ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 22
Herb foot-bath has improving effects on sleep quality and symptom distress of maintenance hemodialysis patients
Lu Ren1, Jiuhong Li2, Xiaofei Zhang1, Jingxia Wang1, Wei Liu1, Jiarui Chen1 and Siyuan Tang1*
1Xiangya Nursing School of Central South University, Changsha, Hunan, PR China
2Intensive Care Unit of Cardiovascular Surgery, the Second Xiangya Hospital of Central South University, Changsha, Hunan, PR China
- *Corresponding Author:
- Siyuan Tang
Xiang Ya Nursing School of Central South University
Hunan, PR China
E-mail: renlu818@126.com
Accepted date: October 03, 2017
Hemodialysis (HD) is an incomplete renal substitutive therapy to interchange blood and dialyzate between semipermeable membrane so as to clean metabolic wastes and toxic products, maintain electrolyte and acid-base balance, and eliminate excessive moisture from body. Because of double affliction of the pain itself and treatment induced complication, most of Maintenance Hemodialysis (MHD) patients are bothered by influenced sleep quality and other symptom distress. In the study, we set out to investigate the intervention effect of herb foot-bath therapy to improve sleep quality and symptom distress for them. It was an experimental study in two stages including preliminary screening survey and herb foot-bath intervention. 142 MHD patients from Xiangya Hospital of Central South University and the Third Hospital of Central South University in accordance with inclusive criteria were randomly divided into control and intervention group. Patients in intervention group were intervened by regular herb foot-bath for 4 w. Pittsburgh Sleep Quality Index (PSQI) and Dialysis Symptom Index (DSI) were applied to quantify sleep quality and symptom distress of MHD patients. The data were analysis by SPSS19.0. The results showed that a majority of MHD patients were undergoing somnipathy and most of them experienced several symptoms at the same time with high scores of PSQI and DSI. Sleep quality was positively correlated with the symptom burden. To some extent, it was found that herb foot-bath therapy can effectively improve sleep quality of MHD patients and mitigate their symptom distress.
Keywords
Maintenance hemodialysis patients, Herb foot-bath, Sleep quality, Symptom distress, PSQI, DSI
Introduction
End Stage Renal Disease (ESRD), caused by irreversible loss of renal function to filter body metabolic wastes, salts and water, is the terminal stage of all progressive renal diseases [1]. The morbidity of ESRD is yearly increasing by 8% average with nearly 50-200 patients in one million natural populations worldwide [2]. At present, the most effective therapy of ESRD is still renal replacements, i.e. Hemodialysis (HD), Peritoneal Dialysis (PD) and kidney transplant. However, because of limiting factors of kidney transplant, such as expensive cost, limiting renal sources and high risk, a majority of ESRD patients still require Maintenance Hemodialysis (MHD) as substitutive therapy throughout their lives. Nowadays, with continuous improvement of HD technique and equipment, long-term survival rate of MHD patients is rising gradually, and the treatment goal of MHD is changed from prolonging survival time to improving life quality and social rehabilitation of patients [3,4].
Due to the pain of disease itself and complication induced by HD treatment , MHD patients are commonly bothered by influenced sleep quality and other symptom distress, which is closely related to their morbidity and death rate [5-7]. According to recent research, nearly 60-80% of MHD patients suffered from somnipathy which appears as poor quality of sleep, insomnia, fatigue and somnolence in the daytime, hypnotic dependence, restless legs syndrome, obstructive sleep apnea, etc. [8,9]. Moreover, through investigating physical health status of ESRD patients, most of patients were bothered by fatigue, pruritus, joint pain, crural paralysis, etc. [10-12]. Symptom of distress is changed with disease process and treatment, severity of which is influenced by numerous factors [13,14].
Several intervention therapies of somnipathy, at present, have been gained some therapeutic effects. Because of expensive cost and easy dependency of medicine therapy as well as difficult grasp and performance of rational-emotive therapy, muscle relaxation training and digital pressure therapy, herb foot-bath therapy is comparatively much easier to be accepted by patients [15-18]. To our knowledge, there is no such research on improving effect of herb foot-bath therapy on symptom distress and somnolence of MHD patients. Thereby, we set out to investigate the influence factors of symptom distress of MHD patients, and explore the intervention effect of herb foot-bath therapy to improve sleep quality and symptom distress for them. It was an experimental study in two stages including preliminary screening survey and herb foot-bath intervention. The theoretical basis of the study is Health Belief Model (HBM) which is extensively applied to forecast of short- and long-term health risk behavior and behavior change.
Materials and Methods
Object of study
MHD patients between 18 and 75 y old in Xiangya Hospital of Central South University and the Third Hospital of Central South University in accordance with inclusive criteria were investigated in the present study. The inclusive criteria are as follow: firstly, the period of MHD is over three months and no surgical operation and change in hemodialysis method are performed within three months; secondly, patient is in stable condition during the experiment; thirdly, patient is voluntary to participate the study with consent, understanding and cooperation. According to scoring method of Pittsburgh Sleep Quality Index (PSQI), MHD patient with over 7 total points was regarded as positive standard of screening. These selected patients were randomly divided into intervention group and control group.
Pittsburgh sleep quality index (PSQI)
PSQI was designed by Buysse et al. to evaluate sleep quality over one-month time interval [19]. The measure is made up by 19 individual items and invited by 7 components including subjective somnus quality, sleep latency, sleep time, sleep efficiency, somnipathy, hypnotic and daytime dysfunction. Every component is scored with 0-3. The total point of PSQI is cumulative score of each component in the range of 0 to 21. Higher total point signifies worse sleep quality of the testee. According to Chinese norm standard, total point of 7 is the boundary, above 7 refers to low amount of sleeping, the sensitivity is 98.3%, the specificity is 90.2% (Kappa=0.89, P<0.01).
Dialysis symptom index (DSI)
The scale of DSI, containing 5 mental and 25 physical symptoms, was designed by Steven [20]. The frequency and severity of symptom occurrence are involved in the investigation to assess emergent symptom and its frequency, severity and distress degree. The occurrence of symptom is analysed in the form of no or yes (no=0, yes=1). Its frequency and severity are measured through four-point Likert scale method: occasionally/slight=1; often/moderate=2; frequently/ severe=3; always/very serious=4. The degree of distress is tested via five-point Likert scale method: no distress=1; slight distress=2; moderate distress=3; severe distress=4; very severe distress. The higher scores indicate the more severe degree of distress. The scale is with 0.923 of Cronbach’s α and 0.939 of content validity.
Herb prescription
All the herbs were obtained from Longjiang Medicinal Materials Co. Ltd. (Heilongjiang, China). The herb prescription for intervention group was composed of 30 g Agastache rugosus, 15 g Herba eupatorii, 10 g Safflower carthamus, 30 g Radix rehmanniae recen, 20 g Angelica sinensis and 30 g Radix paeoniae alba. Herbs were packed by a gauze bag and handed out to patients in intervention group.
Herb foot-bath treatment
Herbs packed by gauze bag were put into a footbath with boiled water. Firstly, feet were put above the footbath in water vapor. Until the water temperature was cooled to 38-43°C, feet were put in water for foot bath. During the time of foot bath, the height of water should be over ankles but below knees. If it cooled down, hot water could be added to keep the temperature of water suitable. A course of treatment was four weeks; the intervention time was before nightly bedtime every day. The duration of each intervention time was 30-40 min, if patient was older than 70, 30 min or below of foot bath was better. Once symptoms such as uncomfortableness, profuse sweating, tachycardia and dizziness occurred, patient should stop the intervention and rest in bed. After foot bath, foot should be dried and kept warm. All situations of intervention including any uncomfortable symptom have to be recorded every day.
Data collection
Questionnaires were distributed and withdrew on the spot. In principle, the questionnaire was filled out by the patient autonomously. Requirements and appeared doubts about the questionnaire were explained by the unified instruction to maintain completeness and correctness.
Statistical analysis
Database was set up by the means of SPSS19.0. Data was double checked and input by two persons. Statistical significance was defined as P<0.05.
Results
Over four fifths of MHD patients were bothered by somnipathy
The base line results of PSQI showed that 27 cases of patients (18.89%) slept well, and 116 cases (81.11%) suffered from somnipathy. The mean score of PSQI was 10.96 ± 4.46. The average scores were respectively 1.62 ± 0.838 of subjective sleep quality, 2.03 ± 1.077 of the time of falling sleep, 1.81 ± 1.081 of sleeping time, 1.61 ± 1.139 of sleeping effect, 1.54 ± 0.591 of the handicap of sleeping, 0.43 ± 1.003 of the drugs of hypnosis and 1.92 ± 0.953 of function handicap in daytime (Table 1).
| Factor | Score () |
|---|---|
| Subjective somnus quality | 1.62 ± 0.838 |
| Sleep latency | 2.03 ± 1.077 |
| Sleep time | 1.81 ± 1.081 |
| Sleep efficiency | 1.61 ± 1.139 |
| Somnipathy | 1.54 ± 0.591 |
| Hypnotic | 0.43 ± 1.003 |
| Daytime dysfunction | 1.92 ± 0.953 |
| PSQI total score | 10.96 ± 4.455 |
| Data were presented as mean ± SD, n=142. | |
Table 1: The PSQI score of MHD patients.
MHD patients suffered from different degree of symptom distress
The prevalence of every distress symptom was 13.3-72 %. The mean total score of distress symptom was 76.69 ± 37.95, lack of strength, dry mouth, festless sleep, difficulty in falling sleeping, sexual hypoactivity, difficulty in sexual excitement, pruritus, dysphoria, worry and edema of lower extremity were ten most frequently occurred symptoms with over 50% of incidence rate. The most severe symptoms were difficulty in falling sleep, restless leg, festless sleep, lack of strength and anhelation (Table 2). The most frequently occurred symptoms were difficulty in falling sleep, festless sleep, lack of strength, anorexia and dry mouth. Multivariable stepwise regression indicated that symptom distress was statistically correlated to the total score of PSQI, the education level and the course time of chronic renal disease of MHD patients in the study (P<0.05). By the means of Spearman correlate test, it was showed that the total score and each dimensionality of PSQI were positively correlated with those of DSI, which implied the positive correlation of sleep quality and symptom distress (Table 3).
| Item | Score range | Score () |
|---|---|---|
| DSI total score | 60-360 | 76.69 ± 37.95 |
| Degree | 0-120 | 23.36 ± 11.02 |
| Frequency | 30-120 | 29.83 ± 14.64 |
| Severity | 30-120 | 24.51 ± 12.74 |
| Occurrence number | 0-30 | 13.12 ± 5.27 |
| Data were presented as mean ± SD, n=142. | ||
Table 2: The DSI score of MHD patients.
| Item | DSI total score | Degree | Frequency | Severity |
|---|---|---|---|---|
| PSQI total score | 0.527** | 0.516** | 0.522** | 0.525** |
| Subjective somnus quality | 0.439** | 0.445** | 0.426** | 0.437** |
| Sleep latency | 0.246** | 0.262** | 0.232** | 0.242** |
| Sleep time | 0.410** | 0.399** | 0.406** | 0.421** |
| Sleep efficiency | 0.469** | 0.449** | 0.475** | 0.465** |
| Somnipathy | 0.356** | 0.351** | 0.354** | 0.356** |
| Hypnotic | 0.230** | 0.218** | 0.239** | 0.212* |
| Daytime dysfunction | 0.417** | 0.392** | 0.418** | 0.415** |
| Data were presented as mean ± SD, n=142, *P<0.05 and **P<0.01 vs. control group. | ||||
Table 3: Correlation analysis of sleep quality and symptom distress of MHD patients.
Herb foot bath decreased total score of PSQI in intervention group
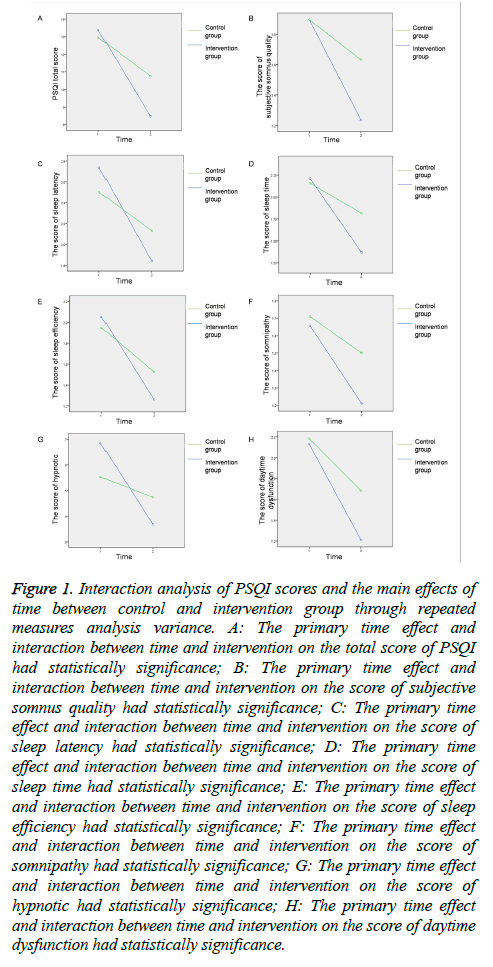
Through comparing the PSQI scores in control and intervention group, it was detected by two independent-samples t-test and Mann-Whitey U test that there were significant differences in PSQI total score, subjective somnus quality, sleep time, somnipathy and daytime dysfunction between two groups (P<0.05) (Table 4). Paired-samples t-test and nonparametric Wilcoxon test showed that the score of PSQI in intervention group was declined markedly after intervention (P<0.05). In the control group, however, there was no statistics significance in the dimensions of subjective somnus quality, sleep latency, sleep time, sleep efficiency, somnipathy and hypnotic (P>0.05) (Table 5). Through repeated measures analysis variance, it was found that the main effects time on PSQI and the interactions between time and intervention on above variations were both statistically significant (Figure 1).
| Item | Intervention group | Control group | Z | P |
|---|---|---|---|---|
| PSQI total score | 8.47 ± 2.82 | 10.76 ± 3.04 | -2.98 | 0.003** |
| Subjective somnus quality | 1.24 ± 0.59 | 1.63 ± 0.71 | -2.237 | 0.025* |
| Sleep latency | 1.84 ± 0.82 | 2.13 ± 0.91 | -1.498 | 0.141 |
| Sleep time | 1.37 ± 0.85 | 1.82 ± 0.97 | -2.073 | 0.038* |
| Sleep efficiency | 1.26 ± 0.98 | 1.53 ± 0.91 | -1.23 | 0.231 |
| Somnipathy | 1.21 ± 0.17 | 1.50 ± 0.37 | -2.444 | 0.015* |
| Hypnotic | 0.37 ± 0.75 | 0.47 ± 0.96 | -0.19 | 0.831 |
| Daytime dysfunction | 1.21 ± 0.70 | 1.68 ± 0.71 | -2.333 | 0.019* |
| Data were presented as mean ± SD, n=142, *P<0.05 and **P<0.01 vs. control group. | ||||
Table 4: Comparison of PSQI scores between control and intervention group through t-test and Mann-Whitney U test.
| Item | Intervention group | z | P | Control group | z | P | ||
|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | |||||
| PSQI total score | 13.37 ± 3.26 | 8.47 ± 2.82 | -5.39 | 0.000** | 12.95 ± 3.14 | 10.76 ± 3.04 | -5.236 | 0.000** |
| Subjective somnus quality | 1.89 ± 0.73 | 1.24 ± 0.59 | -4.33 | 0.000** | 1.89 ± 0.79 | 1.63 ± 0.71 | -1.456 | 0.145 |
| Sleep latency | 2.74 ± 0.55 | 1.84 ± 0.82 | -5.26 | 0.000** | 2.16 ± 0.82 | 2.13 ± 0.91 | -1.742 | 0.081 |
| Sleep time | 2.21 ± 0.94 | 1.37 ± 0.85 | -4.768 | 0.000** | 1.95 ± 1.06 | 1.82 ± 0.97 | -1.512 | 0.13 |
| Sleep efficiency | 2.03 ± 1.05 | 1.26 ± 0.98 | -4.817 | 0.000** | 1.95 ± 1.06 | 1.53 ± 0.91 | -1.929 | 0.054 |
| Somnipathy | 1.66 ± 0.53 | 1.21 ± 0.17 | -3.9 | 0.000** | 1.71 ± 0.61 | 1.50 ± 0.37 | -1.598 | 0.11 |
| Hypnotic | 0.69 ± 1.21 | 0.37 ± 0.75 | -3.051 | 0.002** | 0.55 ± 1.11 | 0.47 ± 0.96 | -1.732 | 0.083 |
| Daytime dysfunction | 2.13 ± 0.84 | 1.21 ± 0.70 | -4.917 | 0.000** | 2.18 ± 0.87 | 1.68 ± 0.71 | -2.512 | 0.012* |
| Data were presented as mean ± SD, n=71, *P<0.05 and **P<0.01 vs. control group. | ||||||||
Table 5: Comparison of PSQI scores between pre- and post-intervention by the means paired-samples t-test and nonparametric Wilcoxon test.
Figure 1: Interaction analysis of PSQI scores and the main effects of time between control and intervention group through repeated measures analysis variance. A: The primary time effect and interaction between time and intervention on the total score of PSQI had statistically significance; B: The primary time effect and interaction between time and intervention on the score of subjective somnus quality had statistically significance; C: The primary time effect and interaction between time and intervention on the score of sleep latency had statistically significance; D: The primary time effect and interaction between time and intervention on the score of sleep time had statistically significance; E: The primary time effect and interaction between time and intervention on the score of sleep efficiency had statistically significance; F: The primary time effect and interaction between time and intervention on the score of somnipathy had statistically significance; G: The primary time effect and interaction between time and intervention on the score of hypnotic had statistically significance; H: The primary time effect and interaction between time and intervention on the score of daytime dysfunction had statistically significance.
Herb foot bath decreased total score of DSI in intervention group
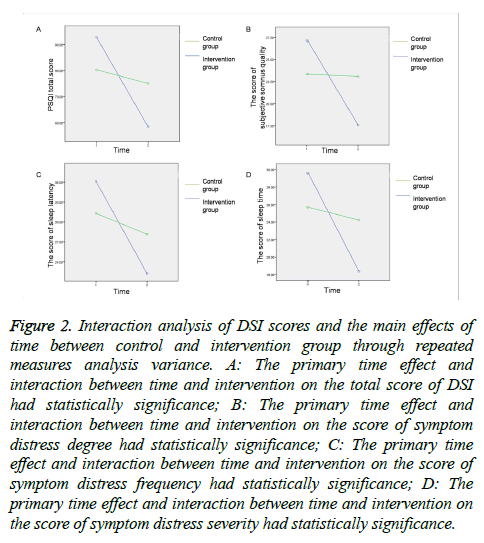
By the means of independent-samples t-test and Mann- Whitney U test to compare the DSI scores in control and intervention group, there were significant differences found in the total scores of DSI, the degree of symptom distress, the severity of symptom and the occurrence number of symptom between two groups (P<0.05) (Table 6). The results of paired-samples t-test and nonparametric Wilcoxon test showed that after intervention, the DSI scores in intervention group was reduced obviously but not significantly changed in control group. The differences in the DSI score, the degree of symptom distress, the frequency of occurred symptom, the severity of symptom and the number of symptom between the pre- and post-intervention were significant (P<0.05) (Table 7). Repeated measures analysis of variance showed that the main effects of time on DSI were statistically significant (P<0.05). There were significant interactions between time and intervention on the total score of DSI and other dimensions (P<0.05) (Figure 2).
| Item | Intervention group | Control group | t/z | P |
|---|---|---|---|---|
| DSI total score | 58.45 ± 20.12 | 75.08 ± 34.09 | -2.026^ | 0.043* |
| Degree | 17.57 ± 5.82 | 23.08 ± 9.86 | -2.367^ | 0.018* |
| Frequency | 22.24 ± 8.23 | 28.16 ± 13.44 | -1.862^ | 0.063 |
| Severity | 18.37 ± 6.75 | 24.24 ± 11.22 | -2.253^ | 0.024* |
| Occurrence number | 10.37 ± 3.66 | 12.76 ± 4.59 | -2.51 | 0.014* |
Table 6: Comparison of DSI scores between control and intervention group through t-test and Mann-Whitney U test.
| Item | Intervention group | t | P | Control group | z/t | P | ||
|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | |||||
| DSI total score | 92.87 ± 35.69 | 58.45 ± 20.12 | 13.849 | 0.000** | 80.34 ± 37.96 | 75.08 ± 34.09 | -2.381∆ | 0.017* |
| Degree | 27.13 ± 10.14 | 17.57 ± 5.82 | 12.34 | 0.000** | 23.34 ± 10.79 | 23.08 ± 9.86 | -0.029∆ | 0.977 |
| Frequency | 36.13 ± 13.74 | 22.24 ± 8.23 | 17.404 | 0.000** | 31.32 ± 15.0 | 28.16 ± 13.44 | -3.418∆ | 0.001** |
| Severity | 29.61 ± 12.36 | 18.37 ± 6.75 | 11.142 | 0.000** | 25.68 ± 12.65 | 24.24 ± 11.22 | -1.647∆ | 0.099 |
| Occurrence number | 14.66 ± 4.62 | 10.37 ± 3.66 | 14.746 | 0.000** | 13.89 ± 5.43 | 12.76 ± 4.59 | 2.726 | 0.010** |
| Data were presented as mean ± SD, n=71, ^refers to z, *P<0.05 and **P<0.01 vs. control group. | ||||||||
Table 7: Comparison of DSI scores between pre- and post-intervention by the means paired-samples t-test and nonparametric Wilcoxon test.
Figure 2: Interaction analysis of DSI scores and the main effects of time between control and intervention group through repeated measures analysis variance. A: The primary time effect and interaction between time and intervention on the total score of DSI had statistically significance; B: The primary time effect and interaction between time and intervention on the score of symptom distress degree had statistically significance; C: The primary time effect and interaction between time and intervention on the score of symptom distress frequency had statistically significance; D: The primary time effect and interaction between time and intervention on the score of symptom distress severity had statistically significance.
Discussion
The study investigated sleep quality and symptom distress of 142 MHD patients, and probed into the effects of herb footbath on them. PSQI and DSI were utilized to quantify sleep quality and symptom distress of MHD patients. According to our results, sleep quality was positively correlated with the symptom burden. To some extent, it was found that herb foot-bath therapy can effectively improve sleep quality of MHD patients and mitigate their symptom distress.
We found about 81.11 % of them suffered from somnipathy, and the ratio of disturbed patients in the present study was in accord with the results in previously publicated researches [21,22]. The total score of PSQI was detected to be 10.96 ± 4.46. In the study, the prevalence of somnipathy was high, which probably resulted from long course of disease induced complicated state and complication of patients. MHD patients of the study generally had more than five year of course of disease, and most of them were gerontal patients who may have been troubling but neglected sleep problems and had never took improvement measures, resulting in increasingly severe sleep disorder. Most of MHD patients mainly complained of difficulty in falling sleep, poor quality of sleep, festless sleep, short sleep time and low sleep efficiency. Because of disrupted circadian rhythm induced by insomnia, the physical and psychological health of these patients were badly influenced by somnolence and lack of strength in the daytime, which further affecting their living quality.
The number of symptom distress in the study was found to be 3-25, averagely 13.12 ± 5.27 per patient, and the total DSI score of symptom distress was in the range of 12 to 193, averagely 76.69 ± 37.95. The results demonstrated that the majority of MHD patients were undergoing various painful symptoms distress simultaneously. As MHD patients suffered from double affliction of somatization from disease itself and relative symptoms induced by dialysis treatment which reduced quality of life, symptom distress was further aggravated. Moreover, we found symptoms with highest degree were difficulty in falling sleep, restless leg, festless sleep, anhelation and lack of strength; the most frequently occurred symptoms were difficulty in falling sleep, festless sleep, lack of strength, anorexia and dry mouth; the most severe symptoms were respectively difficulty in falling sleep, restless leg, festless sleep, lack of strength and anhelation. To our knowledge, it has been documented that sexual dysfunction was one of symptoms troubled MHD patients badly, but it was not reflected in the study [11,23]. The difference probably resulted from traditional concept of Chinese patients and shame in answering sexual dysfunction related questions.
Through correlation analysis of symptom distress and each dimension of PSQI scale, it was detected that the degree, prevalence and severity of symptom distress were all positively correlated PSQI total score, subjective somnus quality, sleep latency, sleep time, sleep efficiency, somnipathy, hypnotic and daytime dysfunction, which indicated that sleep improvement was able to mitigate symptom distress of MHD patients.
Based on Chinese medicine, Chronic Renal Failure (CRF), which is induced by inherent shortage, improper diet, emotional disturbance and recurrent renal diseases, is involved in categories of obstruction and rejection, retention of urine and consumptive disease. Damaged spleen and kidneys, damp turbidity, stasis toxin and internal stagnation are considered as the main mechanisms of CRF. As there exists numerous reflecting regions and acupuncture points on sole of foot, foot is closely related to kidney. The prescription for intervention group was made up by Agastache rugosus, Herba eupatorii, Safflower carthamus, Radix rehmanniae recen, Angelica sinensis and Radix paeoniae alba. Agastache rugosus is an aromatous Chinese medicine which has function of inducing perspiration and resolving dampness [24]. Herba eupatorii can dissolve turbidities and repel foulness [25]. Safflower carthamus is able to invigorate the circulation of blood, stimulate menstrual flow, and improve microcirculation of heart and brain [26]. Radix rehmanniae recen possesses sedative effect, mitigates symptoms of patient with hypertension, and obviously improve hypertension induced insomnia [27]. Angelica sinensis has a lot of functions including immuno-enhancement, protection of the liver and kidney function, improvement of renal blood flow, oxidation resistance, ameliorating renal fibrosis, promotion of hematopoiesis, etc. Radix paeoniae alba has effective of nourishing blood and liver and retaining yin with astringent [28,29].
After intervention of herb foot-bath, the score of PSQI, subjective somnus quality, sleep latency, sleep time, somnipathy and daytime dysfunction of patients in intervention group were significantly decreased in comparison with control group. In addition, by self-comparison, total PSQI score and score in each dimension were also obviously reduced after herb foot-bath compared to pre-intervention. In the study, we found that sleep quality of MHD patients was obviously improved after intervention of herb foot-bath compared with control group, which implied that herb foot-bath could effectively mitigate somnipathy and improve sleep quality of MHD patients. After intervention of herb foot-bath, compared with control group, the total DSI score and scores of the degree, severity and occurrence number of symptom distress were decreased markedly with significant differences. By comparing pre- and post-intervention, the total score of DSI and the scores in dimension of the degree, prevalence, severity and numbers of symptom distress were substantially reduced in intervention group, which indicated the improving effect of herb foot-bath on symptom distress. Herb foot-bath intervention mitigated the degree and severity of symptom distress, and reduced its prevalence and occurrence number. Given the limitation of the study, there may exist placebo effects on the results between control and intervention groups, which is required to be further studied in the future.
Conclusion
Most of MHD patients suffered from somnipathy and most of them experienced several symptoms at the same time with high scores of PSQI and DSI. The sleep quality was positive correlated with the symptom burden. To some extent, herb foot-bath therapy can effectively improve sleep quality of MHD patients and mitigate their symptom distress.
Acknowledgements
This work was supported by the National Science Foundation of China (Grant number: 81370974) and the Fundamental Research Funds for the Central Universities of Central South University (Grant number: 2015zzts107).
References
- Saran R, Li Y, Robinson B, Abbott KC, Agodoa LY, Ayanian J, Hirth RA. US renal data system 2015 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2016; 671-305.
- Xue JL, Ma JZ, Louis TA, Collins AJ. Forecast of the number of patients with end-stage renal disease in the United States to the year 2010. J Am Soc Nephrol 2001; 12: 2753-2758.
- Ismail N, Hakim RM, Helderman JH. Renal replacement therapies in the elderly: Part II. Renal transplantation. Am J Kidney Dis 1994; 23: 1-15.
- Turk S, Atalay H, Altintepe L, Guney I, Okudan N, Tonbul HZ, Yildiz A. Treatment with antidepressive drugs improved quality of life in chronic hemodialysis patients. Clin Nephrol 2006; 65: 113-118.
- Davison SN, Jhangri GS. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manag 2010; 39: 477-485.
- Gurklis JA, Menke EM. Identification of stressors and use of coping methods in chronic hemodialysis patients. Nurs Res 1988; 37: 236-248.
- Mapes DL, Lopes AA, Satayathum S, McCullough KP, Goodkin DA, Locatelli F, Port FK. Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int 2003; 64: 339-349.
- Lui SL, Ng F, Lo WK. Factors associated with sleep disorders in Chinese patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 2002; 22: 677-682.
- Parker KP. Sleep disturbances in dialysis patients. Sleep Med Rev 2003; 7: 131-143.
- Abdel-Kader K, Unruh ML, Weisbord SD. Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol 2009; 4: 1057-1064.
- Weisbord SD, Fried LF, Arnold RM, Fine MJ, Levenson DJ, Peterson RA, Switzer GE. Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 2005; 16: 2487-2494.
- Yong DS, Kwok AO, Wong DM, Suen MH, Chen WT, Tse DM. Symptom burden and quality of life in end-stage renal disease: a study of 179 patients on dialysis and palliative care. Palliat Med 2009; 23: 111-119.
- Sawicki GS, Sellers DE, Robinson WM. Self-reported physical and psychological symptom burden in adults with cystic fibrosis. J Pain Symptom Manage 2008; 35: 372-380.
- Silveira MJ, Kabeto MU, Langa KM. Net worth predicts symptom burden at the end of life. J Palliat Med 2005; 8: 827-837.
- David D, Szentagotai A, Lupu V, Cosman D. Rational emotive behavior therapy, cognitive therapy, and medication in the treatment of major depressive disorder: a randomized clinical trial, posttreatment outcomes, and six-month follow-up. J Clin Psychol 2008; 64: 728-746.
- Sacks SB. Rational emotive behavior therapy: disputing irrational philosophies. J Psychosoc Nurs Ment Health Serv 2004; 42: 22-31.
- Shariati A, Jahani S, Hooshmand M, Khalili N. The effect of acupressure on sleep quality in hemodialysis patients. Complement Ther Med 2012; 20: 417-423.
- Yurtkuran M, Alp A, Yurtkuran M, Dilek K. A modified yoga-based exercise program in hemodialysis patients: a randomized controlled study. Complement Ther Med 2007; 15: 164-171.
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193-213.
- Weisbord SD, Fried LF, Arnold RM, Rotondi AJ, Fine MJ, Levenson DJ, Switzer GE. Development of a symptom assessment instrument for chronic hemodialysis patients: the Dialysis Symptom Index. J Pain Symptom Manag 2004; 27: 226-240.
- Celik G, Annagur BB, Yilmaz M, Demir T, Kara F. Are sleep and life quality of family caregivers affected as much as those of hemodialysis patients? Gen Hosp Psychiatry 2012; 34: 518-524.
- Pai MF, Hsu SP, Yang SY, Ho TI, Lai CF. Sleep disturbance in chronic hemodialysis patients: the impact of depression and anemia. Ren Fail 2007; 29: 673-677.
- Claxton RN, Blackhall L, Weisbord SD, Holley JL. Under treatment of symptoms in patients on maintenance hemodialysis. J Pain Symptom Manage 2010; 39: 211-218.
- Zhao S, Zhao L, Xue L, Lin L, Quan L. Effects of HE particles on medicinal plant Agastache rugosus (Fisch. et Mey.) O. Ktze. Zhongguo Zhong Yao Za Zhi 1997; 22: 721-763.
- Fan WL, Guo LW, Lin Y, Shen J, Cao GP, Zhu Y, Yang L. Study on effect of oil-bearing solution environment of Caryophylli Flos and other traditional Chinese medicines on system flux and oil recovery rate. Zhongguo Zhong Yao Za Zhi 2013; 38: 3277-3281.
- Costa LR, Macedo PC, de Melo JS, Freitas CM, Alves AS, Barbosa HM, Lagranha C. Safflower (Catharmus tinctorius L.) oil supplementation in overnourished rats during early neonatal development: effects on heart and liver function in the adult. Appl Physiol Nutr Metab 2016; 41: 1271-1277.
- Liu C, Ma R, Wang L, Zhu R, Liu H, Guo Y, Gao S. Rehmanniae radix in osteoporosis: A review of traditional Chinese medicinal uses, phytochemistry, pharmacokinetics and pharmacology. J Ethnopharmacol 2017; 198: 351-362.
- Hua Y, Yao W, Ji P, Wei Y. Integrated metabonomic-proteomic studies on blood enrichment effects of Angelica sinensis on a blood deficiency mice model. Pharm Biol 2017; 55: 853-863.
- Wang K, Tang Z, Wang J, Cao P, Li Q, Shui W, Zhang Y. Polysaccharide from Angelica sinensis ameliorates high-fat diet and STZ-induced hepatic oxidative stress and inflammation in diabetic mice by activating the Sirt1-AMPK pathway. J Nutr Biochem 2017; 43: 88-97.