ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2012) Volume 23, Issue 1
Ischemia modified albumin in patients of cardiac and non-cardiac chest pain
1Department of Biochemistry, Kalinga Institute of Medical Sciences, Bhubaneswar, Orissa, India.
2Department of Biochemistry, Pt. B.D.Sharma PGIMS, Rohtak, Haryana, India.
3Department of Biochemistry, Pt. B.D.Sharma PGIMS, Rohtak, Haryana, India.
4Department of Medicine, Pt. B.D.Sharma PGIMS, Rohtak, Haryana, India.
5Department of Anaesthesiology, Kalinga Institute of Medical Sciences, Bhubaneswar, Orissa, India.
Accepted date: May 11 2011
Existing biochemical markers are not suitable for assessing early myocardial ischemia particularly in first 2-6 hours of ischemia i.e. before setting in of irreparable myocardial damage. Recently ischemia modified albumin (IMA) has emerged as the earliest cardiac marker. Therefore, this study was planned to estimate IMA levels in patients of acute chest pain with or without cardiac cause. One hundred patients of acute chest pain (50 patients with cardiac cause and 50 patients with non-cardiac cause) were selected for the study and compared with 50 age and sex matched healthy controls. IMA, creatine kinase- MB (CK-MB), Troponin I, routine biochemical investigations, hemoglobin and total leucocyte count were estimated in these patients. The results were analysed statistically. IMA levels were found to be significantly elevated in patients of chest pain with myocardial ischemia as compared to the other two groups. A significant positive correlation was found between IMA levels & CKMB levels (r = +0.713, p value<0.001) and IMA levels & troponin I levels (r = +0.823, p value<0.001) but a poor correlation was observed between IMA levels and SGOT levels (r = - .012, p value>0.05). Thus we conclude that IMA assay is a sensitive but not very specific marker for early detection of myocardial ischemia. IMA can be combined with other biochemical markers like CK-MB and Troponin I to increase the specificity. Other non myocardial ischemic conditions should be kept in mind while interpreting IMA values.
Key words
Ischemia modified albumin, CK-MB, Troponin I, Myocardial ischemia, Non-cardiac chest pain.
Introduction
Heart disease is the leading cause of death in the world. Incidence of ischemic heart disease is rising alarmingly due to rapid urbanization, sedentary life style, altered food habits and increasingly stressful life. Evaluation of patients presenting with chest pain in the emergency department is difficult and challenging [1,2]. Though there are clinical, biochemical and other laboratory tests which help in diagnosis but there is no rapid and definitive test which can be termed as gold standard to rule out myocardial ischemia. Only about 22% of the patients admitted to cardiac care centres with acute chest pain actually develop acute myocardial infarction [1].
HSA (Human Serum Albumin) is the most abundant multifunctional protein in blood, with a mean concentration of 0.63 mmol/L (40g/L) consisting of 585 amino acid residues (66.5 kDa) folded into three homologous domains as determined by X-ray crystallography, synthesized in the liver, and having a half-life of 19 days [3]. Extensive studies of the metal binding properties of HSA have revealed that metal ions bind to a wide variety of sites [4]. The best characterized metal binding site is located at the N-terminus, which is comprised of amino acid sequence N-Asp-Ala-His-Lys [5]. Out of these four residues first three have been shown to be essential for metal ion binding while the fourth one (lysine) is not essential [6]. These sites have particular high affinity for copper and nickel. The groups that participate in this binding have been shown to be the α-amino group, the two intervening peptide nitrogen atoms, the δ-imidazole nitrogen from His3 and the side-chain carboxyl group of Asp1[4]. Recently, a biochemical test has been reported based on the binding between the serum albumin and the transition metal cobalt. This is known as the albumin co balt binding (ACB) test which is based on the observations that the binding of cobalt to albumin is reduced in serum in patients of myocardial infarction (MI). Albumin in which N-terminus is either damaged or occupied by copper is termed as ischemia modified albumin (IMA) and the test is referred to as ACB test [7-9]. Conditions necessary for altering the metal binding site of HSA are known to occur in vivo and probably occur within minutes after the onset of myocardial ischemia [10-12].
So it can act as the earliest marker for MI. Therefore this study was planned to estimate IMA in patients of acute chest pain with or without cardiac cause.
Material and Methods
After obtaining informed consent from the patients and approval from the institutional board of studies, the present study was conducted on 100 patients of acute chest pain (age group 30-60 years) visiting the Emergency Department of Pt.B.D.Sharma PGIMS, Rohtak within 6 hours of chest pain and 50 healthy controls. These patients were divided into three groups based on electrocardiography (ECG) changes and clinical signs and symptoms.
Group І: (n=50) with myocardial ischemia.
Group ІІ: (n=50) without ischemia.e.g. Musculoskeletal pain, reflux esophagitis etc.
Group ІІІ: (n=50) age and sex matched healthy controls.
Patients having renal disease, liver disease, pregnancy, brain ischemia and trauma were excluded from the study. Serum samples were analysed for IMA, CK-MB, Troponin I (Tn I) immediately and routine biochemical investigations, hemoglobin and total leucocyte count were done on fasting samples on the same day. IMA was estimated by colorimetric method [7], Tn I by Chemiluminometer (Advia Centuer) , CK-MB on semiautoanalyser (Techno 168) by immunoinhibition assay using kits by Siemens and other biochemical investigations were done on autoanalyser (Konelab 30i, Thermo Electron Corporation) using kits by Siemens and Randox. The results were statistically analysed using software SPSS version 16.0 applying unpaired student’s t test & Pearson’s correlation method.
Results
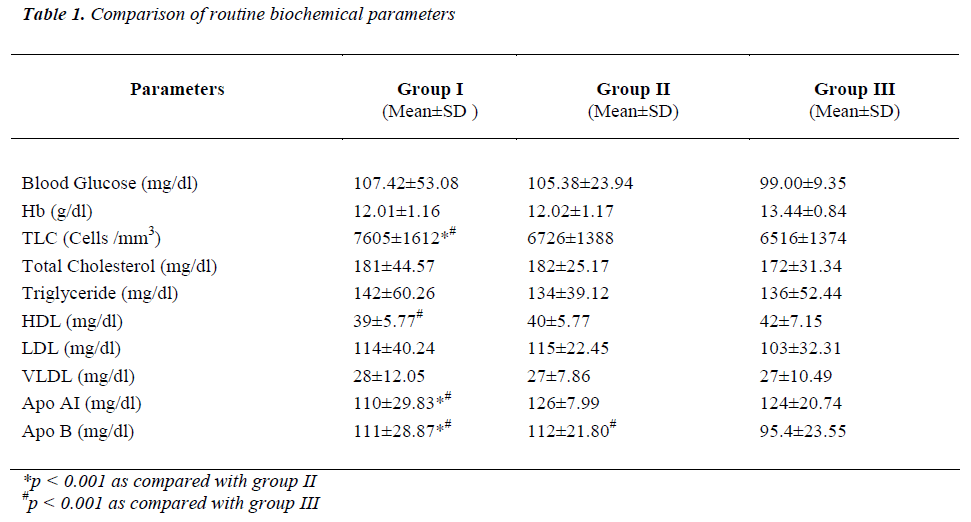
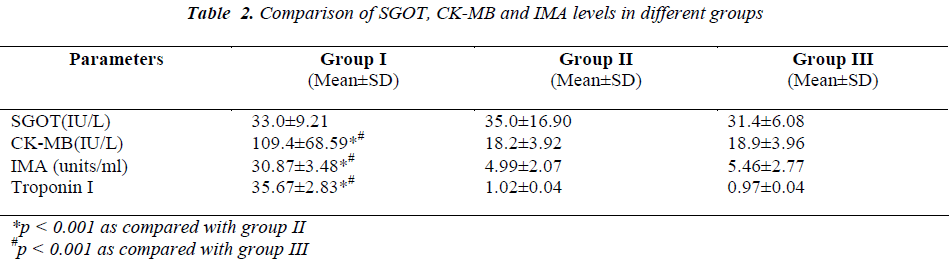
The results of routine biochemical investigations are shown in table1. The levels of different cardiac markers are shown in table 2. A significant positive correlation was observed between IMA levels and CK-MB levels (r = +0.713, p value<0.001) IMA levels and Tn I levels (r = +0.823, p value<0.001) and but there is poor correlation between IMA levels and AST levels (r = -0.012, p value>0.05).
Discussion
Myocardial ischemia results from lack of adequate blood perfusion to the myocytes leading to deficiency of oxygen and nutrients, eventually compromising their vital functions. In a clinical setting, myocardial ischemia is diagnosed by clinical presentation and ECG. In addition to symptomatic and ECG diagnosis, biochemical markers play an integral part in the diagnosis and therapeutic management of these patients. An ideal myocardial ischemia marker should be highly sensitive, highly specific and it should be detected at earliest (i.e. preferably before irreversible damage occurs). Further, the marker should be able to influence therapy, improving patient’s outcome.
Currently, there is no well defined biochemical marker for the identification of myocardial ischemia before irreparable myocardial damage sets in. Biochemical markers such as CK-MB, TnI and myoglobin, used for detection of myocardial infarction, are not suitable for assessing early myocardial ischemia particularly in first 2-6 hours of ischemia because these intracellular markers are released into the circulation only after complete damage to the myocardium has already occurred.
There are various potential markers for early detection of myocardial ischemia like IMA, heart fatty acid binding protein, choline etc. Among these, IMA has been found be very sensitive (sensitivity 85-95%) and it has a high negative predictive value (75-95%). The specificity of the test ranges from 31% to more than 95% in different studies. Our study also shows that IMA is a sensitive and specific marker for diagnosis of chest pain due to myocardial ischemia. Chawla et al found IMA assay to be more sensitive and specific (with sensitivity 78.0% and specificity 82.7%) than CK-MB assay (with a sensitivity of 58% and specificity of 60.0%) for detection of myocardial ischemia [13].
We know from previous studies that IMA levels rise much earlier than CK-MB levels. In the present study IMA levels were not elevated in group of patients with chest pain of non-cardiac origin and in healthy volunteers. However many studies have demonstrated that IMA levels can be elevated in conditions other than myocardial ischemia like pregnancy, stroke, chronic renal disease, exercise-induced calf ischemia, marathon runners due to exercise-induced latent gastrointestinal ischemia [14-20]. IMA also increases after skeletal muscle ischemia during arthroscopic knee surgery [21].
The basis of the IMA assay is that, serum albumin of individuals with myocardial ischemia exhibits reduced binding to Co2+ compared with serum albumin of nonischemic individuals [9]. It is well known that within minutes of onset of myocardial ischemia, there is hypoxia, free radical damage and acidosis followed by disruption of membrane sodium / calcium ion pumps. This, in turn, causes alteration in the NH2 terminus of albumin which has a high affinity for transition metals like Cu2+ and Ni2+. This leads to reduced binding capacity of cobalt ions to albumin. Studies have indicated that mechanisms involved in ischemia/ reperfusion are induced changes in albumin and may include exposure to endothelial and extracellular hypoxia, acidosis, free radical damage, ATP dependant sodium and calcium pump disruption resulting in exposure to free iron and copper ions [10-12].
In the present study, IMA levels were found to be significantly elevated in patients of chest pain with myocardial ischemia as compared to other two groups. A significant positive correlation was observed between IMA levels and CK-MB levels (r = +0.713, p value<0.001) IMA levels and Tn I levels (r = +0.823, p value<0.001) and but there is poor correlation between IMA levels and AST levels (r = -0.012, p value>0.05).
TLC levels were higher in the study group as compared to the other two control groups. Recent studies have reported that TLC is associated with cardiovascular risk. Leukocytes contribute to blood viscosity, release products that induce plaque rupture and thrombus formation [22-24]. In our study, lipid profile parameters viz. total cholesterol, triglyceride, LDL, VLDL were estimated but there was no statistically significant difference in any of the above parameters among the three groups. HDL-C levels were found to be lower in group I as compared to the other two groups. The difference was statistically significant as compared to group III. This decrease in HDL-C in group I could be due to the fact that low levels of HDL-C are associated with an increased risk of ischemic heart disease. ApoA-1 levels were decreased significantly in ischemic group as compared to the other two groups which may be due to association of decreased ApoA-1 with an increased risk of coronary heart disease by participating in the reverse cholesterol transport [25]. ApoB levels were similarly found to be significantly elevated in ischemic group as compared to other two groups. Increased levels of ApoB are associated with an increased risk of ischemic heart disease [25].
Thus, we conclude that IMA assay is a sensitive but not very specific marker for early detection of myocardial ischemia. There is a good correlation of IMA assay with other cardiac markers, so IMA can be combined with these biochemical markers to increase specificity. Other non-myocardial ischemic conditions should be kept in mind while interpreting IMA values.
Acknowledgements
The contribution of technical staff of Biochemistry Department of Pt. B.D. Sharma PGIMS, Rohtak is duly acknowledged.
References
- Graff LG, Dallara J, Ross MA. Impact on the care of the emergency department chest pain patient from the Chest Pain Evaluation Registry (CHEPER) Study. Am J Cardiology 1997; 80: 563-569.
- Storrow AB, Gibler WB. Chest pain centres: Diagnosis of acute coronary syndromes. Ann Emerg Med 2000; 35: 449-461.
- He XM, Carter DC. Atomic structure and chemistry of human serum albumin. Nature 1992; 358: 209-215.
- Predki PF, Harford C, Brar P, Sarkar B. Further characterization of the N- terminal copper (II) and nickel (II) binding motif of proteins. Studies of metal binding to chicken serum albumin and the native sequence peptide. Biochem J 1992; 287: 211-215.
- Laussac JP, Sarkar B. Characterization of the copper (II) and nickel (II) transport site of human serum albumin. Studies copper (II) and nickel (II) binding to peptide 1-24 of human serum albumin by 13C and 1H NMR spectroscopy. Biochemistry 1984; 23: 2832-2838.
- David Bar-or, Curtis DC, Rao N, et al. Characterisation of CO2+ and Ni2+ binding amino acid residue of the Nterminus of human albumin. Eur J Biochem 2001; 268: 42-47.
- Bar-Or D, Lau E, Rao N, et al. Reduction in the cobalt binding capacity of human serum albumin with myocardial ischemia. Ann Emerg Med 1999; 34:S56.
- Bar-Or D, Lau E, Winkler JV. A novel assay for cobalt albumin binding and its potential as a marker for myocardial ischemia - a preliminary report. J Emerg Med 2000; 19: 311-315.
- Bhagavan NV, Lai EM, Rios PA, et al. Evaluation of human serum albumin cobalt binding assay for the assessment of myocardial ischemia and myocardial infarction. Clin Chem 2003; 49: 581-585.
- Cobbe SM, Poole-Wilson PA. The time of onset and severity of acidosis in myocardial ischemia. J Mol Cell Biol 1980; 12: 745-760.
- Bernstein E, Mayer B, Goldberg C, et al. Patterns of mobilization of copper and iron following myocardial ischemia: possible predictive criteria for tissue injury. J Mol Cell Cardiol 1997; 29: 3025-3034.
- McCord JM. Oxygen derived free radicals in post ischemic tissue injury. N Engl J Med 1985; 312: 159- 163.
- Chawla R, Goyal N, Calton R, et al. Ischemia modified albumin: A novel marker for acute coronary syndrome. Indian J Clin Biochem 2006; 21: 77-82.
- Van Rijn BB, Franx A, Sikkema JM, et al. Ischemia modified albumin in normal pregnancy and preeclampsia. Hypertens Pregnancy 2008; 27: 159-167.
- Gunduz A, Turedi S, Mentese A, et al. Ischemia- modified albumin levels in cerebrovascular accidents. Am J Emerg Med 2008; 26: 874-878.
- Abboud H, Labreuche J, Meseguer E, et al. Ischemia modified albumin in acute stroke. Cerebrovasc Dis 2007; 23: 216-220.
- Cichota LC, Moresco RN, Duarte MM, et al. Evaluation of ischemia-modified albumin in anemia associated to chronic kidney disease. J Clin Lab Anal 2008; 22: 1-5.
- Falkensammer J, Stojakovic T, Huber K, et al. Serum levels of ischemia-modified albumin in healthy volunteers after exercise-induced calf-muscle ischemia. Clin Chem Lab Med 2007; 45: 535-540.
- Zapico-Muniz E, Santalo-Bel M, Muntanola M J, et al. Ischemia-modified albumin during skeletal muscle ischemia. Clin Chem 2004; 50: 1063–1065.
- Apple FS, Quist HE, Otto AP, et al. Release characteristics of cardiac biomarkers and ischemia modified albumin as measured by the albumin cobalt- binding test after a marathon race. Clin Chem 2002; 48: 1097–1100.
- Majed AR, Curtis AP, Rick WW, et al. Ischemia modified albumin increases after skeletal muscle ischemia during arthroscopic knee surgery. Clin Chim Acta 2006; 366: 264-268.
- Weijenberg MP, Feskens EJ, Kromhout D. White blood cell count and the risk of coronary heart disease and all cause mortality in elderly men. Arterioscler Thromb Vasc Biol 1996; 16: 499-503.
- Ernst E, Hammerschmidt DE, Bagge U, et al. Leukocytes and the risk of ischemic diseases. J Am Med Assoc 1987; 257: 2318-2324.
- Gokulakrishnan K, Deepa R, Sampathkumar R, et al. Association of leukocyte count and hs CRP with metabolic abnormalities in subjects with normal glucose tolerance. J Assoc Phy India 2009; 57: 27-32.
- Benderly M, Bokyo V, Goldbourt U. Apolipoproteins and long- term prognosis in coronary heart disease patients. Am Heart J 2009; 157: 103-110.