ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 3
In house developed SEVATB ELISA for ruling out tuberculosis in suspected cases of Extra Pulmonary Tuberculosis, a six month Retrospective study in a tertiary care hospital.
1Dept. of Biochemistry & JBTDRC, MGIMS, Sevagram, Maharashtra, India
2JBTDRC, MGIMS, Sevagram, Maharashtra, India
3Dept. of Orthopedics, MGIMS, Sevagram, Maharashtra, India
- *Corresponding Author:
- B. C. Harinath
JB Tropical Disease Research Centre
Mahatma Gandhi Institute of Medical Sciences
Sevagram-442 102 (Wardha) Maharashtra, India
Accepted date: April 05 2014
Evaluation of SEVA TB ELISA using cocktail of mycobacterial antigens ES-31 and EST-6 (containing ES-38 and ES-41 ) and their specific antibodies in diagnosis of suspected cases of extrapulmonary tuberculosis. Detection of circulating free and immune complexed antigen to specific antibodies by sandwich ELISA and antibody to cocktail of antigens ES-31 and EST-6 by indirect ELISA and was carried out in clinically suspected cases of extra pulmonary tuberculosis during a period of six months. Absence of antigen and antibody is considered as negative ELISA. 146 suspected cases of extrapulmonary tuberculosis were screened by SEVA TB ELISA on request by clinicians. 112 cases out of 146 showed negative ELISA test out of which 108 cases were not recommended ATT. The test showed 96% corelation with ELISA negativity and no ATT treatment. Further four cases showing ELISA negativity were advised ATT. These cases need follow up for the development of TB disease or effectiveness ATT of treatment in context to clinical relief. This study showed usefulness of SEVA TB ELISA as a adjunct test for ruling out TB in clinically suspected cases of extrapulmonary tuberculosis.
Keywords
Mycobacterial ES antigens, ES-31, EST-6, SEVA TB ELISA, extra-pulmonary tuberculosis
Introduction
An increasing trend was observed in extra pulmonary tuberculosis during last decade due to HIV infection [1]. EPTB constitutes almost 15-20% of all cases of tuberculosis while it is more than 50% in HIV positive individuals [2]. Many factors such as difficulty in a reliable test, drug administration for long duration, nonresponse to treatment, HIV infection and recently multi drug resistant and extensively drug resistant tuberculosis are contributing for lack of success in its management and control. Main challenge in EPTB is the difficulty in precise diagnosis as it has number of ways of presentation as per the involvement of organ. It has been observed that most of the patients with EPTB have generalized symptoms like fever, weakness, loss of appetite, etc. Many times patient may come with repeated fever i.e. pyrexia of unknown origin and mostly disease in obscure site [2]. These are conditions where clinicians are really in stressful dilemma in confirming diagnosis as well as starting ATT treatment. The existing gold standard test for confirmation of tuberculosis is AFB screening in specimen samples of EPTB cases. However procuring specimen samples is difficult in all EPTB cases as these cases have atypical presentations, and may yield poor positive yield. Another diagnosing aid, X-ray cannot differentiate soft tissue abscess and swelling due to tuberculosis. Improved version of culture media like BACTEC and MJIT are not much popular as they require expert personnels and are costly to maintain in resource limited hospitals. Due to lack of standard diagnostic protocol for extra-pulmonary tuberculosis and number of obstacles for reaching exact diagnosis result in involuntarily delays for starting ATT treatment. It is also equally important to consider diagnosing possibility of EPTB with AFB negative cases. HIV positive patients with AFB negative tuberculosis are generally more immnunocompromised and mortality rates are more in them demanding alternative approaches of diagnosis. All these reasons demand a sensitive, reliable, simple, cost effective test, and it should not depend on the immune response of subject in particularly immunocompromized HIV cases for diagnosis of extra-pulmonary tuberculosis. In our earlier study we have demonstrated usefulness of SEVA TB ELISA in diagnosing TB infection as a adjunct test in addition to other laboratory investigations [3]. In this study we evaluate study the usefulness of SEVA TB ELISA negativity in ruling out TB infection and solving the dilemma of clinician whether to start or not ATT in suspected EPTB cases.
Materials and Methods
Serum from clinically suspected cases of 146 extra pulmonary tuberculosis patients who attended Kasturba Hospital from April to September 2012 were screened by ELISA on clinicians request using cocktail (ES-31 + EST-6) antigen and specific antibodies (anti ES-31 + anti EST-6 IgG) for detection of antibody and circulating free and immune complexed antigen respectively [3]. Absence of both antigen and antibody is considered as ELISA negative and correlated with anti tuberculosis therapy.
Results
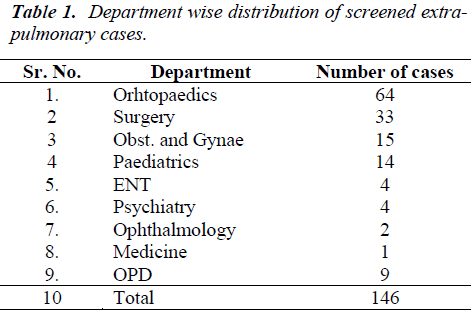
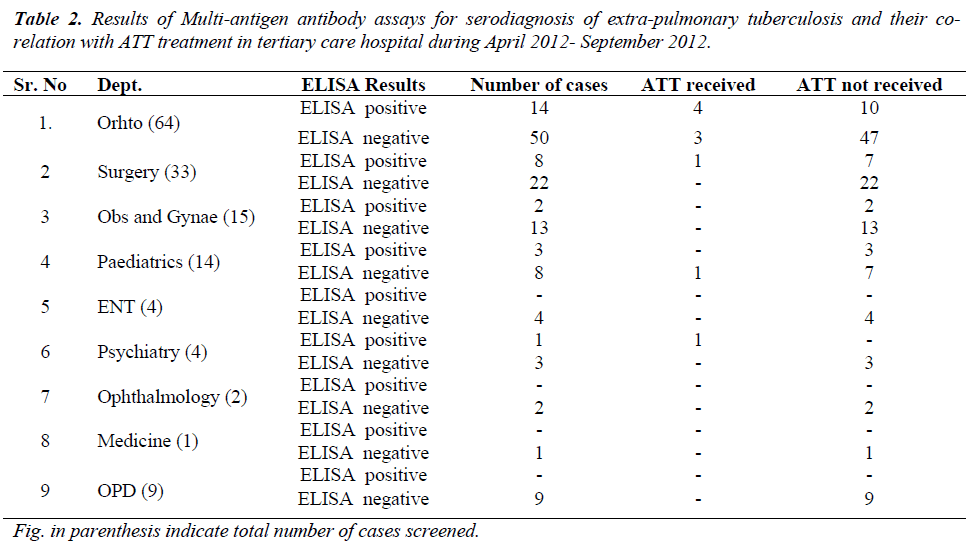
During study period a total 146 clinically suspected cases of extra-pulmonary were screened by SEVA TB ELISA and clinical department wise distribution of cases is given in (Table 1). Details of ELISA results and ATT treatment were given in Table 2. Out of 64 cases of extra pulmonary tuberculosis from department of orthopedics 14 cases were ELISA positive out of which 4 received ATT treatment, and 50 cases were ELISA negative out of which 47 cases were not given ATT treatment. Similarly out of 33 cases from surgery dept. were screened for SEVA TB ELISA and 22 were ELISA negative and none of ELISA negative cases received ATT treatment strongly co-relating ELISA negativity with absence of ATT. Out of 15 cases of OBGY department 13 were ELISA negative and 2 were ELISA positive and no one was given ATT. One ELISA negative case of pediatric department has received ATT on strong clinical suspicion and other laboratory investigation and other 7 cases which were negative for ELISA were not given ATT. 4 cases from each ENT and psychiatry dept. were screened for SEVA TB ELISA and 7 were negative and did not receive ATT. One case of psychiatry department was given ATT treatment which was ELISA positive, which was diagnosed as a case of neuropsychiatric manifestation of tubercular meningitis or encephalitis with mental retardation.
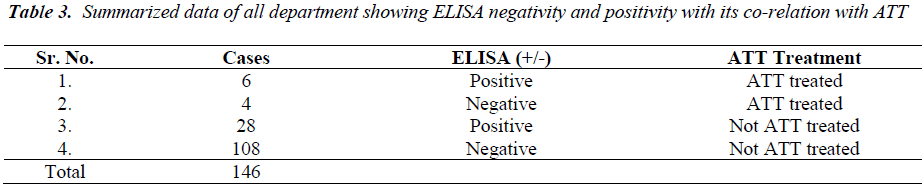
Thus SEVA TB ELISA showed 96% co-relation with ELISA negativity and absence of ATT. A total of total 108 cases out of 112 (table-3) which were suspected for extra-pulmonary tuberculosis were found to be ELISA negative and did not receive ATT. Thus SEVA TB ELISA helped clinician to rule out suspicion and not to start ATT thus preventing toxic effects of ATT in these suspected clinical cases. Only four ELISA negative out of 112 cases were treated with ATT on strong clinical grounds and other laboratory investigations. Six ELISA positive cases received ATT showing 100% co-relation with ELISA positivity and ATT treatment, and 28 cases did not receive ATT though they were ELISA positive.
Discussion
Taking into the account of the reported data [1], to minimize risk from emerging threat of EPTB morbidity and mortality; most effective way out would be early diagnosis and early start of ATT treatment. As there is no gold standard test for confirmation of EPTB infection, clinician has to relay mainly on patients disease history and symptomatology, followed by some laboratory investigations like X-ray, MRI, FNAC, cytological study of aspirated biological fluids. As all these procedures are painful, patients are not ready to undergo such procedures. Moreover results of bacillary culture fluids by BACTEC, MJIT are also questionable due to low bacillary density or wrong specimen collection in inaccessible body parts and are not cost effective. Similar is the case with other investigations like PCR, gamma interferon assays, demanding expertise personnel to carry out besides increased cost. In absence of standard recommended test for diagnosis of EPTB, patients were treated on the basis of clinical symptomatology like weight loss, fever, chronic cough, weakness etc, Clinician also tries short term treatment with higher antibiotics, and if symptoms are not relieved then they go for ATT and such cases were named as response to treatment, on failure of high version antibiotics trial.
Simpler serological tests can be answer for all these problems faced in diagnosis of EPTB in smaller hospitals along with other laboratory investigation and strong clinical suspicion. Serological test is not dependent on site of infection and easy to interpret. Over two decades, Jamanalal Bajaj tropical Disease Research Centre is actively involved in screening of pulmonary cases and extra-pulmonary cases with in house developed SEVA TB ELISA. Earlier studies from our laboratory reported diagnostically important antigens that are ES-31, ES-41, ES-38and ES-43 and detection of their antibodies by penicillinase and more user friendly peroxisdase ELISA [4]. A cocktail of ES 31 and ES-41, ES-38 had shown improved sensitivity when compared with single ES-31 antigen [4]. In house developed SEVA TB ELISA was shown as an important adjunct test in confirming tuberculosis infection of both pulmonary and extra pulmonary cases [3,5]. In this retrospective study we have evaluated usefulness negativity of SEVA TB ELISA in ruling out TB in suspected cases of EPTB and not putting the subject on ATT thus preventing toxic effects of ATT and trauma to the patients.
In present study, ELISA has shown (108 out of 112 ELISA negative) 96% correlation with ELISA negativity and not receiving ATT treatment in suspected subjects of EPTB. ELISA has helped the clinician in a way out from in dilemma, whether a suspected case need to put on ATT or not. Thus SEVA TB ELISA assisted in decreasing active disease case load and also prevented unwanted toxic effects by therapeutic trial in suspected people. SEVA TB ELISA has been helpful as adjunct test for clinicians to rule out tuberculosis and relieving stress for both patients and treating clinicians. However 4 ELISA negative cases, one case was of pediatrics with diagnosis of bilateral pleural effusion and protein energy malnutrition was of tuberculosis Category 1 and treated with ATT. Possible cause of ELISA negativity may be low protein levels, while 3 of orthopedics cases received ATT treatment on ground of clinical history and MRI findings and needed to be followed up for response to treatment.
Data has also shown 100% co-relation with ELISA positivity and ATT treatment, 6 ELISA positive subjects receiving ATT treatment. 28 SEVA TB ELISA subjects which were positive but were not advised ATT and need to be follow up in coming years for development of disease if any. This populace may be having latent tuberculosis infection. It has been documented that almost 5-10% of subjects with latent TB may develop in to active disease in future [6]. Thus SEVA TB ELISA can detect tuberculosis infection well in advance so that one can be monitored for development of disease and also recommended for repeated checkup in future.
Diagnosis of extra-pulmonary tuberculosis is often difficult to establish, especially in resource limited areas, and as patients attending to MGIMS, Sevagram are from rural set up. As signs and symptoms are well in advanced state and the patients insist for prompt treatment. Symptomatology of EPTB is nonspecific and microscopic examination for acid fast bacilli lacks sensitivity, and to obtain samples for histopathology, invasive procedures are more complex and costly [7]. As a result of these difficulties misdiagnosis of EPTB is common in all resource limited countries. Xang [8] reported the misdiagnosis of tuberculosis infection and increasing unnecessary burden on health system. As result of unnecessary treatment in falsely diagnosed cases, leading to more adverse condition of the patients [7]. SEVA TB ELISA can be useful investigation in hand with other clinical investigations not only in diagnosing disease but also in ruling out suspicion of presence of extra pulmonary tuberculous infection.
Acknowledgement
This study was in part supported by Kasturba Health Society core research grant for Jamanalal Bajaj Tropical Disease Research Centre (JBTDRC). Sincere thanks are due to Shri Dhiru S Mehta, President, KHS and Dr B S Garg, Dean, MGIMS for keen interest and encouragement for this study. Technical assistance of Mrs S. Ingole, Ms. M. Kalne, and Ms. Shweta is appreciated.
References
- Lalitkant. Extra-pulmonary tuberculosis: coming out of the shadows. Ind J of Tuberculosis 2004; 51: 189-190.
- SK Sharma and A.K Mohan. Extra-pulmonary tuberculosis. Indian J of Medical Research.2004; 120: 316-333.
- Majumdar A, Pranita D, Kamble CM, Badole CM, Harinath BC. Prospective study of SEVA TB peroxidase assay for cocktail antigen and antibody in the diagnosis of Tuberculosis in suspected patients attending a tertiary care hospital located in rural area. Asian Pacific Journal of Tropical Medicine 2010; 356-359.
- Gupta S, Shende N, Kumar S, Harinath BC. Detection of antibodies to a cocktail of mycobacterial excretory secretory antigens in tuberculosis by ELISA and immunoblotting. Curr Sci 2005; 88: 1825-1827.
- Waghmare P, Wankhede G, Majumdar A, Wandile K, Badole CM, Harinath BC. SEVA TB ELISA- Multi antigen and antibody assays for serodiagnosis of suspected cases of pulmonary tuberculosis and extra pulmonary tuberculosis in tertiary care hospital- A retrospective study. Asian Pacific J of Trop Diseases 2012; S827-S832.
- Centre for Disease Control and prevention. TB Elimination. The Difference Between Latent TB Infection and TB Disease. 2011.(Online available from: http:/www.cdc.gov/tb/publications/factsheets/general/LTBI and Active TB pdf )
- Steingart K, Ramsay A, Pai M. Commercial serological tests for the diagnosis of tuberculosis: do they work? Future Microbiol 2007; 2(4): 355-359.
- Xiu-Hong XI, Shui-Hua LU. Characteristics of 54 diagnosed and misdiagnosed cases of pediatric tuberculosis. Journal of Microbes and Infections.2009; 4(3): 137-139.