ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2010) Volume 21, Issue 3
Growth faltering among exclusively breastfed infants in Ogun State, Nigeria
1Department of Nursing Science ,Lead City University, Ibadan, Nigeria
2Department of Health Promotion and Education, Faculty of Public Health, College of Medicine, University of Ibadan, Nigeria.
3Obafemi Awolowo University Teaching Hospital, Ile Ife, Nigeria.1Department of Nursing Science, Lead City University Ibadan, Nigeria
- Corresponding Author:
- A.M. Amosu
Department of Nursing Science
Lead City University
Ibadan, Oyo State, Nigeria
Accepted date: March 11 2010
This is a descriptive and cross-sectional study of the nutritional status of exclusively breastfed infants under six months of age in Ogun state, Nigeria. The objective of this communitybased study was to examine the pattern of growth of infants whose mothers claimed were being exclusively breastfed within the first 6 months of life. Data were obtained from purposely selected 400 nursing mothers with the use of focus group discussions (FGDs) and observational methods, using a combination of exclusive breastfeeding indicators developed from the “Ten Steps to Successful Breastfeeding” guidelines and tips from “Helping Mothers to Breastfeed” guide. Findings revealed that majority of nursing mothers were not exposed to the basic practical steps in breastfeeding during the antenatal period. It was also observed that nursing mothers usually transferred the baby from one breast to another arbitrarily without allowing the baby to exhaust the milk in each breast, thereby depriving the baby of the hind milk necessary for energy. This resulted in a technical deficiency in the practice of exclusive breastfeeding. These findings suggest that health care providers and nursing mothers need to know more about nutrition education on exclusive breastfeeding
Keywords
Exclusive breastfeeding, growth faltering, hind milk, nutrition education
Introduction
The beneficial effects of breastfeeding in the prevention of morbidity and mortality from diarrhoea in infants have been documented [1]. Though nationwide efforts to promote exclusive breastfeeding started in Nigeria since 1992, data on this type of infant feeding are however, generally scarce [2]. Due to many health benefits of breastfeeding to mothers and children, governments of many nations have set goals for breastfeeding practices and rates [3]. However, success in the achievement of such set goals in many countries is still very much in doubt.
Presently in Nigeria, it has been shown by the Multiple Indicator Cluster Survey (MICS) data, that only 13.0% of nursing mothers practiced exclusive breastfeeding [4]. The growth pattern of breastfed babies has been shown to be different from that of formula-fed babies, in that breastfed babies show a slower gain, starting around 4 months. Using a bottle-fed infant growth chart to judge the breastfed infant’s growth can therefore, lead to premature discontinuation of breastfeeding or hasty introduction of complementary foods [5].
Activities to promote breastfeeding are now being carried on world-wide, following the WHO and UNICEF recommendations that infants be exclusively breastfed for about 6 months, followed by the introduction of complementary foods while continuing breastfeeding well into the second year [6] . Diarrhoea is one of the problems associated with the use of feeding bottles while growth retardation in babies has been found to coincide with the introduction of milk substitutes [7].
A 1996 study of pregnant women receiving antenatal care in Jos, Nigeria, showed that 75% of the 653 pregnant women had breastfeeding education. This was however, devoid of practical demonstration of breastfeeding techniques. Forty (6%), of these mothers exclusively breastfed at 3 months while early supplementation was common [8]. Poor feeding techniques contribute significantly to problems associated with infant feeding [9]. Poor exclusive breastfeeding rates might have resulted from the absence of practical demonstration/knowledge of breastfeeding during antenatal nutrition education. When infants are subjected to poor breastfeeding practices, they may easily become malnourished with the tendency of contributing to the increasing rate of infant mortality.
Materials and Methods
This cross-sectional and descriptive study was conducted on purposively selected 440 nursing mothers attending immunization clinics of 40 randomly selected primary health care centres, located within 4 local government areas (Yewa North, Yewa South, Ifo and Ado- Odo Ota ) in Ogun State of Nigeria. These nursing mothers were however, those with undernourished infants whose growth curves were already faltering, and who could show the actual age of their infants (by presenting the infants’ immunization cards). Those who could not satisfy these criteria were excluded from the study. It was also ensured (by confirmation from the mothers and health workers), that none of the infants suffered from any serious illness within the preceding two weeks, prior to the discussions and observations. The nursing mothers’ consent was obtained by requesting them to sign or thumb print consent forms after duly explaining to them the goal of the study. At this stage, however, 40 mothers backed out of the study, leaving 400 of them who continued on to the end. They were then divided into 40 groups consisting of 10 mothers per group. Data were collected from the nursing mothers using qualitative methods including fo cus group discussions (FGDs) and observation/ demonstration. These methods were considered relevant because the use of quantitative data collection instrument, especiially the questionnaire would not capture the actual practice of nursing mothers on exclusive breastfeeding. Data were collected using the FGD guide developed based on the study objectives, and a checklist from indicators of appropriate breastfeeding process as presented in “Ten Practical Steps to Successful Breastfeeding” compiled by the Department of Health and Nutrition Services, Kwa- Zulu Natal, South Africa [10] and the tips on “Helping Mothers to Breastfeed”[11]. The mothers’ responses were tape recorded with their consent and transcribed for manual analysis. Assessment of the nutritional status of the infants was conducted using anthropometric measurements including weight and height (length), to validate the recordings on the growth chart cards brought by the mothers.
Results and Discussion
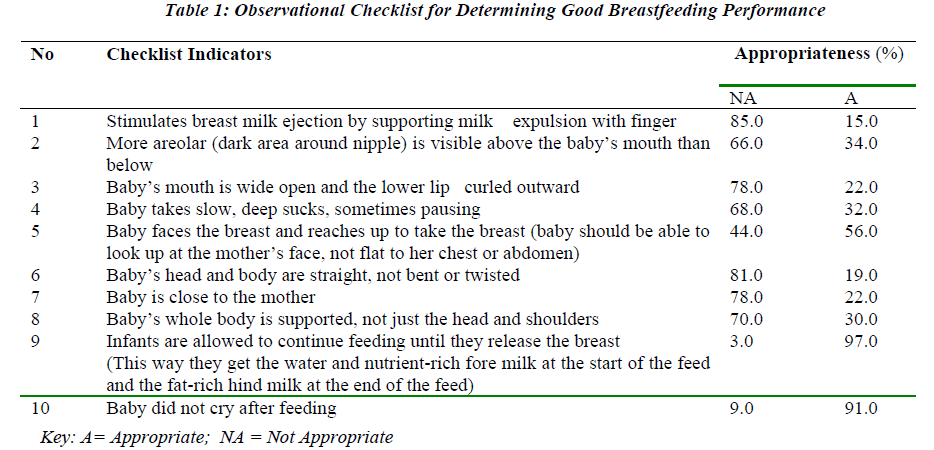
The FGDs’ findings showed that majority of nursing mothers received information on breastfeeding from the nurses, community health workers and community health extension workers. Nearly all the nursing mothers could explain exclusive breastfeeding correctly as the process of feeding babies with breast milk alone without adding even water for the first six months, though many confessed that they didn’t find it easy. It was however, revealed that verbal information was provided to the mothers and in most cases, there was no feedback on the information received. In demonstrating how babies should be breast-fed, nearly all the nursing mothers did not know the appropriate time to transfer the babies from one breast to another during breastfeeding, as this was done arbitrarily during demonstration. The result of the observational checklist (Table 1) showed that the 9th indicator was the main problem the mothers had in the practice of exclusive breastfeeding. This went on to show that they might not be aware of the importance of allowing their infants to suck both the fore and hind milk during breastfeeding. It therefore meant that most nursing mothers fed their infants on fore-milk only (which contains lactose, protein, water, minerals and vitamins), and which may not support adequate growth of the breast-fed infants. Nursing mothers with stunted and undernourished infants did not actually know anything about fore- and hind-milk. The hindmilk comes last during breastfeeding and it contains mainly fat which is required to supply the energy needed by a growing infant. An infant deprived of hind-milk suffers the consequences of insufficient energy intake. This shortfall in energy intake may then lead to other nutrients especially protein, being mobilized to supply the additional energy needed for growth in order to balance the deficit. This may eventually result in the stunting or undernutrition which was observed in the faltering growth charts.
Conclusion and Recommendation
Infants that are exclusively breastfed in the proper way are expected to show normal growth without signs of or record of growth faltering. It was observed in this study however, that the nursing mothers did not receive adequate information on exclusive breastfeeding. They were unaware of the different types of breast milk, and were unable to properly demonstrate how to breastfeed their infants and when to shift from one breast to another during the breastfeeding process, to enable them obtain both the fore- and hind- milk. The results from this study also revealed the possibility of nursing mothers erroneously believing that they practice exclusive breastfeeding whereas scientifically, they do not. This may lead to increase in morbidity and mortality in infants. Also, some of these infants usually resorted to crying when they were not satisfied, a situation which prompted some of the nursing mothers to prematurely introduce complementary food even before the age of six months. It is therefore imperative; to reassess the quality of nutrition education received by nursing mothers from the health care provid ers. Health facilities should be equipped with audiovisuals, and endeavour to provide practical demonstrations of the appropriate ways of carrying out exclusive breastfeeding.
References
- Huffman SL, Combest C1. Role of breast-feeding in the prevention and treatment of diarrhoea. J. Diarrhoeal Dis Res. Sep 1990; 8: 68-81.
- Lawoyin TO, Olawuyi JF, Onadeko MO. Factors Associated With Exclusive Breastfeeding in Ibadan. Nigeria Journal of Human Lactation. 2001; 17: 321-325.
- Vogel A, Hutchison BL, and Mitchell EA . Factors associated with the duration of breastfeeding. Acta Paediatrica 1999; 88: 1320-1326.
- Multiple Indicator Cluster Survey, 2007.
- Guise JM and Freed G . Resident physicians' knowledge of breastfeeding and infant growth, Birth. 2000; 27(1): 49-53.
- Cattaneo A, Davanzo R and Ronfani L . Are data on the prevalence and duration of breastfeeding reliable? The case of Italy, Acta Paediatrica.2000; 89: 88-93.
- Sumati R and Mudambi . Breast-feeding Practices of Mothers from Mid-Western Nigeria Journal of Tropical Pediatrics.1981;27(2):96-100; doi:10.1093/tropej/27.2.96).
- Ighogboja S, Odumodu CU. and Olarewaju RS . Breastfeeding Pattern in Jos, Nigeria, Before Babyfriendly Hospital Initiative. Journal of Tropical Pediatrics 1996; 42(3):178-179; doi:10.1093/tropej/42.3.178).
- Righard L. Are breastfeeding problems related to incorrect breastfeeding technique and the use of pacifiers and bottles? Birth.1998; 25(1): 40-4.
- Savage FK. Helping Mothers to Breastfeed. Revised Edition.1992.