ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 4
Hyperglycaemia in the emergency department: stress hyperglycaemia or diabetes mellitus
1Department of Emergency Medicine, Karabuk University, Karabuk, Turkey
2Department of Internal Medicine, Tokat State Hospital, Tokat, Turkey
3Department of Family Practice, Faculty of Medicine, Karabuk University, Karabuk, Turkey
4Department of Emergency Medicine, Faculty of Medicine, Gaziosmanpasa University, Tokat, Turkey
5Department of Emergency Medicine, Karabuk Education and Research Hospital, Karabuk, Turkey
6Department of Emergency Medicine, Corum State Hospital, Corum, Turkey
7Department of Emergency Medicine, Sisli Hamidiye Etfal Education and Research Hospital, Istanbul, Turkey
Accepted on August 9, 2016
Stress Hyperglycaemia (SH) evolving especially in the acute period of diseases and in post-traumatic patients is appeared in many diabetic and non-diabetic patients. Patients with undiagnosed diabetes mellitus may also present with complications of diabetes, with 5% fatal courses. The aim of this study was to determine the incidence of diabetes mellitus in patients who applied to Emergency Department (ED) for various reasons. The files of the patients were retrospectively examined. The patients were divided into the following groups: Group 0: No prior diagnosis of diabetes. Group 1: Stress hyperglycaemia. Group 2: Diabetes mellitus. Group 3: The patients had not been diagnosed with diabetes mellitus before visiting the emergency department, and they were not taking any treatment for diabetes. Group 4: Newly diagnosed diabetes mellitus. Group 2 had the highest number of patients (64.4%), followed by Group 3 (10.4%), Group 4 (4.3%), and Group 0 (4.1%). The highest average blood glucose values were found in Group 2 (258.00), followed by Group 3 (230.00), and Group 4 (237.00). Undiagnosed patients with diabetes mellitus risk can apply with complications, and this not only threatens the lives of these patients but also dramatically reduces their quality of their life. It should be considered that there could be diabetes mellitus patients, as well as stress hyperglycaemia patients, with a high blood sugar level, in the emergency department. Thus, we believe that patients diagnosed with a high blood sugar level should be advised to attend their family practices and/or a polyclinic for disease monitoring, with follow-up in an endocrine unit.
Keywords
Stress hyperglycaemia, Diabetes mellitus, Emergency department.
Introduction
Diabetes mellitus (DM) is one of the most important reasons of mortality and morbidity, and its frequency is increasing because of aging population and obesity. All international organizations, especially the World Health Organization, have set down diagnostic criteria based on the direct Plasma Glucose measurement (PG) for diabetes mellitus diagnosis [1]. These diagnostic criteria are below: random plasma glucose ≥ 200 mg/dl in addition to symptoms of diabetes, plasma glucose ≥ 126 mg/dl after minimum 8 hours fasting or plasma glucose ≥ 200 mg/dl in the Oral Glucose Tolerance Test after 2 hours fasting (OGTT) [2,3].
According to the TURDEP-II’s study which was conducted between January 2010 and June 2010, the frequency rate of diabetes mellitus among the adult Turkish is 13.7% and the frequency rate of diabetes mellitus has increased within 12 years. According to the results of that study obesity and diabetes are the most important health problems of Turkish people today [4].
Definition of Stress Hyperglycaemia (SH) was first mentioned by Claude Bernard in 1877 and stress hyperglycaemia is one of the most common clinical situations in the Emergency Department (ED). Stress hyperglycaemia, which emerges especially in the acute period of diseases and in post-traumatic patients, is diagnosed in many diabetic and non-diabetic emergency department patients [5]. Undiagnosed diabetes mellitus patients could also have complications of diabetes with 5% fatal courses [6]. Hyperglycaemia is considered as stress hyperglycaemia in the emergency department. However, it is unknown if patients have early-stage diabetes mellitus when they applied to the emergency department with stress hyperglycaemia [7].
The aim of this study is to determine the incidence of diabetes mellitus in patients who applied to emergency department with 200 mg/dl or more blood glucose level for various reasons. This will lead us to determine what is advantageous for the patients and diabetes mellitus examination in terms of health policies and what is needed for further evaluation of diabetes mellitus patients with high blood sugar and without a history of diabetes mellitus.
Material and Methods
Ethics committee’s approval was taken for this study from the head of Bulent Ecevit University Clinical Research Ethics Committee (21/10/2015; protocol number 2015-86-21/10). Patients who applied to Emergency Department of the Training and Research Hospital for various reasons between the dates of 01/01/2014 and 30/06/2015 and who had a blood glucose level of ≥ 200 mg/dl were identified through the hospital’s information system. These patients’ files were retrospectively examined. Demographic data, blood glucose levels, diagnoses in the emergency department and medical histories before and after the emergency department were examined. Also answers of these questions were recorded: “Did patient receive a diagnosis of diabetes earlier?”, “Did patient consult the emergency department without an appointment?” and “Was patient examined after multiple applications to the emergency department?” Lastly, patients’ blood sugar levels after applying to the emergency department were recorded.
The patients were divided into five different groups. These groups are as the following:
Group 0: Patients who applied only once to the hospital with plasma glucose ≥ 200 mg/dl and without prior diagnosis of diabetes.
Group 1: Patients applying to our hospital more than one except for emergency department visits with plasma glucose level>120 mg/dl. These patients were diagnosed with stress hyperglycaemia and they had never been diagnosed with diabetes mellitus according to their patient files.
Group 2: Patients diagnosed with diabetes mellitus before applying to the emergency department. They were receiving treatment for diabetes mellitus.
Group 3: Patients who were not diagnosed with diabetes mellitus before visiting the emergency department, despite having plasma glucose level ≥ 200 mg/dl in examinations in polyclinic visits (excluding internal medicine, endocrine diseases and family practice polyclinics). They were not taking any treatment for diabetes.
Group 4: Patients who were not diagnosed with diabetes mellitus before applying to the emergency department. They were diagnosed with diabetes mellitus according to detection of plasma glucose level ≥ 200 mg/dl in examinations in the emergency department visits and they commenced treatments. This group was classified as newly diagnosed diabetes mellitus.
These patients were excluded from the study:
*Patients who applied to the emergency department with diabetes and diabetes-related complications.
*Patients who have history of malignancy.
*Patients diagnosed as gestational diabetes.
*Patients under the age of 18.
Statistical analysis
All phenotypes were subjected to the Anderson-Darling test before the statistical analyses. The results showed that the phenotypes’ distribution was not normal. Therefore, the Kruskal-Wallis test was used for multiple comparisons and the Mann-Whitney U test was used as a post-hoc test. And also a chi-squared test was used.
Findings
In the study, 46.6% of patients were males and the rest of them were females. There were 3299 patients in the four groups. Group 2 had the highest number of patients (n=2124; 64.4%). It was followed by Group 3 (n=343; 10.4%), Group 4 (n=142; 4.3%) and Group 0 (n=137; 4.1%). There was not a significant statistical difference among the patient groups in terms of gender as shown in Table 1.
| Group 0 | Group 1 | Group 2 | Group 3 | Group 4 | Total | |
|---|---|---|---|---|---|---|
| Male | 81 | 278 | 943 | 166 | 70 | 1538 |
| Female | 56 | 275 | 1181 | 177 | 72 | 1761 |
| Total | 137 | 553 | 2124 | 343 | 142 | 3299 |
*There is no statistically significant difference when patient groups are examined in terms of gender.
Table 1. Evaluating the patients groups in terms of gender*.
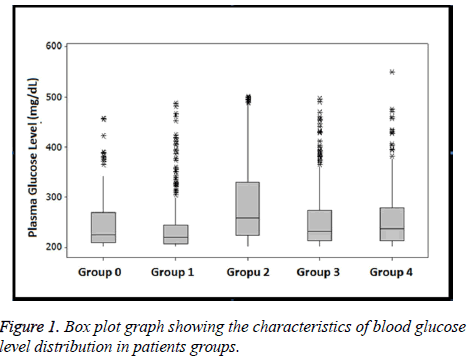
The highest average blood glucose values were found in Group 2 (258.00) and it was followed by Group 3 (230.00) and Group 4 (237.00). As we see in Table 2, there was not a significant statistical difference among the average blood glucose levels of the patient groups shown in Table 2 and Figure 1.
| Patients group | n | % | Blood glucose level average value (Q1-Q3) |
|---|---|---|---|
| Group 0 | 137 | 4.1% | 225.00 (207.50-268.50) |
| Group 1 | 553 | 16.8% | 219.00 (207.00-244.00) |
| Group 2 | 2124 | 64.4% | 258.00 (223.00-329.75) |
| Group 3 | 343 | 10.4% | 230.00 (212.00-273.00) |
| Group 4 | 142 | 4.3% | 237.00 (212.00-279.25) |
Table 2. Introductory statistics in terms of value of diabetes for patient groups. Average value (Q1-Q3)).
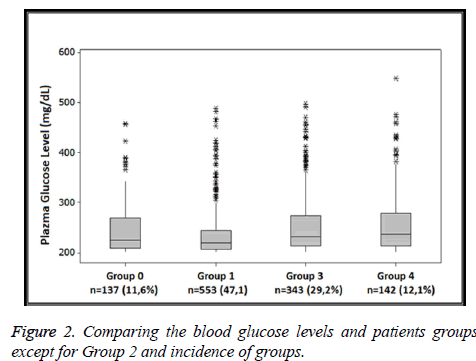
Group 2 was excluded from the analysis and other patient groups (1175 patients) were re-evaluated using the Kruskal- Wallis test. After visiting the emergency department 11.6% of the patients in Group 0 (n=137), 47.1% of the patients in Group 1 (n=553), 29.2% of the patients in Group 3 (n=343) and 12.1% of the patients in Group 4 (n=142) were diagnosed with diabetes and they had high blood sugar levels as shown in Table 3.
| Group 0 | Group 1 | Group 3 | Group 4 | |
|---|---|---|---|---|
| Group 1 | 0.0526 | 0.0000 | 0.0000 | |
| Group 3 | 0.1342 | 0.0000 | 0.5131 | |
| Group 4 | 0.0606 | 0.0000 | 0.5131 |
Table 3. The difference between groups (Mann-Whitney U test).
As we see in Table 3 and Figure 2, there is a difference between Group 0 and other groups and between Group 3 and Group 4 but there is not a significant difference between Group 1, Group 3 and Group 4.
Discussion
According to the World Health Organization’s Global Situation Report on NCD’s in 2010, number of fatal and nonfatal cardiovascular cases could be reduced by at least 30% due to taking diabetes mellitus under control. Diabetes mellitus patients use health services two or three times more than patients without diabetes. Furthermore, approximately 15% of national health expenditures are spent for the care of diabetes mellitus patients. Impaired glucose tolerance and impaired fasting glucose are major risk factors for diabetes mellitus and cardiovascular diseases. According to researches, the risk of stroke of diabetes mellitus patients in developed countries is twice as much than those without diabetes mellitus and they have 10 times greater risk in lower limb amputation [2]. It is estimated that there were 382 million diabetics in the world in 2013, also it is expected that this number is going to reach 592 million in 2035. The majority of diabetes mellitus cases are in low- or middle-income countries. Nearly half (46%) of diabetes mellitus cases are not diagnosed. Frequency of diabetes mellitus was estimated as 8.3% among between the ages of 20 and 79. Diabetes mellitus caused 5.1 million deaths in the world and at least 548 billion dollars was spent on diabetes mellitus in 2013. Turkey (2011) was in the 4th place in European countries with 8.1% frequency rate of diabetes mellitus and 3.6 million diabetes mellitus cases [4,8,9].
An increase in catabolic hormones and hepatic gluconeogenesis could be seen in inpatients as well as hyperglycaemia based on peripheral and hepatic insulin resistance. It is considered as an adaptive response to provide fuel for noninsulin-dependent tissues (e.g. elytron, central nervous system) in acute disease states. Excessive dextrose could also increase hyperglycaemia. Studies have shown that mortality was much higher in stress hyperglycaemia compared to diabetes-induced hyperglycaemia. Stress hyperglycaemia patients commonly recover after acute diseases. 60% of patients who were diagnosed with hyperglycaemia in the hospital were diagnosed with diabetes, so patients should be followed up. The oral glucose tolerance test was previously recommended to assess carbohydrate metabolism disorders for patients diagnosed with stress hyperglycaemia just after discharge from the hospital. Although, current guidelines suggest that HbA1c should be measured. According to the criteria of the ADA, an HbA1c level ≥ 6.5 is indicative of diabetes [3,7,10,11].
In the study by Kilic et al. on type 2 diabetes mellitus risk prediction, 55.8% of patients in the community were male patients [8]. However, a study on the frequency of type 2 diabetes mellitus in Turkey did not find any difference between males and females in terms of the development of the disease [12]. According to the literature there are differences between the gender ratios of diabetes mellitus patients and newly diagnosed diabetes mellitus patients, there was still no statistical difference between genders. In the present study, 46.6% of the patients were men and the rest of them were women as shown in Table 1. This is consistent with the literature data.
According to the former study of the incidence of type 2 diabetes mellitus in Turkey, the annual growth in number of newly diagnosed diabetes mellitus cases was 19,050 and the authors predicted that this number would increase over years [12]. In the study of Olveira et al. on diabetes prevalence in Spain, they found that there were people with diabetes mellitus (17%), people who previously did not know their diabetes mellitus (4.3%) and people with stress hyperglycaemia (7.1%) [13]. The rate of stress hyperglycaemia in Group 1 was 16.8% as shown in Table 2 and Figure 1 in this study. We attributed the percentage of stress hyperglycaemia, which is higher than the rate reported in the literature, to our study’s working area (Emergency Department).
In the study of Yigit et al. on patients diagnosed with diabetic ketoacidosis in emergency department, they found that 21% of patients were newly diagnosed with diabetes [7]. The authors of this study pointed out further tests to detect diabetes mellitus were not conducted in patients diagnosed with high blood sugar level but without history of diabetes mellitus. They stated that a high blood sugar level could denote traumatic or metabolic stress in patients applying to the emergency department with complications such as diabetic ketoacidosis. In this study, there is no one who applied to our hospital more than once and who had high blood sugar level, except for their examination in our hospital in Group 1 patients. Also diabetes mellitus was not recorded in any of the patients’ medical records. Thus, these patients (16.8%) were diagnosed with stress hyperglycaemia as shown in Figure 1 and Table 1. When it is evaluated (except for Group 2 diabetes mellitus patients), Group 1 which is considered as stress hyperglycaemia has the highest rate with 47.1% as shown in Figure 2. In our study stress hyperglycaemia level is expected high in services having high endogenous and exogenous stress levels such as emergency department, which is consistent with the literature. In the study of Koyuncu et al. on 59 KDA patients, they realized that 15 patients were not diagnosed with diabetes mellitus and they did not take any treatment [14]. In this study, the rate of Group 4 which could be defined as a new diagnosis of diabetes is about 10.4% as we see in Table 2 and Figure 1. We attributed the difference between the rates of undiagnosed diabetes compared to rates in the literature due to the lack of information on patients’ fates in Group 0 and Group 3.
In the study of Kilic et al. on development of diabetes mellitus prevalence in Yozgat, they saw that diabetes mellitus risk was high in 11.2% of the patients and higher in 0.4% of the patients. That study emphasized the importance of blood glucose measurement in terms of diabetes mellitus disease complications and the importance of counselling to people in the risk group [8]. Bayrak et al. pointed out that diabetes mellitus education could improve the patient’s life quality and facilitate the work of healthcare personnel when the patients have knowledge about their diseases and actions to be taken in that situation. Also the importance of taking under control of the disease was emphasized for reducing of material and nonmaterial casualties.
In this study, the rate of Group 0 with patients who applied just once (except for diabetes mellitus patients) is 11.06% as we see in Figure 2. It is unknown whether these patients were later diagnosed with diabetes mellitus. In our opinion, these patients could be visitors who reside in other cities. However, the percentage of diabetes mellitus was substantial (29.2%) in Group 3 which contained patients with high blood sugar levels and without a diagnosis of diabetes mellitus and any treatment as shown in Figure 2. As stated previously, patients with undiagnosed diabetes mellitus could apply with complications and have high mortality and morbidity rates [8,15]. Therefore, we believe that patients with diabetes mellitus risk should be identified, treated and trained about diabetes mellitus as soon as possible.
Conclusions
Undiagnosed patients with diabetes mellitus risk could apply with complications and this situation not only threatens the lives of these patients but it also reduces their quality of life dramatically. It should be considered that there could be diabetes mellitus patients in the emergency department, as well as stress hyperglycaemia patients with high blood sugar level. Therefore we believe that patients diagnosed with a high blood sugar level should be recommended to apply their family practices and/or a polyclinic for disease monitoring and followup.
Limitations
We were unable to assess the status of the patients in Group 0 because we could not see the entire country’s health system. When higher number of patients are surveyed or/and prediabetes and metabolic diseases are examined, more precise comments could be made. We did not examine symptoms and diagnosis for all patients. We think examination for symptoms and diagnosis strengthens the value of the study.
References
- Steinberg MB, Randall J, Greenhaus S, Schmelzer AC, Richardson DL. Tobacco dependence treatment for hospitalized smokers: a randomized, controlled, pilot trial using varenicline. Addict Behav 2011; 36: 1127-1132.
- World Health Organization. Global status report on non-communicable diseases 2010.Switz WHO Press 2011.
- Association AD. Standards of medical care in diabetes-2013. Diabetes Care 2013; 36: 11-36.
- Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol 2013; 28: 169-180.
- Henderson WR, Chittock DR, Dhingra VK, Ronco JJ. Hyperglycemia in acutely ill emergency patients-cause or effect? CJEM 2006; 8: 339-343.
- Durukan P, Koyuncu M, Salt O, Kavalci C, Ozkan S, Muhtaroglu S. Comparison of ischemia modified albumin levels with total oxidant, total antioxidant status, oxidative stress index in carbon monoxide poisoning. Acta Medica Mediterranea 2014; 30: 601-605.
- Yigit Y, Ozucelik DN, Ayhan H, Gencer EG, Karakum M. Evaluation of the new diagnosis of diabetes patients suffering with diabetic ketoacidosis apply to emergency services. Med Bull Haseki 2013; 51: 168-172.
- Kilic M, Cetinkaya F, Kilic AI. Predicting risk of type 2 diabetes mellitus: A population-based study. J Clin Anal Med 2015; 6: 850-854.
- Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014; 103: 137-149.
- Khunti K, Gray LJ, Skinner T, Carey ME, Realf K, Dallosso H, Fisher H, Campbell M, Heller S, Davies MJ. Effectiveness of a diabetes education and self-management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ 2012; 344: e2333.
- Smith FG, Sheehy AM, Vincent JL, Coursin DB. Critical illness-induced dysglycaemia: diabetes and beyond. Crit Care 2010; 14: 327.
- Onat A, Hergenc G, Uyarel H, Can G, Ozhan H. Prevalence, incidence, predictors and outcome of type 2 diabetes in Turkey. Anadolu Kardiyol Derg 2006; 6: 314-321.
- Olveira G, Tapia MJ, Ocon J, Cabrejas-Gomez C, Ballesteros-Pomar MD, Vidal-Casariego A, Arraiza-Irigoyen C, Olivares J, Conde-Garcia MC, Garcia-Manzanares A, Botella-Romero F, Quilez-Toboso RP, Cabrerizo L, Matia P, Chicharro L, Burgos R, Pujante P, Ferrer M, Zugasti A, Petrina E, Manjon L,Dieguez M, Carrera MJ, Vila-Bundo A, Urgeles JR, Aragon-Valera C, Sanchez-Vilar O, Breton I, Garcia-Peris P, Munoz-Garach A, Marquez E, Del Olmo D, Pereira JL, Tous MC. Prevalence of diabetes, prediabetes, and stress hyperglycaemia: insulin therapy and metabolic control in patients on total parenteral nutrition (prospective multicenter study). Endocr Pract 2015; 21: 59-67.
- Koyuncu M, Ozturk D, Altinbilek E, Yapar N, Karakisa H, Kavalci C, Ikizceli I. Effects of drug use on the development of diabetic ketoacidosis. Acta Medica Mediterranea 2015; 31: 1013-1017.
- Bayrak G, Colak R. Patient education on diabetes treatment. J Exp Clin Med 2012; 29: 7-11.