ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2009) Volume 20, Issue 3
Menopausal Syndrome: Effect on Serum Lipid and Lipoprotein Profiles
Ebele J* Ikekpeazu, Emeka E. Neboh1, Ignatius C. Maduka2, Fidelis E. Ejezie, Silas Ufelle3
Department of Medical Biochemistry
1Department of Chemical Pathology, College of Medicine, Enugu State University Teaching Hospital (ESUTH), Enugu State Nigeria,
2Department of Chemical Pathology, University of Nigeria Teaching Hospital (UNTH), PMB. 01129, Ituku-Ozalla, Enugu State, Nigeria
3Department of Medical Laboratory Sciences, College of Medicine, University of Nigeria Enugu Campus (UNEC), Enugu State, Nigeria,
- *Corresponding Author:
- Ebele J. Ikekpeazu
Department of Medical Biochemistry
College of Medicine, University of Nigeria
Enugu Campus, UNEC
Enugu State, Nigeria.
E-mail: iebelejoy@yahoo.com
Accepted date: April 04 2009
Plasma lipids have been known to be altered by the within-month variations in the female hormonal system. The female hormonal system also controls the menstrual cycle in the pre-menopausal women. This study is, therefore, aimed at finding the possible effects of menopause on plasma lipids and lipoproteins, as shown by the lipid profile. The lipid profiles of 200 post-menopausal women and 100 pre-menopausal control women were estimated. The results obtained show a statistically significant increase (P less than 0.05) in the total cholesterol level of early menopausal subjects (6.05 plus/minus 1.03mmol/L) and slightly higher values in late menopausal subjects (6.80 plus/minus 0.81mmol/L), when compared with the control subjects (4.6 plus/minus 0.62mmol/L). Triglycerides (TG) showed slight but significant increase (P less than 0.05) in the early menopausal subjects (1.40 plus/minus 0.80 mmol/L) and higher levels in late menopausal subjects(1.96 plus/minus 0.45 mmol/L) in comparison with the control subjects (1.02 plus/minus 0.44 mmol/L). High density lipoprotein (HDL) levels were however reduced significantly (P less than 0.05) in early menopausal subjects (1.20 plus/minus 0.27 mmol/L) and even lower in late menopausal subjects (1.17 plus/minus 0.28 mmol/L) when compared to the controls; while Low density lipoprotein (LDL) and very low density lipoprotein (VLDL) levels were significantly increased (P less than 0.05) in early menopausal subjects (4.21 plus/minus 0.81 and 0.63 plus/minus 0.37 mmol/L), and higher in late menopausal subjects (4.70 plus/minus 0.55 and 0.81 plus/minus 0.41 mmol/L) when compared with the control subjects. The findings suggest the probability that menopausal syndrome can lead to hyperlipidaemia, dyslipidaemia and possibly predispose women to coronary artery disease.
Keywords
Effect, menopausal syndrome, serum, lipid, lipoprotein, profile
Introduction
A lipid profile is a battery of tests used in diagnosing, treating and predicting atherosclerosis. It consists of four tests and some calculated values. The measured tests are total cholesterol (TC), triglycerides (TG) and high density lipoprotein (HDL), while the calculated values are low density lipoprotein (LDL), very low density lipoprotein (VLDL) and a cardiac risk factor [1].
Coronary artery disease (CAD) results from the thickening of the inner layer of arterial walls and accounts for more than 50% of all deaths. It is the number one cause of death of women. Part of the body’s cholesterol is derived from dietary intake, but majority is synthesized by the liver and other tissues [2]. Lipids have important roles in virtually all aspects of biological life – serving as hormone precursors, aiding digestion, providing energy storage and metabolic fuels, acting as functional and structural components in bio-membranes and forming insulation to allow nerve conduction or to prevent heat loss [3]. Menopause results from the loss of ovarian function, either naturally or surgically.
The female hormonal cycle is an exquisitely controlled system that includes the hypothalamus, pituitary, adrenal, thyroid and gonadal tissues; involving both positive and negative feed back loops [4]. At birth, every woman is endowed with one to two million primodial follicles which decrease to about 300,000 by the time of menarche (puberty) [5]. By age 51, the median age for the final menstrual period, the ovary reserve is about 1000 and this corresponds with a significant drop in estrogen production, typical when symptoms of menopause occur [4]. It is significant to note that while a woman may stop menstruating at this time, endogenous cycling and ovulation may still occur for months, even years [5]. About 20% of estrogenemic effects on arteries are mediated through changes in lipids and lipoproteins [6]. The association between hypercholesterolemia and atherosclerotic heart disease is an established fact and thrombosis produce occlusive vascular lesions in humans, which may lead to such adverse clinical conditions as stroke, myocardial infarction or peripheral vascular disease [7]. While similar mechanisms operate to induce cardiovascular disease in women and men, genderrelated differences exist in the anatomy and physiology of the myocardium, and sex hormones modify the course of the disease in women [8].
The hypo-estrogenic status that results from menopause leads to ovarian failure, resulting in a significant increase in total cholesterol and LDL-cholesterol, predisposing such women to the risk of coronary artery disease [9].
Material and Method
Subjects
The subjects in this study were 200 apparently healthy volunteers of post-menopausal age status (aged between 50 and 69 years), drawn from Enugu metropolis. A total of 100 apparently healthy pre-menopausal women (aged between 35 and 49 years) served as control subjects for the study. Informed consent was duly obtained from each subject that participated in the study.
Exclusion criteria
Subjects with a history of, or who were suffering from conditions which predisposes one to abnormal lipid profile, such as diabetes mellitus, hypercholesterolaemia and hyperlipidaemia, were excluded from the study.
Sample collection and preparation
Fasting whole blood samples {3.0 ml each} were collected from subjects while in the sitting position, by clean venepuncture from the antecubital vein. The samples were collected under asceptic conditions while avoiding haemolysis and dispensed into sterile plain tubes and allowed to clot. The clotted samples were centrifuged at 3000 rpm for five minutes and the separated clear serum supernatants were transferred into sterile tubes. These freshly drawn serum supernatants were used for total cholesterol, triglycerides and HDL-cholesterol assays. The sera were stored frozen and the analysis was carried out within one week.
Analytical method
Total cholesterol (TC) assay was done by enzymaticspectrophotometric method [10]; while HDL-cholesterol (HDL-C) estimation was carried out using precipitation/ enzymatic-spectrophotometric method [11]. Enzymatic spectrophotometric method [12] was used for triglyceride (TG) estimation; while LDL and VLDL were calculated using Friedewald’s formula [13].
Statistical method
The statistical analysis (students T-test) were done using graph pad prism computer software package. Results are reported as mean plus/minus standard deviation (mean plus/minus SD).
Result
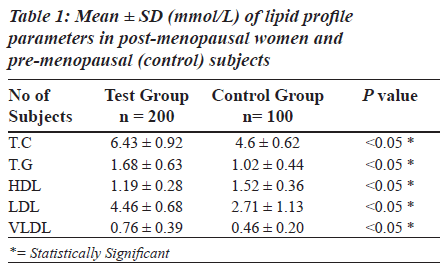
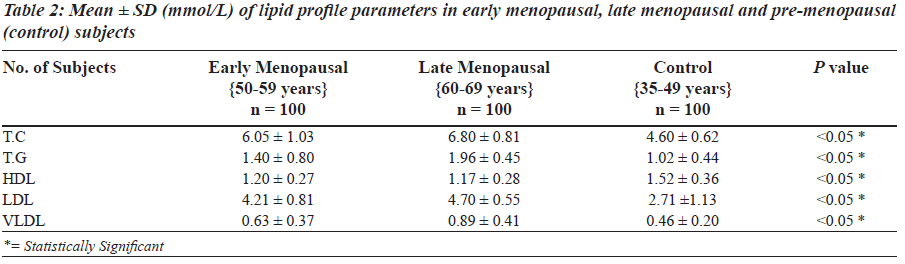
The results are presented as mean plus/minus standard deviation (mean plus/minus SD). Table 1 shows a statistically significant difference (P less than 0.05) in the levels of the lipid profile parameters in the test and control subjects. There was a marked increase in the mean levels of TC, TG, LDL, VLDL and lower than normal HDL concentration for postmenopausal women 6.43 plus/minus 0.92; 1.68 plus/ minus 0.63; 4.46 plus/minus 0.68; 0.76 ± 0.39 and 1.19 plus/minus 0.28 mmol/L when compared to the controls (4.60 plus/minus 0.62; 1.02 plus/minus 0.44; 2.71 plus/ minus 1.13; 0.46 plus/minus 0.20 and 1.52 plus/minus 0.36 mmol/L, respectively). When late post-menopausal subjects (60-69 years) were compared with early post-menopausal subjects (50-59 years), there was a statistically significant difference (P less than 0.05) in the mean levels of the various parameters [Table 2].
TC, TG, LDL,VLDL and HDL for the late postmenopausal subjects were 6.80 plus/minus 0.81; 1.96 plus/minus 0.45;4.70 plus/minus 0.55; 0.89 plus/minus 0.41 and 1.17 plus/minus 0.28 mmol/L respectively, while that of the early menopausal subjects were 6.05 plus/minus 1.03; 1.40 plus/ minus 0.80; 4.21 plus/minus 0.81; 0.63 plus/minus 0.37 and 1.20 plus/minus 0.27 mmol/L in the same order.
Discussion
The study is focused on the effect of age, early and late menopause on the lipid profile of postmenopausal women. The results obtained in the two age groups pf postmenopausal women show elevated TC, TG, LDL, VLDL and reduced HDL level (P less than 0.05), which could be attributed to gradual cessation in the synthesis of reproductive hormones due to the transition into menopause. This consequently leads to the accumulation of cholesterol in the blood. This finding agrees with an earlier study by [1].
Although the two groups of post-menopausal women showed elevated levels of lipids and lipoproteins, there was significantly higher levels among the late menopausal women (P less than 0.05), which might be linked to a total loss of estrogen production. This finding supports the work of [5], which stated that while a woman may stop menstruating at the onset of menopause, endogenous cycling may still occur for months or even years (as seen in the early menopausal age). The control subjects however showed a normal pattern of lipid profile which can be attributed to the continual metabolism of cholesterol, via the synthesis of hormones such as estrogens, which regulate the female menstrual cycle.
The study shows an association between early and late menopause and lipid profile of post-menopausal women; and also provides an explanation for the higher prevalence of hyperlipidemia and increased risk of atherosclerosis as observed in the late menopausal women.
Conclusion
The study shows that there is a probability that concentration of the lipid profile parameters in post-menopausal subjects might depend on menopausal age.
It also reveals possible predisposition to unfavorable lipid profile and risk of coronary heart disease with progress from early to late menopausal age. It is therefore recommended that post-menopausal women should always be screened for hyperlipidaemia to reduce the prevalence of coronary artery disease (CAD).
References
- Brites FD, Bonavita CD, Cloes M. Yael M. VLDL compositional changes and plasma levels of triglycerides and high density lipoproteins. Clinica Chimica Acta 1998;269:107-24.
- Betteridge DJ. High density lipoprotein and coronary heart disease. BMJ 1989;298:974-6.
- Burtis CA, Ashwood ER, Aldrich JE. Lipids, apolipoproteins and lipoproteins. In: Aldrich JE, editor. Tietz fundamental of Clinical chemistry. 5th ed. Pennsylvania, U.S.A: W.B. Saunders Company; 2001. p. 780-94. ISBN: 0-7216-3763-9.
- Wolfman W. Reality check on menopause: Your Health Report. Spring 2002;40:34-6.
- Wald M. Menopause- A natural transition. Advanced Medicine 2003;12:25-9.
- Stevenson JC, Crook D, Godsland T. Influence of age and menopause on lipids and lipoproteins in Healthy women. Atherosclerosis 1993;98:83-90.
- Maduka IC, Onyeanusi JO, Shu EN, Duru CR. Lipid and lipoprotein profile in Nigerian non insulin-dependent diabetic patients: Biomedical Research 2007;18:49-53.
- Gorodeski GI. Update on cardiovascular disease in postmenopausal women. Best Pract Res Clin Obstet Gynaecol 2002;16:329-55.
- Murray R, Granner D, Mayes P, Rodwell V. Lipid transport and storage: In: Harpers Illustrated Biochemistry: 26th ed. 2003. p. 205-29. ISBN: 0-83853684-0.
- Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. ClinChem 1974;20:470-5.
- Groove TH. Effect of reagent pH on determination of high density lipoprotein cholesterol by precipitation with sodium Phosphotungstate-magnesium. Clin Chem 1979;25:560-4.
- Buccolo G, David H. Quantitative determination of serum triglycerides by the use of enzymes. Clin Chem 1973;19:476-82.
- Friedewald W, Levy R, Fredrickson D. Estimation of the concentration of low density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499-515.