chan TF, Chen YL, Chen HH. Increased plasma visfatin concentrations in women with polycystic ovary syndrome. Fertil Stefil 2007; 88: 401-405.
- Kowalska L, Straczkowski M. Serum visfatin in relation to insulin resistance and markers of hyperandrogenism in lean and obese women with polycystic ovary syndrome. Human Reprod 2007; 22: 1824-1829.