ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 15
Hand dermatitis among nurses at a University Hospital in Saudi Arabia
King Abdulaziz University, Faculty of Medicine in Rabigh, Saudi Arabia
- *Corresponding Author:
- Amal A Kokandi
Department of Medicine, Faculty of Medicine in Rabigh
King Abdulaziz University, Saudi Arabia
Email: akokandi@kau.edu.sa
Accepted date: June 27, 2017
Background: Hand dermatitis is a frequently reported problem among health nurses and other health care professionals worldwide. There is paucity of data regarding this problem in our area.
Objectives: This study aimed to determine the prevalence of hand dermatitis among nursing staff in a University hospital, the factors associated with it and its impact.
Methods: Self-administered questionnaire was distributed to nurses in different departments of a University Hospital in Jeddah.
Results: Out of 181 nurses who completed the questionnaire, 14 (7.73%) nurses reported having symptoms of hand dermatitis. Nurses who reported hand dermatitis were more likely to have past history of eczema, allergic rhinitis and other allergies. Generally there were no considerable effect of hand dermatitis on daily activity, finance and psychological burden.
Conclusions: Hand dermatitis among nurses represents a problem. Despite the fact that the frequency of hand dermatitis was not as high as the frequencies reported in some previous studies, it is still considered an issue that needs addressing and solving. Incidence of hand dermatitis among nurses might need to be confirmed clinically and compared to the general population in our area in future studies.
Keywords
Hand dermatitis, Nurses, Questionnaire.
Introduction
Hand dermatitis comprises a heterogeneous group of disorders with different morphologies and etiologies. Often, the etiological diagnosis of the clinical type of hand dermatitis needs experience and as no simple relationship can be found between them. Patch testing and exposure analysis are mandatory for the diagnosis [1]. Severity of the disease ranges from very mild to severe and the course can be acute or chronic. Hand dermatitis treatment can be challenging and sometimes unsatisfactory [2,3]. A significant proportion of patients may not receive adequate treatment according to the guidelines on management of hand dermatitis [4].
Hand dermatitis is a frequently reported complaint among health care workers worldwide. It is also reported to be the most common diagnosis of occupational skin diseases among health care workers [5]. The prevalence of hand dermatitis varies in different studies worldwide [6]. A review of the literature based on the studies performed between 1964 and 2007 concluded that the point prevalence of hand dermatitis was around 4% in the general population, whereas the lifetime prevalence reaches 15% [7]. Hand dermatitis affects the performance of health care professionals by causing absences and reducing their productivity. Additionally, returning to work after having occupational hand dermatitis can be challenging for nurses [8]. Tobacco smoking, stress and obesity are reported to be associated with hand eczema [9]. The high incidence of hand dermatitis has been attributed to improving hygiene procedures in UK [10].
In our country, there is a huge lack of data on the incidence of hand dermatitis among nurses and other health care professionals. Therefore, this study aimed to determine the prevalence of hand dermatitis among nursing staff and to investigate the factors associated with it.
Methods
A simple 3 page self-administered questionnaire with an invitation letter was distributed to nurses at King Abdulaziz University hospital, Jeddah (Saudi). For convenience; questionnaires were distributed to all departments at the hospital. Completed questionnaires were collected in envelops and collected after 1 w. A second round of collection was commenced after the end of the week after. Questionnaires were collected in the time period of 26 February to 9 March 2017.
The questionnaire contained demographic data of gender, age, place of work, years of experience, any chronic diseases, height and weight (to calculate the BMI), caring for children under 4 y of age, smoking (only yes, no or was a smoker and quitted). It also included questions about history suggestive of eczema (Have you ever had an itchy rash that has been coming and going, and has affected skin creases? (by skin creases we mean folds of elbows, behind the knees, fronts of ankles, under buttocks, around the neck, ears, or eyes?)), history of eczema, asthma, allergic rhinitis and allergies from dust, animals or plants. Additionally, it contained questions about the diagnosed of allergy and where and how the diagnosis was made. Then it was followed by a question about the frequency of hand washing in usual working day and the frequency of using disinfecting alcohol for hands in a usual working day, followed by a question about history suggestive of hand dermatitis (Did you have eczema or inflammation of your skin on your hands, wrists or forearms?) and if the answer is yes, subjects were asked to complete the questionnaire.
The second page contained questions about the frequency of hand eczema in the past 6 months, what is the cause of this in the subject’s opinion, if the subject has ever visited a doctor for this complaint, times of flares and whether hand dermatitis improves with long vacations from work. This was followed by a question about the factors that increase hand or wrist/forearm eczema outside work place, and whether eczema on hands, wrists or forearms affected daily activities by any way in the occupation. Following that, there was a multiple selection question about the influence of eczema on the financial situation and on the psychological well-being?
This study protocol was approved by the unit of biomedical ethics research committee at King Abdulaziz university Hospital (Reference No 400-16).
Statistical analysis
Data was reported as frequency and percentages (%) of hand dermatitis groups and analysed using SPSS (version 21). Statistical significance for the difference in the frequency between subjects with and without hand dermatitis was determined by Pearson chi-square χ2 test. The continuity correction in R was computed for 2 × 2 tables. The effect size for the chi-square test of independence was determined using the phi coefficient. A P<0.05 values (two-sided test) was accepted as statistically significant.
Results
A total of 183 out of 235 questionnaires were received (response rate of 77.9 %). Females were 136 (74.3%) and males were 47 (25.7%). Of these, 2 did not answer the question of having symptoms of hand dermatitis. Out of 181 who answered the question, 14 (7.73%) nurses reported having symptoms of hand dermatitis. Characteristics of the participants in the study are described in Table 1.
| No hand dermatitis (n=167) | Hand dermatitis (n=14) | |
|---|---|---|
| F:M | 122:47:00 | 14:00 |
| Age in years | ||
| Mean ± SE | ||
| Range | 35.68 ± 0.69 | 36.79 ± 2.48 |
| 22-61 | 27-55 | |
| Years of experience | ||
| Mean ± SE | ||
| Range | 8.63 ± 0.5 | 1-38 |
| 10.64 ± 2.28 | 2-25 | |
| BMI | ||
| Mean ± SE | ||
| Range | 26.25 ± 0.4 | 16.71-44.46 |
| 24.2 ± 0.77 | 20.5-28.88 |
Table 1: Characteristics of study groups according to hand dermatitis.
Nurses who suffered from hand dermatitis were more likely to have a history suggestive of eczema compared to those who did not have hand dermatitis. 42.9% of nurses who had hand dermatitis had a history suggestive of eczema compared to only 15.2% of subjects who did not have hand dermatitis, and this difference was significant (χ2=10.825, Phi=0.25, P<0.01). Similar association was observed between hand dermatitis and history of eczema as 46.2% of nurses who suffered from hand dermatitis had a history of eczema compared to only 5.4% of nurses who did not have hand dermatitis (χ2=26.493, Phi=0.384, P<0.001). Nurses who suffered from hand dermatitis were also more likely to have history of allergies compared to those who did not have hand dermatitis. 46.2% of subjects who suffered from hand dermatitis had a history of allergies compared to only 15.2% of subjects who do not have hand dermatitis and this difference was significant (χ2=5.970, Phi=0.21, P<0.02). This was reflected on both history of allergic rhinitis and history of allergies from dust, animals or plants as 61.5% of subjects who suffered from hand dermatitis had a history of allergic rhinitis compared to only 27.4% of subjects who did not have hand dermatitis (χ2=6.963, Phi=0.198, P<0.05) and 61.5% of subjects who had hand dermatitis had a history of allergies from dust, animals or plants compared to only 25.1% of subjects who did not have hand dermatitis (χ2=8.358, Phi=0.215, P<0.02) (Table 2).
| No hand dermatitis (n=167) n (n (%)) | Hand dermatitis (n=14) n (n (%)) | Total (n=181) n (n (%)) | Chi-square P-value | |
|---|---|---|---|---|
| Suffering from chronic diseases | ||||
| No | 145 (88.4%) | 12 (85.7%) | 157 (88.2%) | NS |
| Yes | 19 (11.6%) | 2 (14.3%) | 21 (11.8%) | |
| Caring for children under 4 | ||||
| No | 115 (69.7%) | 12 (85.7%) | 127 (70.9%) | NS |
| Yes | 50 (30.3%) | 2 (14.3%) | 52 (29.1%) | |
| Smoking | ||||
| No | 147 (88.0%) | 14 (100.0%) | 161 (89.0%) | NS |
| Yes | 20 (12.0%) | 0 (0.0%) | 20 (11.0%) | |
| History suggestive of eczema | ||||
| No | 139 (84.2%) | 8 (57.1%) | 147 (82.1%) | χ2=10.825 |
| Not sure | 7 (4.2%) | 0 (0.0%) | 7 (3.9%) | Phi=0.25 |
| Yes | 19 (11.5%) | 6 (42.9%) | 25 (14.0%) | P=0.004 |
| Skin dryness | ||||
| No | 128 (76.6%) | 9 (64.3%) | 137 (75.7%) | NS |
| Not sure | 9 (5.4%) | 2 (14.3%) | 11 (6.1%) | |
| Yes | 30 (18.0%) | 3 (21.4%) | 33 (18.2%) | |
| History of eczema | ||||
| No | 149 (89.2%) | 7 (53.8%) | 156 (86.7%) | χ2=26.493 |
| Not sure | 9 (5.4%) | 0 (0.0%) | 9 (5.0%) | Phi=0.384 |
| Yes | 9 (5.4%) | 6 (46.2%) | 15 (8.3%) | P<0.001 |
| History of asthma | ||||
| No | 143 (87.7%) | 11 (84.6%) | 154 (87.5%) | NS |
| Not sure | 6 (3.7%) | 0 (0.0%) | 6 (3.4%) | |
| Yes | 14 (8.6%) | 2 (15.4%) | 16 (9.1%) | |
| History of allergic rhinitis | ||||
| No | 107 (65.2%) | 4 (30.8%) | 111 (62.7%) | χ2=6.963 |
| Not sure | 12 (7.3%) | 1 (7.7%) | 13 (7.3%) | Phi=0.198 |
| Yes | 45 (27.4%) | 8 (61.5%) | 53 (29.9%) | P=0.031 |
| History of allergies from dust, animals or plants | ||||
| No | 114 (68.3%) | 4 (30.8%) | 118 (65.6%) | χ2=8.358 |
| Not sure | 11 (6.6%) | 1 (7.7%) | 12 (6.7%) | Phi=0.215 |
| Yes | 42 (25.1%) | 8 (61.5%) | 50 (27.8%) | P=0.015 |
| History of any allergies | ||||
| No | 139 (84.8%) | 7 (53.8%) | 146 (82.5%) | χ2=5.970 |
| Yes | 25 (15.2%) | 6 (46.2%) | 31 (17.5%) | Phi=0.21 |
| P=0.015 |
Table 2: Characteristics of nurses with and without hand dermatitis.
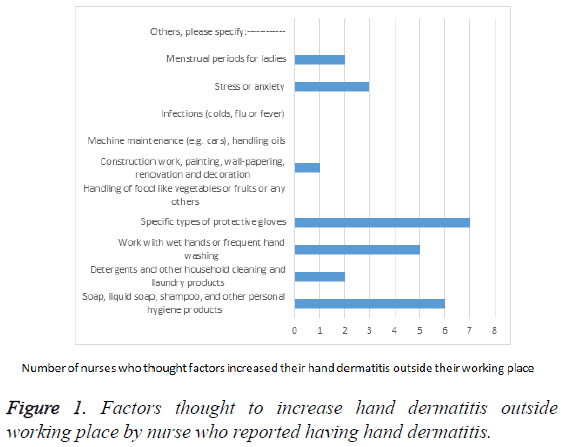
The nurses who reported having hand dermatitis symptoms were all female. Places of work were: 1 in emergency room, 3 in the operation room, 4 in the labor and delivery, 1 in the nursery, 1 in blood bank, 1 in outpatient department, 1 in the patient education department, 1 in nursing research and 1 in the nursing education department. In the past 6 months, 4 of them had it once and lasted for a week or less, one had it once and lasted for more than a week, one had it nearly once every month, one had it once every week, and one had it nearly all the time. The rest of them did not specify the incidence and duration of had dermatitis. Having hand dermatitis is thought to be caused by gloves or hand hygiene by 4 nurses, the others thought it was caused by water, climate or did not know the cause. Only 3 nurses saw a doctor for their hand condition, while 7 confirmed not seeing a doctor. In terms of time and season of having hand dermatitis, 5 nurses reported having it on work days, 3 had it in the very cold weather, and 2 with exposure to dust. On questioning whether hand eczema improves with long vacations from work, 5 replied yes, 4 replied no and one was not sure. The factors that increased hand conditions outside working place are presented in Figure 1. Gloves were mostly implicated, followed by soap, liquid soap, shampoo, and other personal hygiene products.
In terms of how did hand dermatitis affect daily activity, 3 nurses reported that they had to avoid doing some tasks in their job, 2 reported having difficulties in doing some tasks and none had to change or lost jobs or had to take sick leaves. Regarding the financial influence of hand dermatitis; 10 nurses reported that they were affected financially, 1 had some financial loss because of the problem and none had any substantial financial effect. Regarding the psychological effect of this condition, 6 reported no effect, 4 reported some anxiety or stress, and none reported any considerable effect on anxiety or stress, family problems, or depression. One nurse only reported that hand conditions caused a decrease in her self-confidence.
Discussion
The percentage of self-reported hand dermatitis was 7.73% in our study. The incidence of hand dermatitis among nurses varied in different countries in different studies. In Germany, the prevalence of hand eczema was reported to be 18% in a study on 1375 geriatric nurses from 86 nursing homes [11]. A questionnaire survey reported a 1 year prevalence of hand dermatitis of 21% among healthcare workers in three hospitals in Denmark [12]. The previous study indicated that hand dermatitis was positively associated with atopic dermatitis, younger age, male sex and working hours. Sick leave was reported by 8% of subjects in this previous study. In another questionnaire based study on nurses working in a regional hospital in Hong Kong (724 nurses), hand eczema prevalence was reported to be 22.1% [13]. In a Korean study of hand eczema among nurses in a general hospital, the proportion of self-reported hand eczema was 31% [14]. In a recent Turkish study on 158 pediatric nurses, the incidence of hand dermatitis was reported to be as high as 47.5% [15]. In this previous study nurses filled a questionnaire and were examined professionally. A 12 months period prevalence ranging from 43.2-59.3% was reported from a study conducted at a large tertiary hospital in Australia [16]. An even higher incidence was reported in a Canadian study that reported a 72% prevalence rate of mild, moderate/severe dermatitis among 183 health care workers in a large teaching hospital [17]. The response rate was low in this previous study (28%). This might have affected the prevalence rate as many hand dermatitis sufferers might have participated in the study. Similarly a very high prevalence of hand dermatitis was reported in another study [14]. They reported a 75.6% prevalence rate of symptom based frequency of hand dermatitis among 525 nurses in a single general hospital in Korea and 31% of self-reported hand eczema. Risk factors suggested in this previous study included young age, history of atopic dermatitis, frequent hand washing and long duration of glove wearing. This study also indicated that there was lower hand dermatitis incidence among frequent hand moisturizer users. The low incidence in our study in comparison to these studies might be attributed to the study method which depended on recall of symptoms without clinical examination. Additionally, half of the study population was working in clerical or administrative positions where there is no frequent contact with patients and no required frequent hand washing or wet work. These positions included patient education, nursing research, nursing administration, quality and nursing education.
The presence of hand dermatitis was associated with previous history of eczema, allergic rhinitis and previous allergies in this study. This is similar to findings in a study that investigated the impact of atopic eczema on the occurrence of hand dermatitis among nurses in Taiwan. This previous study suggested that atopic eczema is a major risk factor of hand dermatitis. It reported that 17% of nurses with hand dermatitis had a history of atopic eczema constitute only [18].
A systematic review and meta-analysis that analysed the association between smoking and hand dermatitis suggested that there is no confirmed association [19]. However, this meta-analysis suggested that the relation between smoking and hand dermatitis is not conclusive as its results depended mainly on two large studies (out of three included in the analysis) from one country. None of nurses suffering from hand dermatitis was a smoker in our study. This might be due to the small number of nurses who had hand dermatitis. Therefore, no conclusion can be drawn from this finding. Hand dermatitis in this study did not cause a considerable effect on daily activities, finance or psychological burden.
In this study the association of hand washing frequency with hand dermatitis could not be determined due to the variation in the responses as it was an open question. The responses included uncountable, many times and after each patient. In future studies, options of variable numbers can be used in order to get a more specified data. The other limitation of this study could be related to the type of data collection depending on recall of symptoms with no clinical confirmation of hand dermatitis.
Conclusion
In conclusion, the prevalence hand dermatitis among nurses represents an issue. Despite the fact that the prevalence rate in our study was not as high as the rates reported in other studies, hand dermatitis might need to be confirmed clinically and its prevalence need to be compared to the general population in our area. History of eczema, allergic rhinitis and history of allergies were risk factors for hand dermatitis.
Acknowledgement
To Dr. Sumia Enani for her assistance in statistical analysis and to Miss. Rehab Halawani for her assistance in distributing and collecting the questionnaires to departments at the hospital.
References
- Johansen JD, Hald M, Andersen BL, Laurberg G, Danielsen A, Avnstorp C, Kristensen B, Kristensen O, Kaaber K, Thormann J, Menne T, Veien N, Danish Contact Dermatitis Group. Classification of hand eczema: clinical and aetiological types. Based on the guideline of the Danish Contact Dermatitis Group. Contact Dermatitis 2011; 65: 13-21.
- Diepgen TL, Andersen KE, Chosidow O, Coenraads PJ, Elsner P, English J, Fartasch M, Gimenez-Arnau A, Nixon R, Sasseville D, Agner T. Guidelines for diagnosis, prevention and treatment of hand eczema-short version. J Dtsch Dermatol Ges 2015; 13: 77-85.
- Diepgen TL, Andersen KE, Chosidow O, Coenraads PJ, Elsner P, English J, Fartasch M, Gimenez-Arnau A, Nixon R, Sasseville D, Agner T. Guidelines for diagnosis, prevention and treatment of hand eczema-long version. J Dtsch Dermatol Ges 2015; 13: 1-22.
- Apfelbacher C, Molin S, Weisshaar E, Bauer A, Elsner P, Mahler V, Weiss M, Ruzicka T, Diepgen TL. Characteristics and provision of care in patients with chronic hand eczema: updated data from the CARPE registry. Acta Derm Venereol 2014; 94: 163-167.
- Higgins CL, Palmer AM, Cahill JL, Nixon RL. Occupational skin disease among Australian healthcare workers: a retrospective analysis from an occupational dermatology clinic, 1993-2014. Contact Dermatitis 2016; 75: 213-222.
- van der Meer EW, Boot CR, van der Gulden JW, Jungbauer FH, Coenraads PJ, Anema JR. Hand eczema among healthcare professionals in the Netherlands: prevalence, absenteeism, and presenteeism . Contact Dermatitis 2013; 69: 164-171.
- Thyssen JP, Johansem JD, Linneberg A, Menne T. The epidemiology of hand eczema in the general population-prevalence and main findings. Conatct Dermatitis 2010; 62: 75-87.
- Chen J, Gomez P, Kudla I, DeKoven J, Holness DL, Skotnicki S. Return to Work for Nurses With Hand Dermatitis. Dermatitis 2016; 27: 308-312.
- Sørensen JA, Fisker MH, Agner T, Clemmensen KK, Ebbehoj NE. Associations between lifestyle factors and hand eczema severity: are tobacco smoking, obesity and stress significantly linked to eczema severity? Contact Dermatitis 2017; 76: 138-145.
- Stocks SJ, McNamee R, Turner S, Carder M, Agius RM. The impact of national-level interventions to improve hygiene on the incidence of irritant contact dermatitis in healthcare workers: changes in incidence from 1996 to 2012 and interrupted times series analysis. Br J Dermatol 2015; 173: 165-171.
- Skudlik C, Dulon M, Wendeler D, John SM, Nienhaus A. Hand eczema in geriatric nurses in Germany-prevalence and risk factors. Contact Dermatitis 2009; 60: 136-143.
- Ibler KS, Jemec GB, Flyvholm MA, Diepgen TL, Jensen A, Agner T. Hand eczema: prevalence and risk factors of hand eczema in a population of 2274 healthcare workers. Contact Dermatitis 2012; 67: 200-207.
- Luk NM, Lee HC, Luk CK, Cheung YY, Chang MC, Chao VK, Ng SC, Tang LS. Hand eczema among Hong Kong nurses: a self-report questionnaire survey conducted in a regional hospital. Contact Dermatitis 2011; 65: 329-335.
- Lee SW, Cheong SH, Byun JY, Choi YW, Choi HY. Occupational hand eczema among nursing staffs in Korea: Self-reported hand eczema and contact sensitization of hospital nursing staffs. J Dermatol 2013; 40: 182-187.
- Ozyazicioglu N, Surenler S, Tanriverdi G. Hand dermatitis among paediatric nurses. J Clin Nurs 2010; 19: 1597-1603.
- Smith DR, Smyth W, Leggat PA, Wang RS. Prevalence of hand dermatitis among hospital nurses working in a tropical environment. Aust J Adv Nurs 2005; 22: 28-32.
- Nichol K, Copes R, Spielmann S, Kersey K, Eriksson J, Holness DL. Workplace screening for hand dermatitis: a pilot study. Occup Med (Lond) 2016; 66: 46-49.
- Lan CC, Tu HP, Lee CH, Wu CS, Ko YC, Yu HS, Lu YW, Li WC, Chen GS. Hand dermatitis among university hospital nursing staff with or without atopic eczema: assessment of risk factors. Contact Dermatitis 2011; 64: 73-79.
- Lukacs J, Schliemann S, Elsner P. Association between smoking and hand dermatitis-a systematic review and meta-analysis. J Europ Acad Dermatol Venereol 2015; 29: 1280-1284.