ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 1
Impact of maternal nutrition on birth weight of babies.
1Department of Public Health, School of Health Sciences, University of Venda, P/Bag X5050, Thohoyandou 0950, South Africa
2Department of Community Medicine, Faculty of Public Health, University College Hospital, Ibadan, Nigeria
- *Corresponding Author:
- A. M. Amosu
Department of Public Health
School of Health Sciences
University of Venda, P/Bag X5050
Thohoyandou 0950, South Africa
Accepted October 11 2013
This is a cross-sectional and descriptive study of pregnant mothers who delivered in four randomly selected health facilities in urban Abeokuta, Nigeria. The study examined the influence of maternal nutritional status on newborn birth weight and particularly low birth weight (LBW). Five hundred and twelve pregnant mothers booked for antenatal care and were attending antenatal clinics were recruited for the study as they became available. Complete physical examination, clinical profile along with weight, biochemical and haematological measurements were carried out. Data were analyzed using descriptive statistics and chi-square test. The mean weight gain of the pregnant mothers in this study was 7.78 ± 1.01 kg. Weight gain in pregnancy, maternal haemoglobin, mean corpuscular haemoglobin concentration, serum cholesterol and serum albumin were all found to be significant for LBW (p<0.001). Maternal nutritional status impacted significantly on newborn birth weight as poorly nourished mothers were observed to produce a higher percentage of LBW babies when compared to those who were better nourished.
Keywords
Maternal nutritional status, low birth weight, antenatal care, maternal haemoglobin
Introduction
Birth weight (BW) is the single most predictive factor of mortality in the first few months of life [1], and a baby's birth weight is an important indicator of his health. The World Health Organization (WHO) defined low birth weight (LBW) as that below 2,500gm [2]. It is a major public health problem in most African countries [3], and in most developing countries, being associated with a high incidence of neonatal mortality in these regions. In India 85% of neonatal mortality is associated with LBW, 87% in Guatemala and 56% in North Acrot [4]. It is estimated worldwide that 25 million LBW infants were born in 1990, making up to 18% of all live births, 90% of which occurs in developing countries [5]. LBW babies are at the greatest risk in early childhood. BW below 2.5kg reflects intrauterine malnutrition involving micro-nutrient deficiencies, infections such as malaria and syphilis, and maternal malnutrition. The incidence of LBW is therefore a powerful indicator of infant survival, and indirectly of the mother’s nutritional status [6]. In Nigeria, the average prevalence of LBW is estimated to be about 16%, with a range of 6-21% [7]. The immediate consequences are higher morbidity and mortality rates in the perinatal and neonatal periods [8]. The late consequences may include prolonged impairment of immunological defense mechanisms [9], and neurological sequelae [10] which interfere with the normal development of the child and on a national level, are serious obstacles to development. Among the causes of LBW, maternal malnutrition has been identified as one of the main determinants [11]. Maternal morbidity during pregnancy is highly prevalent in the low socio-economic groups [12] and protective mechanisms such as the bactericidal zinc peptide system in the amniotic fluid [13], may be impaired partly because of malnutrition during pregnancy [14].
This study was therefore designed to investigate the effect of maternal nutritional status on the BW of the newborn in urban Abeokuta, Nigeria.
Material and Methods
This is a cross-sectional and descriptive study design for booked pregnant mothers who delivered in four randomly selected health facilities in urban Abeokuta, Nigeria. The study was carried out between January and September, 2012. The subjects were selected from each health facility as they became available. Five hundred and twelve randomly selected pregnant mothers attending antenatal clinics in the health facilities were booked and advised to report regularly for antenatal care. Complete abdominal examination, clinical profile along with height, weight, weight gain in pregnancy, blood pressure, haematological and biochemical examinations were carried out. All the newborns were weighed and their general physical conditions assessed immediately following delivery. All infants weighing below 2.5 kg were recorded as low birth weight (LBW) babies.
Statistical Analysis
Data were collated according to the various maternal nutritional characteristics included in the study. Analysis was carried out using descriptive statistics and chi-square test of significance was employed in testing for association between two variables.
Results
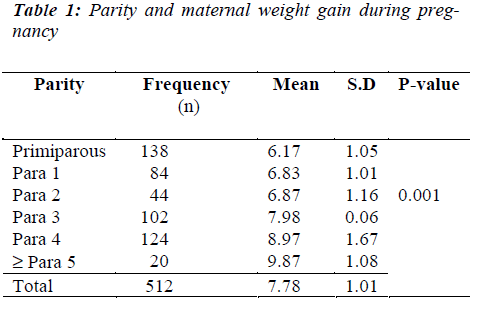
The mothers’ weights were measured before and immediately after delivery of the baby, placenta and membranes. Primiparous mothers were found to gain significantly less weight than multiparous mothers (p<0.05).
The mean weight gain in this study population was 7.78 ± 1.01 kg. Primiparous mothers recorded the lowest mean weight gain of 6.17 ± 1.05 kg, weight gain in pregnancy increasing with increase in parity as seen in Table 1.
Triceps skin fold thickness of the mothers as measured using a Harpenden caliper was expressed as a percentage of normal values [15]. This variable indicates the amount of adipose tissue in the upper arm, with primiparous mothers recording lower percentage than the multiparae.
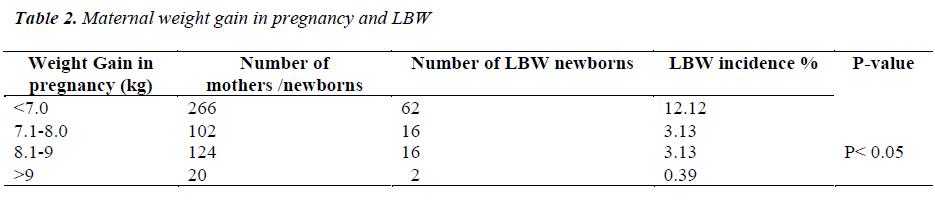
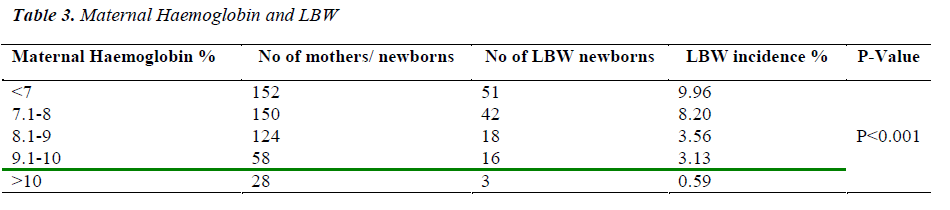
Table 2 shows the association between maternal weight gain in pregnancy and LBW incidence in all the deliveries. Weight gain of 7kg and below was associated with 12.12% LBW incidence, while mothers who gained 9kg and above, recorded the lowest LBW incidence of 0.39%. Table 3 summaries the relationship between maternal haemoglobin (Hb) level and LBW incidence. Mothers with Hb below 7g % had the highest incidence of LBW (9.96%) while those with Hb of 10g% and above recorded the lowest LBW incidence of 0.59%.
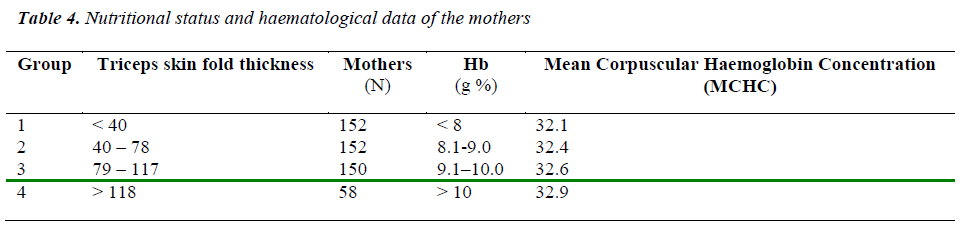
Those mothers with very low triceps skin fold thickness (<40% of normal value) had significantly lower Hb and MCHC values (Table 4). Furthermore, anaemic mothers (those with low Hb and MCHC levels), were also found to have lower serum albumin and cholesterol levels than non-anaemic mothers.
Discussion
Low birth weight (LBW) is a major public health problem due to its association with high morbidity and mortality of infants. Newborn mortality and disease are directly related to birth weight (BW), and insufficient or excess weight at birth is always accompanied by an increase of these risk factors. The relationship between weight gain in pregnancy and newborn birth weight has been known for several decades [16], and even now its importance to pregnancy outcome is being increasingly recognized. This importance is reflected in the recommendation that pregnant women should be encouraged to gain at least 11kg during gestation [17].
Results from this study have shown that several maternal nutritional parameters: weight, weight gain in pregnancy, triceps skin fold thickness, serum albumin and anaemia (low Hb and MCHC levels) significantly influenced the BW of infants. Primiparous mothers were shown to be at particular risk of delivering LBW babies. This agrees with previous works on pregnancy weight gain in that mothers with higher weight gain in pregnancy delivered lesser number of LBW babies [16]. Mothers whose Hb was below 7g% were associated with the highest percentage of LBW, while with increasing maternal Hb level, LBW incidence decreased. This is also in conformity with results from studies by earlier researchers [18] and [19].
Conclusion
In conclusion, this study has established that maternal nutritional status impacted significantly on newborn birth weight, as poorly nourished mothers were observed to produce a higher percentage of LBW babies in comparison to those who were better nourished. The challenge of addressing the problem therefore remains an urgent imperative for development.
References
- FAO/WHO International conference on nutrition— Major issues for nutrition strategies, Rome, 1992; 66 (2) 182-198
- Kramer MS. Determinants of LBW, Methodological assessment and meta analysis. Bull. WHO 1987; 65(5):663-737
- Wilcox AJ. On the importance – and the unimportance– of birth weight. International Journal of Epidemiology 2001; 30:1233-41
- Asthworth A; Feachem R .G. Interventions for the con- trol of Diarrhoeal diseases among young children. Pre- vention of low birth weight: Bull. WHO, 1985; 63(1) 165-184
- Bale JR, Stoll BJ, Lucas AO, editors. Improving birthoutcomes: meeting the challenge in the developing world. Washington, DC: The National Academies Press; 2003.
- Allen LH, Gillespie SR. What works? A review of the efficacy and effectiveness of nutrition interventions. Geneva: United N a t i o n s A d m i n i s t r a t i v e C o m m i t t e e o n C o o r d i n a t i o n Subcommittee on Nutri- tion; 2001.
- Federal Ministry of Health. Infant and Young Child Feeding in Nigeria; Guidelines: A publication of Fed- eral Ministry of Health, Department of Development and Population Activities, Nutrition Division Abuja, Nigeria, 2005, Pg 28.
- Osrin D, de L Costello A M. Maternal nutrition and fetal growth: practical issues in International health. Semi- nars in Neonatology, 2000; 5:209-19.
- Ferguson A.C. Prolonged Impairment of Cellular Im- munity in Children with intrauterine growth retarda- tion. J. Paediatr. 1998; 93, 52-56.
- Davies P.A. and Stewart A.L. Low Birth Weight in- fants: Neurological sequence and later intelligence. Br. Med. Bull. 1995; 31, 85-91.
- Lechtig A; Yazbrough C; Delgando H; Habitch J.PMartorell. R; Klein R.E. Influence of maternal nutrition on birth weight. Am. J.Clin Nutr 1975; 28, 1, 223
- Lechtig A; Yazbrough C; Delgando H; Habitch J.P Martorell. R; Klein R.E. Effect of morbidity during pregnancy on birth weight in a rural Guartemalan popu- lation. Ecol. Food Nutr. 1976; 5: 225-233.
- Schlievert P; Johnson W; Galask R.P (1976): Bacterial growth inhibition by amniotic fluid. Evidence for a zinc- peptide antibacterial system. Am. J. Obstet . Gy- naecol. 1976; 125: 900-910.
- Naeye R.L; Tafari N; Judge D; Gilmour D; Malboe C. Amniotic fluid infections in an African city. J. Paediat, 1997; 965-972.
- Jelliffe D.B. The assessment of nutritional status of the community. WHO Monogr. Ser. No 53. Geneva, 1966.
- Beilly J.S; Kurkland I. I. The relationship of maternal weight gain and weight of newborn infants. Am.J. Ob-stet. Gynaecol. 1945; 50: 202-206.
- United Nations Administrative Committee on Coordi- nation Subcommittee on Nutrition. Mainstreaming nutrition: opportunities to improve development out- comes. Fifth report on the world nutrition situation. Geneva: United Nations Administrative Committee on Coordination Subcommittee on Nutrition; 2004.
- Bhatia B.D; Sur A.M; Tyagi N.K. LBW babies in rela- tion to nutritional status and primipara. Indian J Paed 1981; 27 (23): 507
- Chadha V.K;Bachani D; Chawla S.C; Bansal R.D. Nu- tritional status of urban poor mothers and birth weight. J Obst Gynae. 1992; 46 (6): 278-292.