ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2012) Volume 23, Issue 4
Investigation of Clinical and Laboratory Findings of 26 Cases with Crimean-Congo Hemorrhagic Fever.
KANDIS Hayati1,*, KATIRCI Yavuz2, BALTACI Davut3, SARITAS Ayhan1, KARA Ismail Hamdi3, GEYIK Mehmet Faruk4
1Duzce University Faculty of Medicine Department of Emergency Medicine, Duzce, Turkey
2Yozgat State Hospital Emergency Service, Yozgat, Turkey
3Duzce University Faculty of Medicine Department of Family Medicine, Duzce, Turkey
4Duzce University Faculty of Medicine Department of Clinical Microbiology and Infectious Diseases, Duzce, Turkey
- *Corresponding Author:
- Hayati KANDIS
Duzce University Faculty of Medicine
Department of Emergency Medicine
Duzce, Turkey
Accepted Date: June 27 2012
The objective of the present study was to analyze demographic-epidemiologic features, laboratory findings and mortality rates of cases with Crimean-Congo Hemorrhagic Fever (CCHF). CCHF is an acute and severe hemorrhagic fever syndrome, caused by nairovirus transmitted by ticks, presenting with fever and hemorrhages. Twenty-six cases with CCHF admitted to the Emergency Department of Yozgat Public Hospital due to tick bites between 01.04.2007 and 30.07.2007 were enrolled in the present study. Mean age of the patients was 38.9±15.9 years. The majority of the cases was farmers and admitted to hospital mainly in April 2007. The commonest symptoms were fever, fatigue, nausea and vomiting. While thrombocytopenia and leucopenia were most commonly seen as hematological findings, AST, ALT, LDH and CPK were increased in more than half of the patients. One patient died during hospitalization. Viral disease associated with hemorrhagic changes was considered in cases of admission to the emergency department with symptoms such as hemorrhage from one or more sites of the body without any trauma, fever, lassitude, fatigue, headache and with thrombocytopenia, leucopenia or increased levels of the liver enzymes.
Keywords
Crimean-Congo hemorrhagic fever, tick bite, epidemic, hemorrhage, clinical & laboratory Investigations
Introduction
Crimean-Congo hemorrhagic fever (CCHF) is an acute and severe hemorrhagic fever syndrome, caused by nairovirus transmitted by ticks, presenting with fever and hemorrhages. CCHF is primarily a zoonosis, but sporadic and outbreaks can be observed. The disease was once called Crimean hemorrhagic fever, which was first described in Crimea in 1944. The agent of the disease seen in Congo in 1956 was discovered as the same pathogen with Crimean hemorrhagic fever, and the two names was combined as Crimean-Congo hemorrhagic fever (CCHF) [1,2].
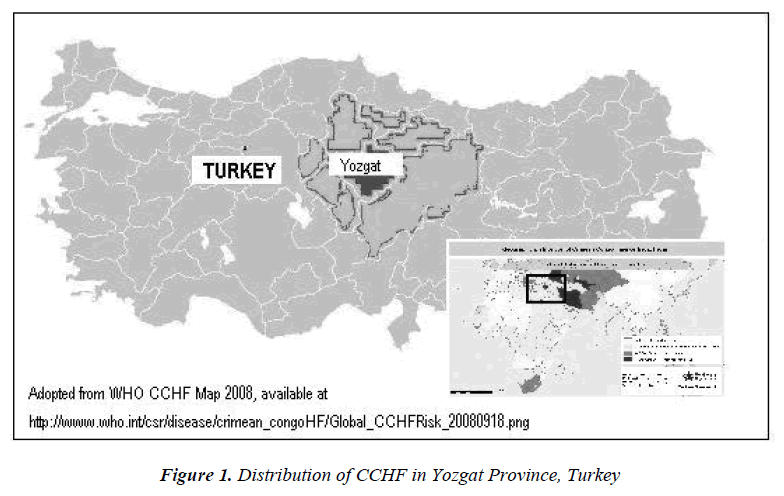
CCHF cases are frequently reported in some provinces in Turkey such as Tokat, Yozgat, Cank?r?, Corum and Sivas (Figure 1). These cities are located in the middle and near the northern part of Anatolia. These are generally steppes and mountainous and rural areas. Here, the majority of population lives in urban area. People living in these areas usually engage in agriculture and livestock. In Turkey, cases due to tick bites are reported throughout Anatolian region, and they were often severe and sometimes fatal [3].
CCHF cases attracted attention especially in the spring and the summer of 2002 and 2003 in Turkey. There were two epidemics seen in the inner Black Sea and the Eastern Anatolian region including cities such as Tokat, Yozgat, Çank?r?, Çorum, Sivas, Erzurum and Amasya [4,5].
Attending ticks can be seen everywhere especially in grasslands, stock farms, forests and bushes. CCHF has an incubation period of 1 to 3 days after tick bites but it can vary up to 9 days depending on the location of the bite. Incubation period is 5 to 6 days and up to 13 days when it is transmitted from infected body fluids and blood. CCHF caused by RNA virus, which is more severe and fatal in humans [1,6].
In this study, it was aimed to investigate the demographic, epidemiologic properties, laboratory findings and mortality rates of CCHF-infected cases at the Yozgat Central Hospital emergency clinic.
Materials and Methods
A total of 26 cases, 24 confirmed with polymerase chain reaction (PCR) positive and 2 confirmed with enzymelinked immunosorbent assay (ELISA) attending Yozgat Central Hospital Emergency Clinic after tick bite between 01.04.2007 and 30.07.2007 were included in this study.
In this cross-sectional study, age, sex, occupation, residence, times of the year, localization of the site of tick bites, clinical and laboratory (CBC and biochemical) findings were evaluated. White blood cell (WBC) < 3000/mm3 and thrombocyte (PLT) < 150.000/mm3, aspartate aminotransferase (AST) > 40 U/L, alanin aminotransferase (ALT) > 56 U/L, lactate dehydrogenase (LDH) > 243 U/L, creatine phosphokinase (CK) > 168 U/L, prothrombine time (PT) > 14 sec, partial prothrombine time (aPTT) > 35 sec were recorded as significant.
Statistical Analysis
Gathered data were evaluated by the software SPSS 11.5 (Statistical Package for Social Science). Data were presented as the mean and standard deviation. In the comparison of two independent groups and categorized variables, Student t test and Chi-Square (Fisher’s exact) test were used, respectively, and P > 0.05 was accepted as statistically non-significant (NS).
Results
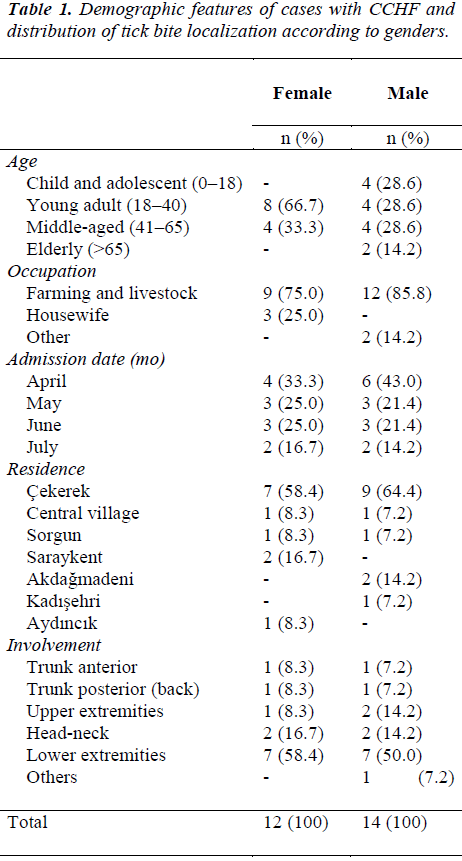
In this study, 26 cases, 14 of whom were male and the remaining 12 were female. The patients were detected CCHF-positive within the period of 4 months (between 01.04.2007 and 30.07.2007) and investigated. The average age of the patients was 38.9±15.9 years, ranging from 15 to 67 years. Males had an average age of 39.5±19.6 years and the females were 38.3±10.8 year-old. When CCHF was evaluated, most of the cases were seen in young adults 18–40 (n=12; 46.2%) whereas the least cases were seen in the geriatric age group of above 65 (n=2; 7.7%). When the cases were evaluated in terms of their occupation, the majority of the cases (n=21; 80.8%) admitted to the hospital were stock farmers and agriculturists, and most of them came in the month of April (n=10; 38.5%). Concerning the site of tick bites, lower extremities were the commonest (n=14; 53.8%), followed by the head and neck (n=4; 15.4%) (Table: 1).
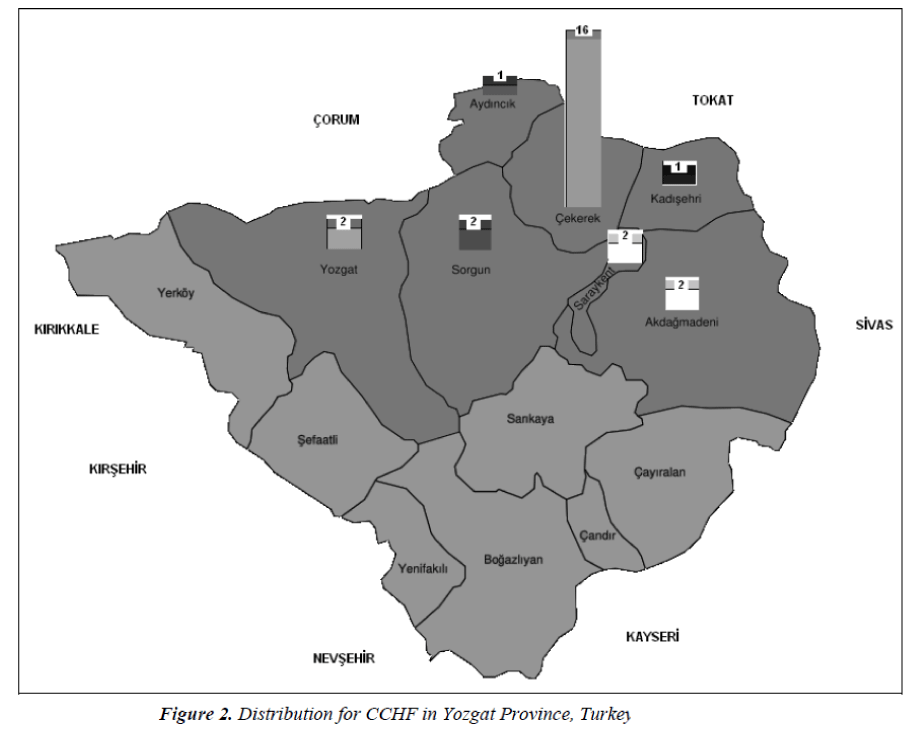
When the cases were evaluated in terms of their residential origin, there were two cases from central villages and 24 cases from town villages. Among the towns, Çekerek was ranked first with 16 cases, and Ayd?nc?k and Kad?sehri were ranked the last with one case each (Table: 1). The majority of cases were seen in north-eastern part of Yozgat (Figure: 2).
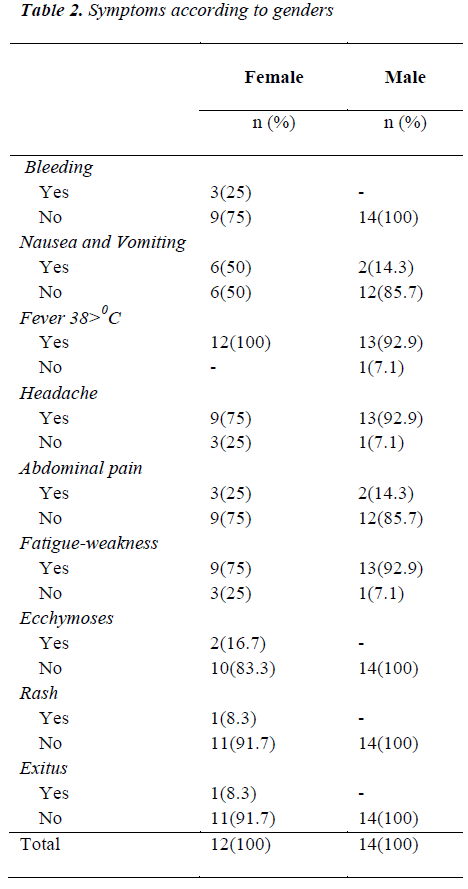
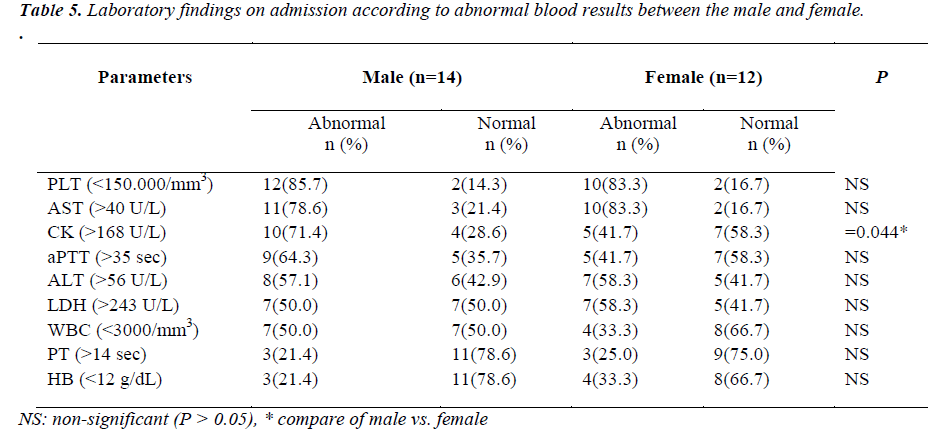
The commonest symptoms were fever (n=25; 96.2%), fatigue (n=22; 84.6%), headache (n=22; 84,6%), and nausea and vomiting (n=8; 30.7%) (Table: 2). Thrombocytopenia (n=20; 76.9%) and leucopenia (n=11; 42.3%) were the commonest laboratory findings. AST (n=21; 80.8%), ALT (n=15; 57.8%), LDH (n=15; 57.8%) and CK (n=14; 53.8%) were increased in more than half of the cases.
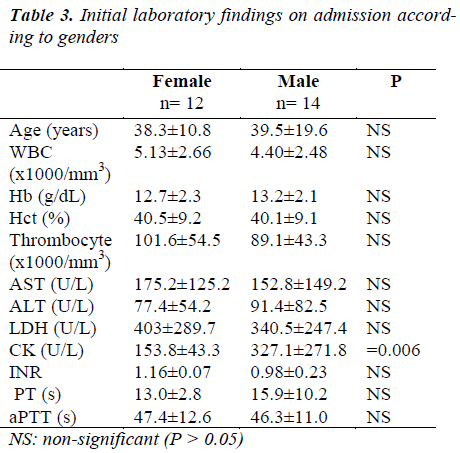
In Table: 3, the initial laboratory findings of the CCHF cases on presentation were compared in terms of their gender. Levels of thrombocyte were lower than 150.000 /mm3, and levels of AST, ALT and LDH were found to be higher than the normal for both genders. CK levels of males were significantly higher than those of females (female CK: 153.8±43.3 vs. male CK: 327.1±271.8, p=0.006).
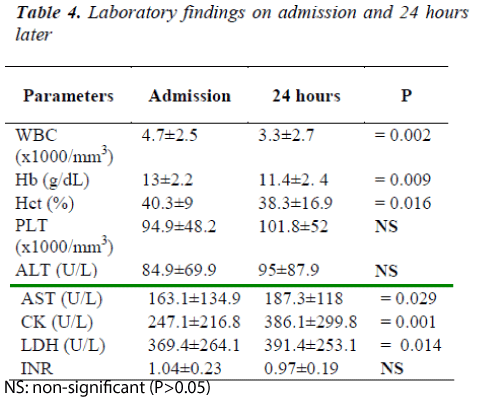
In Table: 4, laboratory findings of CCHF cases on arrival and one day after were evaluated. On arrival, it was found that the level of thrombocyte was lower than 150.000 /mm3, and levels of AST, ALT, CK and LDH were higher than the normal. Laboratory analysis showed lower WBC, hemoglobin (Hb), hematokrit (Hct) on the next day, whereas AST, LDH and CK levels were significantly higher.
Of 26 patients, 18 patients required tertiary health care, after having hospitalized into infectious disease unit from emergency room, and transferred to the health center with advanced facilities. Eight cases were discharged with relieving from service of infectious diseases unit. Eleven out of 18 referred patients were admitted in the intensive care unit of tertiary hospital. Ribavirin treatment was administered to those cases along with the support in therapy. One of 11 patients with CCHF was died due to severe gastrointestinal bleeding. The remaining cases were able to be discharged from the intensive care unit. Mortality rate was 3.8%.
Discussion
The middle, northern and eastern parts of Anatolia in Turkey, are endemic region for CCHF [7-9]. Yozgat, situated in the middle part of Anatolia, has a suitable environment for ticks spreading CCHF due to its geographic structure, climate and lifestyle of people living in this city. Many patients presenting with fever, fatigue, weakness and bleeding were admitted to the emergency rooms in those hospitals from this region. Therefore, detailed history, physical examination, some laboratory tests should be carefully evaluated and differential diagnosis for CCHF should be kept in mind, especially in the province of Yozgat.
Tick bites are especially seen in livestock farmers and agriculturists [7-11]. It is known that cases with tick bite in our country show seasonal pattern and usually occurred during the spring and the summer period [7,10,11]. In our study from April to July 2007, CCHF was diagnosed mostly in the livestock farmers and agriculturists, who were usually young adults and the adults working in open field and taking care and cleaning of animal barns. It is interesting to note that except two cases, all the infected patients were from the villages of northern and eastern parts of Yozgat which are close to the cities, such as Çorum, Tokat and Sivas. When tick bites and their consequences are investigated, most of the tick bites are recorded over the head and neck, the lower extremities and the arms [7,10,12]. In this study, tick bites were also mostly seen in the lower extremities, and the head and neck region. It is significant that tick bites are seen in the bare/exposed areas of the body in all studies.
CCHF spreads by the bite of infected ticks or through contact with infected bloods and body fluids of people and animals [1,2]. In our study, all cases were infected by the tick bite. In the literature, nosocomial transmissions were reported. In our hospital, because of universal precautions being carefully extended, we had no nosocomial transmission in any of the health care workers.
For diagnosis of the disease, isolation of the virus from blood and tissue samples, serology of the viral antigens, and antibodies against the viral antigen are used. Antibodies can be analyzed by ELISA serologically. PCR molecular biological methods are also used in diagnosis [2,5,9]. Immunoflourescent test can also be performed to confirm serology of cases. In our study, diagnostic test were performed in Refik Saydam H?fz?s?hha Research laboratories of the Department of Health of Ministry. Twenty-four of our cases were viral RNA positive with PCR, 2 of the cases were IgM positive with ELISA.
Clinical progress of CCHF changes from mild to moderate or severe. Initial symptoms differ from patients to patients. The symptoms include fever, headache, dizziness, fatigue, myalgia, nausea, vomiting and diarrhea. It can progress into shock, coma, hepatic, renal and respiratory failure in the later days [5,9,13]. Generally, recovery time of patients takes 10 days. In our study, clinically mild or moderate cases generally had fever, dizziness, nausea and vomiting. In severe cases, bleeding was seen along with fever.
Leucopenia and thrombocytopenia can be observed as laboratory findings. Biochemical analysis showed elevated levels of ALT, AST, GTT, CK and LDH. Bleeding time, PT and PTT are prolonged [3,5,7,9,14]. In our study, leucopenia and thrombocytopenia were the commonest hematological findings. More than half of the cases had elevated levels of ALT, AST, LDH, CK but there was no significant increase in PT, aPTT, INR measurements as seen on arrival. CK elevation in male patients was higher than that in the female patients. It might be due to more muscle body mass in males. On comparison, laboratory findings of the cases with CCHF on arrival and the day after, WBC, Hb and Hct levels decreased while AST, LDH and CK levels increased. Therefore, serial laboratory investigations can be used to monitor patients’ condition.
In case of non-traumatic, chronic bleedings in single or multiple parts of the body together with complaint of fever, weakness, fatigue, with laboratory findings of leucopenia, thrombocytopenia, elevated liver enzymes, and an altered clotting tests on arrival to emergency room; one should take viral hemorrhagic diseases into consideration. A good anamnesis is usually helpful for differentiating bleeding disorder, such as congenital bleeding disorders, medication overdose or hepatic failure [15]. A detailed physical examination and laboratory analysis must be performed as well. In our study, being endemic in this region, tick-bitten people with one or more abnormal laboratory findings such as thrombocytopenia, leucopenia, elevated liver enzymes, increased in bleeding time, a detailed anamnesis and physical examination were performed for CCHF suspicion were sent to Refik Saydam H?fz?s?hha Central Research Laboratories for confirmation of the diagnosis.
Intensive care is needed for severe CCHF patients. Airway, breathing, and circulation should be controlled in CCHF patients. Calorie support should be given and blood products should be given when needed. CCHF patients should be closely monitored and if needed they should be supported by mechanical ventilation and dialysis in ICU [7,16,17]. There is no specific treatment but an antiviral agent ribavirin can be used orally or parenterally [7,14,17]. However, it is only currently the oral form available in our country. Although it is claimed that ribavirin decreases mortality especially in severe cases of CCHF, it has been reported that ribavirin increased mortality instead of decrease in mortality [3,9,7,18,19]. We initiated supportive treatment to confirm cases. Eighteen cases, not responding to supportive treatment and probably requiring intensive care, were referred to another health center with advanced facilities. Eleven patients of them needed to be admitted into intensive care unit. Ribavirin was administered to them along with supportive treatment. Based on WHO guidelines, patients should be treated for 10 days (30 mg/kg as an initial loading dose, then 15 mg/kg every 6 hours for 4 days, and then 7.5 mg/kg every 8 hours for 6 days) [14,20]. Ribavirin was given to patients with vomiting or unable to tolerate oral intake by way of nasogastric tube. It was reported that hemolytic anemia, hypocalcaemia, and hypomagnesaemia might be seen in patients receiving ribavirin to treat severe acute respiratory syndrome [21,22]. However, no adverse events due to ribavirin therapy were noted among the CCHF patients healed in Turkey [14].
Ten patients monitored in intensive care were discharged, but one patient died from massive gastrointestinal bleeding (hematemesis and melena). All others were also discharged. Mortality ranged between 0 and 80 % in different series. In the study conducted by Papa et al. [23] with eight cases, all of the cases showed full recovery. Mortality rate was 25% in another study with eight cases conducted by Van Eeden et al. [17], and mortality rate was 30% in the study with 50 cases conducted by Swaneopel et al. [24]. Mortality rate was 25% in another study from Turkey with four cases conducted by Öztürk et al. [25]. In our study, there were 26 cases only one died and the mortality rate was 3.8%. The low mortality rate in our study may be related to early diagnosis. Because CCHF cases are common in our country since 2002, and facilities for intensive care have improved to substantial extent. Early diagnosis and the treatment with intensive care might decrease mortality due to CCHF.
Conclusion
In conclusion, we emphasize that the differential diagnosis should also include viral diseases for non-specific symptoms such as dizziness, fatigue, bleeding, fever, and headache and abnormal laboratory findings such as thrombocytopenia, leucopenia and elevated liver enzymes. CCHF should be kept in mind among the viral diseases. A detailed anamnesis and physical examination should be performed in all cases. Clinically suspicious cases should be hospitalized, observed and after differential diagnosis early treatment should be initiated as soon as the diagnosis is confirmed.
References
- Gedik H. Crimean-Congo Hemorrhagic Fever Virus, Ticks and Base Measures. Nobel Med 2009;5: 10–14
- Whitehouse CA. Crimean–Congo hemorrhagic fever. Antiviral Res 2004; 64:145–160.
- Ergönül E, Çelikbas A, Dokuzo?uz B, et al. Characteristics of patients with Crimean-Congo hemorrhagic fever in a recent outbreak in Turkey and impact of oral ribavirin therapy. Clin Infect Dis 2004; 39: 284-287.
- Gozalan A, Akin L, Rolain JM, et al. Epidemiological evaluation of a possible outbreak in and nearby Tokat province. Mikrobiol Bull 2004; 38: 33-44.
- Karti SS, Odabasi Z, Korten V, et al. Crimean-Congo hemorrhagic fever in Turkey. Emerg Infect Dis 2004; 10: 1379-1384.
- Capua I. Crimean-Congo haemorrhagic fever in ostriches: a public health risk for countries of the European Union? Avian Pathol 1998; 27:117-120.
- Ozkurt Z, Kiki I, Erol S, et al. Crimean–Congo hemorrhagic fever in Eastern Turkey: clinical features, risk factors and efficacy of ribavirin therapy. J Infect 2006; 52:207–215.
- Bakir M, Ugurlu M, Dokuzoguz B, et al. Group Crimean- Congo haemorrhagic fever outbreak in Middle Anatolia: a multicentre study of clinical features and outcome measures. J Med Microbiol 2005; 54:385-389.
- Koksal I, Yilmaz G, Aksoy F, et al. The efficacy of ribavirin in the treatment of Crimean-Congo hemorrhagic fever in Eastern Black Sea region in Turkey. J Clin Virol. 2010;47:65–68.
- Al B, Y?ld?r?m C, Sö?üt Ö, et al. Batman Devlet Hastanesi Acil Servisine yedi ayda basvuran 39 kene ?s?r???n?n de?erlendirilmesi. Akad Acil T?p Derg 2008; 7:40-43.
- Kandis H, Kat?rc? Y, Uzun H, et al. Demographic and Epidemiologic Features of Tick Bite Cases Who Have Applied to Emergency Service in an Endemic Region. Duzce Medical Journal 2010; 12:18–23.
- Taskesen M, Okur N, Tas MA. Kene Is?rmas? Nedeniyle Basvuran 19 Olgunun De?erlendirilmesi. Dicle T?p Dergisi 2008; 35:110-113.
- Anagnostou V, Papa A. Evolution of Crimean-Congo Hemorrhagic Fever virus. Infect Genet Evol 2009; 9:948–954.
- Ergönül O. Crimean-Congo hemorrhagic fever. Lancet Infect Dis 2006; 6:203–214.
- Hemphill RR. Evaluation of anemia and the bleeding patient. In: Tintinalli JE, Kelen GD, Stapczynski JS, editors. Emergency medicine. A comprehensive study guide. New-York: McGraw-Hill; 2004. p. 1319-24.
- Borio L, Inglesby T, Peters CJ, et al. Hemorrhagic fever viruses as biological weapons: medical and public health management. JAMA 2002; 287:2391-2405.
- Uzun R, U?urlu M. K?r?m-kongo kanamal? atesinde ribavirin kullan?m?. Klimik Derg 2004; 17:62-64.
- Tasyaran MA, Özkurt Z. K?r?m-Kongo Hemorojik atesi: Tedavi ve Korunma. Klimik Derg 2004; 17:157-160.
- Mardani M, Jahromi MK, Naieni KH, et al. The efficacy of oral ribavirin treatment of Crimean–Congo hemorrhagic fever in Iran. Clin Infect Dis 2003; 36:: 1613–1618.
- WHO. Crimean - Congo haemorrhagic fever. http://www.who.int/mediacentre/factsheets/fs208/en/ (accessed March 12, 2009).
- Knowles SR, Phillips EJ, Dresser L, et al. Common adverse events associated with the use of ribavirin for severe acute respiratory syndrome in Canada. Clin Infect Dis 2003; 37:1139–1142.
- Chiou HE, Liu CL, Buttrey MJ, et al. Adverse effects of ribavirin and outcome in severe acute respiratory syndrome: experience in two medical centers. Chest 2005; 128: 263–272
- Papa A, Bozovic B, Pavlidou V, et al. Genetic detection and isolation of Crimean-Congo haemorrhagic fever virus, Kosova, Yugoslavia. Emerg Infect Dis 2002; 8:852-854.
- Swanepoel R, Gill DE, Shepherd AJ, et al. The clinical pathology of Crimean-Congo hemorrhagic fever. Rev Infect Dis 1989; 11: 794-800.
- Öztürk DB, Sencan I, Gürbüz Y, et al. People To People Transmission of CCHF among Society: Four Cases. Konuralp T?p Dergisi 2012; 4: 28–31.