ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2015) Volume 26, Issue 3
Gender differences in body composition, respiratory functions, life style among medical students.
Magda HM Youssef1; Moaz Mojaddidi1; Mohamad Fath El Bab2; Wafaa Abd El Nabi3 and Mohamad Salem1
1Department of Physiology, Faculty of Medicine, Taibah University, Al Madinah Al Monawarah, KSA
2Department of Physiology, Faculty of Medicine, Suez Canal University, Cairo, Egypt
3Department of Physiology, Faculty of Medicine, Alexandria University, Cairo, Egypt
- Corresponding Author:
- Magda HM Youssef
Department of Physiology
Faculty of Medicine, Taibah University
Al Madinah Al Monawarah
Saudi Arabia
Accepted date: May 08 2015
Obesity in combination with unhealthy life style may increase the risk of chronic diseases. Objectives: This study aimed to determine the gender difference of body composition and respiratory functions among medical students and its relationship with their life style. This study was performed on 165 male and female students. Body mass index (BMI) and body composition parameters were assessed using bioelectric impedance. Respiratory function, fasting blood glucose, lipid profile and sex hormones were assessed. A questionnaire was distributed among the participants to determine the association between the different variables and risk of obesity. The rate of overweight and obesity among male and female students were 16.9% and 15%. Overweight and obesity among male and female students were (24.6% and 21.3% vs. 12.1% and 11.1 %, respectively). Total fat mass and total fat percentage were higher in female students, whereas, free fat mass was higher in male students. The total fat percentage exceeded its normal limits in overweight and obese females and in 11.7% of those with normal BMI. High levels of total fat% were observed in obese and in 66.7% of the overweight male students. Thus, 37.7% in male and 35.6% in female students were obese according to the body fat percentage when used for defining adiposity rather than BMI. Forced vital capacity (FVC) was increased in male students and a positive correlation between FVC and free fat mass among male students was found. These data demonstrate that overweight and obesity are a problem among medical students of Taibah University.
Keywords
Overweight, Obesity, Body mass index, Total fat percentage, Free fat mass.
Introduction
The prevalence of obesity is increasing worldwide and it has become a significant health hazard. Obesity is associated with a large number of debilitating and life threatening disorders, such as cardiovascular, metabolic and other non-communicable diseases [1].
Materials and methods
Studies on medical students in many countries suggested that obesity is a problem among these population groups. Children and adolescents who are overweight and obese, however, face a greater risk of health problems— including type 2 diabetes mellitus, high blood pressure, high blood lipids, asthma, sleep apnoea, orthopaedic problems and psychosocial problems—than their normal weight peers [2].
A variety of factors, including diet, genetic predisposition, physical activities, physiological and behavioral factors, are implicated as contributing factors to obesity. Urbanization, less physical activity, increased energy intake, and the modern life style are important risk factors in obesity [3].
The present study aimed to determine the gender difference of body composition and respiratory functions in Taibah University and its relationship with their dietary intake and physical activities. Medical students represent the most crucial opportunity for education in the field of healthy lifestyles and nutritional habits.
Participants and methods
A cross-sectional study was conducted over in January to April, 2014 academic year at the Faculty of Medicine, Taibah University, AL Madinah Al Monawarah, Saudi Arabia. The participants in this study were 165 healthy male and female students from the first and second academic years (37% males and 63% females). The participation was voluntary and a written informed consent was obtained from each subject, and the study protocol was in agreement with all Saudi Arabia University ethical standards.
A standard questionnaire was developed and distributed to the students after extensive literature review. A group discussion was conducted with other staff members to brainstorm and come up with a suitable data collection tool. The questionnaire was designed containing questions enquiring about age, gender, academic level, total sleeping duration per 24 h, frequency of exercise per week, type of exercise, eating habits, smoking and family history of diabetes and obesity.
Height was measured to the nearest 0.1 cm using a standard stadiometer. Body composition was measured by body composition analyzer type BC-418 MA TANITA (Japan). The participants were asked not to eat or drink within 4 hours prior to being tested. Participants were asked to void within 30 minutes prior to the test (with empty bladder) and students were asked to wipe off the sole of their feet before stepping onto the measuring platform as unclean foot pads interfere with the device conductivity. The participant standing on a metal footpad scale and gripping handles. After recording the participant’s sex, age and height; body mass index, total body water, basal metabolic rate, fat mass, fat free mass, truncal fat mass and truncal fat percentage were calculated and a report was instantly printed.
Forced vital capacity (FVC), forced expiratory volume (FEV) and forced expiratory volume (FEV1) were measured for the participant in a sitting position using spirometer. Fasting blood sample was obtained from only 45 students (22 male and 23 female) due to refusal of some participants to take blood samples. Fasting blood sugar (FBS), was carried out by an enzymatic colorimetric technique, according to Trinder method [4], Triglycerides were determined by an enzymatic colorimetric method according to Bucolo and David, [5] and total cholesterol and HDL-cholesterol were estimated by an enzymatic colorimetric method according to Allain et al. [6] and Friedewald et al. [7]. LDL-cholesterol was calculated according to Friedewald et al. [7] as follows: LDL-C= Total cholesterol–(triglyceride/5+HDL-C). Testosterone and estrogen levels were estimated by ELISA tests according to Kicklighter and Norman [8] and Peckham and McElwain [9] .
Body mass index was used for assessment of overweight and obesity. Calculation of BMI (kg/m2 ) = Body weight in kilogram ( kg) / Height in squared meter (m2) and classified according to the National Institutes of Health (NIH), adults were classified based on their BMI to underweight (BMI < 18.5), normal (BMI = 18.5- 24.9), overweight (BMI = 25-29.9), or obese (BMI ≥ 30). Furthermore, obesity was subdivided to three grades: Grade 1 (BMI = 30-34.9), Grade 2 (BMI = 35-39.9) and Grade 3 or extreme obesity (BMI ≥ 40) (10). Taking in consideration age and gender, the participants were classified as high (BF% ≥ 25) body fat for male, whereas, high (BF% ≥ 35) body fat for female (11).
Statistical analysis
Data were analyzed by the SPSS version 17.0 (SPSS, Inc. Chicago, IL). Frequency table was used to present the distribution of nominal variables. Results were expressed as means ± standard error of means. Qualitative variables were expressed as number and percentage. Parametric variables were analyzed using students't-test, while the analyzed non-parametric variables were tested using Chisquared tests. Correlation coefficients and lines of regression calculated by linear regression analysis (ranking data directly or indirectly) using the least square method. P values below 0.05 were considered as statistically significant. Independent Student's "t" test was used.
Results
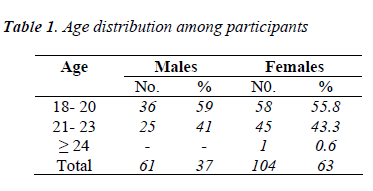
There were 165 responses from the total population of 200 students with a response rate of 82.5%. Study population was distributed as follows: male students totaled 61 (37%) and female 104 (63%). The mean age was 20.5±0.1 years, ranging from 18 to 24 years as seen in table 1. The students were distributed almost equally in the two academic years.
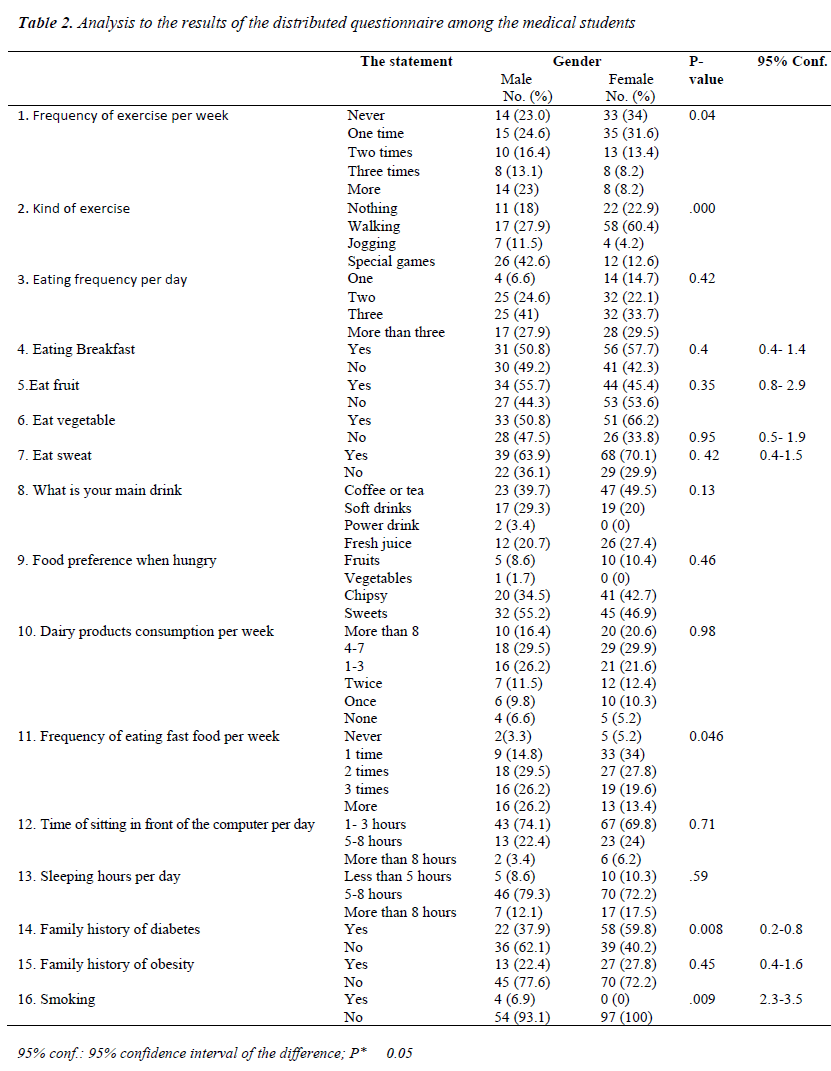
The results represented in Table 2 showed that: There were significant differences in the Frequency of exercise per week and kind of exercise among male and female students. 23.0% vs 34% of male and female students don't do exercise. 24.6% vs 31.6%; 16.4% vs 13.4%; 13.1% vs 8.2% and 23% vs 8.2% of male vs female students do exercise one time; two times; three times or more per week respectively. 42.6% of male students undergo special games whereas, 60.4% of female students prefer walking.
Eating habits showed that 49.2% of males and 42.3% of females don't eat breakfast. 44.3% and 53.6% of male and female students don't eat fruits, 47.5% and 33.8% don't eat vegetables, whereas, 63.9% of males and 70.1% of females eat sweets every day. Coffee or tea was the preferred drink in 39.7% of male students and 49.5% of male students then soft drink then fresh juice. In case of hunger, snacking between meals weresweets, potato chips, fruits and vegetables (55.2%; 34.5%; 8.6% and 1.7% respectively) among male students, and (46.9% and 42.7% ; 10.4% and 0% respectively) among female students.
The frequency of eating fast food per week was significantly higher in male students than female students (P= 0.046). 14.8% of male students and 34% of female students eat one time per week. Eating two times per week was 29.5% vs 27.8% among male vs female students respectively. Eating three times per week was 26.2% vs 19.6%, whereas eating fast food more than three times per week was 26.2% vs 13.4% among male and female students respectively.
Dairy products consumption per week was nonsignificantly changed among male and female students (more than eight times 16.4% vs 20.6%; four to seven times 29.5% vs 29.9%; one to three times 26.2% vs 21.6%; twice 11.5% vs 12.4% and once 9.8% vs 10.3% respectively), whereas, 6.6% of male students and 5.2% of female students don't drink milk.
The time of sitting in front of the computer did not significantly changed among male and female students (from 1-3 hours, 74.1% vs 69.8%, from 5- 8 hours, 22.4% vs 24% ; more than 8 hours, 3.4% vs 6.2% respectively).
The average sleeping hours was non- significantly changed among male and female students, less than 5 hours, 8.6% vs 10.3%, from 5- 8 hours, 79.3% vs 72.2% and more than 8 hours, 12.1% vs 17.5% among male vs female students respectively).
Family history of Diabetes was significantly higher in female compared to male students as 37.9% vs 59.8% had family history of diabetes in male and female students respectively.
Family history of obesity was insignificantly changed as 22.4% vs 27.8% had family history among male and female students respectively. 6.9% of male students smoked.
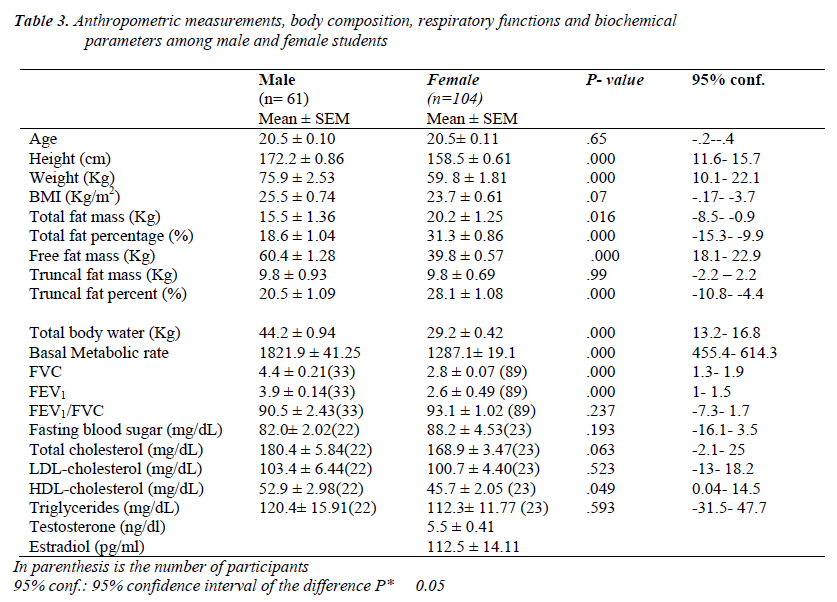
Table 3 showed that the height and weight were more in male than in female students. BMI of male students was 25.5 Kg/m2 and 23.7 Kg/m2 in female students. Total fat mass and total fat percentages were significantly higher in female than in male students. Free fat mass of males were higher than those of females. FVC and FEV1 were significantly higher in male students than female students. The high-density lipoprotein-cholesterol levels were higher in males than in females. There were no statistically differences for total cholesterol, low-density lipoprotein-cholesterol, fasting blood glucose levels between male and female medical students.
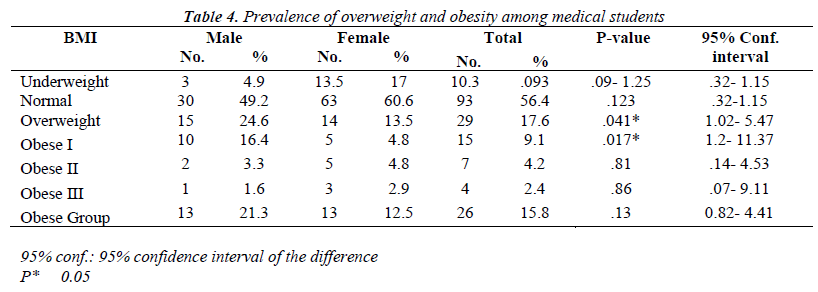
Table 4 showed that depending on BMI, 4.9% of male students and 13.5% of female students were underweight, 49.2% and 61.6% of male and female students were of normal weight, 24.6% of male students and 13.5% of female students were overweight, 21.3% of male students and 12.5% of female students were obese; obese degree I (16.4% vs 4.8%), obese II (3.3% vs 4.8%) and obese III (1.6 vs 2.9%) among male and female students respectively.
Depending on fat percentage classification, 66.7% of underweight male students have low fat percentage while 33.3% had normal fat percentage. 100% of normal BMI had normal fat percentage, 13.9% of overweight had normal fat% while 66.7% have high fat % and 100% of obese have high fat %. 71.4% of underweight female students had low fat% while 28.6% of them had normal fat%. 4.8% of normal BMI have low fat%, 79.3% had normal fat% while 15.9% had high fat%. All overweight and obese females had high fat%. The total males and females with high fat% was 37.7% and 35.6% respectively.
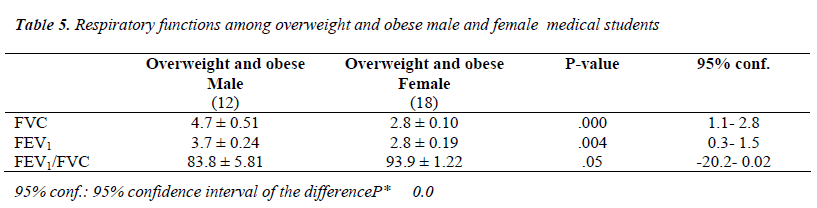
Table 5 showed that FVC, FEV1 and FEV1/FVC were significantly higher in overweight and obese male and overweight than overweight and obese female students.
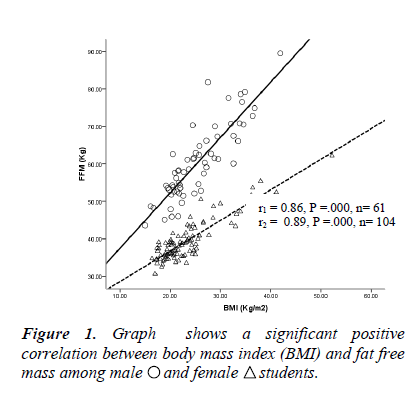
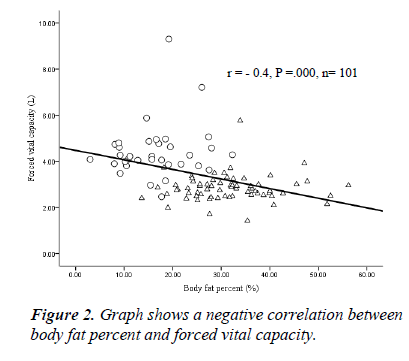
Correlations studies: Figure 1 showed a significant positive correlation between BMI and fat free mass in male and female medical students. Figure 2 shows a significant negative correlation between body fat percent and forced vital capacity among medical students.
Discussion
This study showed that the prevalence rates of overweight and obesity among the sample of students were 17.6% vs 15.8%, which were more common among male students compared to females (24.6% and 21.3% vs. 13.5% and 12.5 %, respectively). 49.2% of males and 60.6% of females were found to be of normal weight, whereas 4.9% of male and 13.5% of female students were underweight.
The study of body composition showed that fat mass, fat percentage and truncal fat percentage were higher in female than male students, whereas, free fat mass was significantly higher in male students than in female students. The total fat percentage exceeded its normal limits in overweight and obese female students and in 15.9% of those with normal BMI. However, high levels of total fat percentage were observed in all obese and in 66.7% of the overweight male students only; those with normal BMI had normal fat levels. When the body composition was used for defining adiposity rather than BMI, This resulted in increasing the obesity prevalence to be 37.7% of male and 35.6% of female students. Also, this showed that normal weight female students could have high levels of fat percentage, which means they might be considered healthy by BMI standards, but in fact they might be at a risk of developing health hazards. So, these results showed that it is necessary to classify obesity condition on the basis of body fat composition, rather than simply on the increase the BMI.
The presence of positive and significant correlations among the anthropometric measurements (BMI, free fat mass, total fat %) were found in this study. These significant positive correlations between BMI and both the fat percentage and the fat free mass indicate that BMI may be caused by gains in either fat weight or lean body mass. This indicates that BMI can’t distinguish between fat and muscle. The usage of BMI doesn't directly measure the amount of adipose tissue and cannot differentiate between fat and lean mass [12; 13].
This finding is consistent with the results of another study of Abdel-Megeid et al., 14 at King Saud University, Riyadh, Kingdom of Saudi Arabia, who found that overweight (23%) and obese (7%) male students were more than overweight (19%) and obese (6%) female students when compared. These results also are in agreement with several studies of [15 -17] who reported that obesity was more common among male students than females. Al-Rethaiaa et al. [18] found that 21.8% of the male students in Qassim University in Saudi Arabia were overweight and 15.7% were obese.
The frequency of eating fast food per week was higher among male than female students. 49.2% of the male students and 42.3% of the female students skipped breakfast. Student’s data showed that 44.3% and 47.5% of the male students do not eat fruits and vegetables respectively. It also showed that 53.6% and 33.8% of female students do not eat fruits and vegetables respectively too. On the other hand, 63.9% of males and 70.1% of females eat sweets every day. When students were hungry most of male and female students eat sweets. The preferred beverage for both student genders was coffee or tea at a percentage of 46.5% among male students and 44% among females, followed by soft drinks.
The result of this study showed that the medical student diet includes high percentages of fat and small amounts of fruits and vegetables. This result is in agreement with the studies of [15, 19-23]. Abdel-Megeid et al. [14]; Ma et al. [24]; Forslund et al. [25] observed that sweets and fatty food increase the energy intake.
The frequency of exercise was significantly higher and more common in male students than females. Also, the type of exercises were different as male students prefer resistance and weight lifting games whereas, female students prefer walking or jogging.
The study of the respiratory function showed that FVC and FEV1 were significantly higher in male students than females. This result could be contributed to the high free fat mass in male students and this is supported by the significant positive correlation between FVC and free fat mass among male students, and the negative correlation between body fat percent and FVC among medical students. All respiratory functions (FVC, FEV1 and FEV1/FVC) decreased in overweight and obese females compared to overweight and obese males. This result is in agreement with Banerjee et al. [26] who reported a decrease in respiratory function at increasing BMI in females than in males.
The findings of this study were limited by the use of a sample of students from just one faculty which may not be a representative of all students in Taibah University. Further studies with a greater number of students at different colleges are required. However, baseline information about BMI, body composition, eating habits and respiratory function among a sample of university students was obtained from the present study.
According to results obtained, the authors concluded that overweight and obesity are problems among Taibah University medical students. Overweight and obesity were more common among male students compared to females. The consumption of fruits and vegetables which are important to prevent chronic diseases was relatively low. Also, an ideal alternative is to use actual measures of body composition rather than of body mass. Increased BMI resulted in decreased respiratory functions in females than in males. These results indicated that medical students need nutritional and health promotion programs to improve their eating habits. It is also important to increase the awareness of eating fruits and vegetables to sustain a good health and to reduce the tendency of overweight and obesity, particularly among males.
Conflict of Interests
The authors declare no conflict of interest in this study.
Acknowledgement
This study (433/1242) was funded by Scientific Research Deanship, Taibah University, Al Madinah Al Monawarrah, Saudi Arabia.
References
- Campbell P, Katzmarzyk P, Malina R, Rao D, PerusseL, Bouchard C. Stability of adiposity phenotypes from childhood and adolescence into young adulthood with contribution of parental measures. Obes Res 2001; 9: 394-400.
- Goossens L, Braet C, Decaluwe V. Loss of control over eating in obese youngsters. Behavior Research and Therapy. 2007; 45(1): 1-9.
- Hingorjo MR, Syed S, Qureshi MA. Overweight and obesity in students of a Dental College of Karachi: lifestyle influence and measurement by an appropriate anthropometric index.J Pak Med Assoc 2009; 59: 528- 532.
- Trinder P. "Determination of blood glucose using an oxidase- peroxidase system with a non-carcinogenic chromogen," J. Clin. Pathol 1969; 22: 158-161.
- Bucolo, G, David, H. Quantitative determination of serum triglycerides by the use of enzymes. Clinical Chemistry 1973; 19(5): 476-482.
- Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol.Clinical Chemistry 1974; 20(4): 470-475.
- Friedewald, WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry 1972; 18(6): 499- 502.
- Kicklighter EJ, Norman RJ.J ClinChem 1989; 43; 658- 660.
- Peckham MJ, McElwain TJ. J ClinEndocinol.Metab1975; 4: 665- 692.
- Chang C J, Wu C H, Chang C S, Yao WJ, Yang YC, Wu JS, et al. Low body mass index but high percent body fat in Taiwanese subjects: implications of obesity cutoffs. Int J ObesRelatMetabDisord 2003; 27, 253- 259.
- Ko GT, Tang J, Chan JC, Sung R, Wu MM, Wai HP, Chen R. Lower BMI cut-off value to define obesity in
- Hong Kong Chinese: an analysis based on body fat assessment by bioelectrical impedance. Br J Nutr 2001; 85, 239-242.
- Muller MJ, LagerpuschM, Enderle J, Schautz B, HellerM, Bosy-Westphal A. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev 2012; 13 Suppl 26-30.
- Frankenfield DC, Rowe WA, Cooney RN, Smith JS, Becker D. Limits of Body Mass Index to Detect Obesity and Predict Body Composition. Nutrition 2001; 17: 26-30.
- Abdel-Megeid FY, Abdelkarem HM, El-Fetouh AM. Unhealthy nutritional habits in university students are a risk factor for cardiovascular diseases. Saudi Med J 2011; 32 (6): 621-627.
- Yahia N, Achkar A, Abdallah A, Rizk S. Eating habits and obesity among Lebanese university students. Nutrition Journal 2008, 7: 32.
- Irazusta A, Hoyos I, Irazusta J, Ruiz F, Diaz E, Gil J. Increased cardio vascular risk associated with poor nutritional habits in first year university students. NutrRes 2007; 27: 387-394.
- Allam AR, Taha IM, Al-Nozha OM, Sultan IE. Nutritional and health status of medical students at a university in Northwestern Saudi Arabia Saudi Med J 2012; 33 (12): 1296-1303.
- Al-Rethaiaa AS, Fahmy AA, Al-Shwaiyat NM. Obesity and eating habits among college students in Saudi
- Arabia: a cross sectional study. Nutrition J 2010; 9: 39-48.
- Galore SR, Walker C, Chandler A. Brief Communication: Dietary habits of first-year medical students as determined by computer software analysis of three-day food records. J Am CollNutr 1973; 12: 517-520.
- Ravussin E, Tataranni PA. Dietary fat and human obesity. J Am Diet Assoc. 1997; 97: S42-46.
- Hill JO, Peters JC. Environmental contributions to the obesity epidemic.Science 1998; 280: 1371-1374.
- Sakarata K, Matumura Y, Yoshimura N, Tamak J, Hashimoto T, Oguri S. et al. Relationship between skipping breakfast and cardio-vascular disease risk factors in the national survey data. Nippon KashuEiseiZasshi 2001; 48: 873-881.
- Ortega RM, Redondo MR, Labez–Sabaler AM, QuintasME, Zamora MJ, Andres P, et al. Association between
- obesity, breakfast time food habits intake of energy and nutrients in a group of elderly. Madrid Residents. J Am Cell Nutr 1996; 19: 65-72.
- Ma Y, Bertone ER,Stanek EJ, Reed GW, Hebert JR, Cohen NL, et al. Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol 2003; 158: 85-92.
- Forslund BH, Torgerson JS, Sjostrom L, Lindroos AK. Snacking frequency inrelation to energy intake and food choices in obese men and women compared toareference population. Int J Obes 2005; 29: 711-719.
- Banerjee J, Roy A, Singhamahapatra A, Dey PK, Ghosal A, Das A. Association of body mass index\ (BMI) with Lung Function Parameters in Non- Asthmatics identified by spirometer protocols. Journal of Clinical and Diagnostic Research 2014; 8(2):12-14.