ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 13
Modified laminoplasty for multilevel cervical myelopathy
To investigate the effectiveness of combined C3 laminectomy preserving the semispinalis cervicis into axis and modified C4-C7 open-door laminoplasty in the treatment of multilevel cervical myelopathy. 57 out of 74 patients who underwent combined C3 laminectomy preserving the semispinalis cervicis into axis and modified C4-C7 open-door laminoplasty were followed. Pre- and postoperative Japanese Orthopaedic Association (JOA) score, cervical Range of Motion (ROM) and Cervical Curvature Index (CCI) were measured. The mean operative time was 70 min and the mean intraoperaitve blood loss was 230 ml. Early postoperative neck pain occurred in 41 patients (71.9%), wound infection occurred in 2 patients (3.5%), obvious axial symptoms occurred in 9 patients (15.8%) and C5 nerve root palsy occurred in 6 patients (10.5%). There were no severe complications, such as spinal cord injury, and cerebrospinal fluid leakage. JOA score significantly increased from preoperative 8.5 ± 2.0 points to postoperative 13.8 ± 2.3 points (P<0.05). Cervical ROM decreased from 37.4° ± 10.3° to 28.2° ± 10.8° with a mean loss of 8.2° ± 5.1°. CCI decreased from 13.9 ± 7.4% to 11.3 ± 8.1% with a mean loss of 2.9 ± 2.4%. The rate of neurological function improvement was 57.0 ± 1 9.7%. Combined C3 laminectomy preserving the semispinalis cervicis into axis and modified C4-C7 open-door laminoplasty can significantly improve the neurological function of patients with multilevel cervical myelopathy and the surgical procedure is relatively simple. Therefore, this technique might be widely used in the clinical practice.
Keywords
Cervical myelopathy, Open-door laminoplasty, Anchor system, Axial symptoms, Semispinalis cervicis
Introduction
Expansive open-door laminoplasty, introduced by Hirabayashi in 1977, had been widely used to treat multilevel cervical myelopathy, cervical ossification of the Posterior Longitudinal Ligament (OPLL), developmental cervical canal stenosis, etc., and the results of operations were satisfactory [1-3]. However, the posterior cervical muscles damage caused by expansive open-door laminoplasty due to extensive and consecutive decompression could inevitably destroy the stability of cervical spines [4]. Therefore, the key point of this surgical technique was to maintain the stability of posterior cervical spines [5]. In this study, to reduce the damage to the cervical stability, combined C3 laminectomy and modified C4-C7 open-door laminoplasty were used to treat multilevel cervical myelopathy and several indexes, including pre- and postoperative Japanese Orthopaedic Association (JOA) score, cervical Range of Motion (ROM) and cervical curvature index (CCI), were measured for evaluating this surgical procedure.
Methods
General data
57 out of 74 patients with multilevel cervical myelopathy between January 2009 and October 2011 who underwent combined C3 laminectomy preserving the semispinalis cervicis into axis and modified C4-C7 open-door laminoplasty were followed. Among them, 31 were males and 26 were females and there were significant differences of surgical outcomes between male and female patients. The ages ranged from 50 to 71 y with a mean age of 63 y. Segmental or localized OPLL was observed in 17 cases and the sagittal diameter of the spinal canal was less than 12 mm in 36 cases. The mean preoperative JOA score was 8.5 ± 2.0 points (range, 4 to 11 points), and the average preoperative cervical ROM was 37.4° ± 10.3° (range, 23° to 49°), which was measured by the Nishituzi method [6] on the lateral radiographs in maximum flexion and extension. The average preoperative CCI was 13.9 ± 7.4% (range, 6.0% to 22.0%), which was calculated by the Ishihara method [7]. Intraoperative and postoperative complications were recorded. 6 months after surgery, cervical X-ray examination was performed to measure the CCI and cervical ROM. JOA score was evaluated during the last follow-up visits and the rate of neurological function improvement was calculated.
Surgical procedure
After general anesthesia, the patient was placed in the prone position with the slight flexion of neck and immobilization of head. Before laminoplasty, we decided on the open and hinged sides based on the severities of symptoms and stenosis by MRI. The more severe side was taken as the open side to enable appropriate foraminotomy and a standard midline incision was made to expose the spinous processes from C2 to C7. As a typical laminoplasty, a C3-C7 decompression was carried out, C3-C7 spinous processes were identified one by one, and C3 lamina was exposed using the Shiraish method [8]. The C3 spinous process was split using a high-speed burr and cut off from the root, and subperiosteal dissection of the paraspinous muscles was carried out to expose C3 lamina. The semispinalis cervicis insertion in C2 was preserved completely and muscles were retracted bilaterally to expose C3-C7 laminae. On the hinged side, holes for the anchors were drilled in the C4-C7 (or C5 and C7) lateral masses and four (or two) 12 mm long anchors with non-absorbable suture material were inserted into the prepared holes. On the side to be opened, a channel was made via the base of each spinous process with a hole punch. The non-absorbable suture in the end of the anchor was passed through the prepared hole in the base of the spinous process and the open side was slowly elevated to establish the C4-C7 open door. The anchor suture was tightened to fix the elevated laminae on the anchor. The C3 lamina was removed carefully using pituitary forceps and the ligamentum flavum was removed in order to completely decompress the spinal cord. The split parts of C3 spinous process were reattached by suturing and a drainage tube was placed within the wound. Within 24-72 h after operations, the tube could be removed according to the amount of drainage and the patient began ambulation after wearing a neck protection collar. The neck was immobilized until 3 weeks after surgery and functional exercise of the neck muscles was carried out after that.
Outcome evaluation
Surgery-related complications, such as postoperative earlystage neck pain, C5 nerve root palsy, wound infection, closure of opened laminae were recorded. The axial symptoms were evaluated according to the Zeng’s criteria [9], and the severity of axial symptoms was divided into four grades. Patients without axial symptoms were graded as poor and fair and those with axial symptoms were graded as good and excellent. The incidence of axial symptoms was calculated. Anteroposterior (AP) and lateral cervical spine X-rays were obtained 6 months after surgery and the cervical spine ROM and CCI were measured according to the methods used before surgery. The differences between preoperative and postoperative data were compared to calculate the losses of ROM and CCI. JOA scores were obtained during the last follow-up visits and the improvement rate of neurological function was calculated. Improvement rate=(postoperative JOA score-preoperative JOA score)/(17-preoperative JOA score) × 100%.
Statistical analysis
SPSS version 17.0 was used for the statistical analysis. The normal distribution and homogeneity of variance of the data had been verified via SPSS 17.0 before statistical analysis. Comparison of pre- and postoperative JOA scores was carried out using the independent two-sample t-test. P<0.05 was considered to be statistically significant. Meanwhile, the improvement rate of the neurological function, loss of the cervical ROM, differences between the pre- and postoperative CCI and the incidence of postoperative axial symptom were calculated.
Results
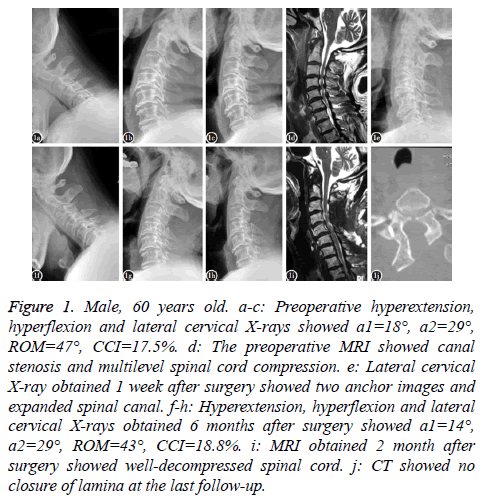
Operations were successfully completed with a mean operative time of 70 min (range, 50 to 110 min). The mean volume of intraoperative blood loss was 230 ml (range, 150 ml to 600 ml). Severe postoperative complications, including spinal cord injury and cerebrospinal fluid leakage, were not occurred. 41 patients (71.9%) had postoperative early-stage neck pain, which were relieved after 3 weeks with anti-inflammation therapy. C5 nerve root palsy was observed in 6 patients (10.5%), which improved after intravenous administration of methylprednisolone and disappeared at the last follow-up visits. Wound infection occurred in 2 patients (3.5%) and delayed wound healing was obtained after anti-infection therapy and secondary debridement. 9 patients (15.8%) had obvious axial symptoms within 6 months after surgery. The follow-up duration ranged from 6 to 32 months, with a mean of 13 months. The average postoperative JOA score was 13.8 ± 2.3 points (range, 10 to 17 points), which was significantly higher than the preoperative JOA score (P<0.05). The mean postoperative cervical ROM was 28.2° ± 10.8° (range, 18° to 46°) with a mean loss of 8.2° ± 5.1° and the average postoperative CCI was 11.3 ± 8.1% (range, 4.2% to 21.1%) with a mean loss of 2.9 ± 2.4%. The average rate of neurological function improvement was 57.0 ± 19.7% (range, 29.0% to 77.3%). No closure of lamina was observed during follow-up. The postoperative neurological and radiological outcomes are summarized in Figure 1.
Figure 1: Male, 60 years old. a-c: Preoperative hyperextension, hyperflexion and lateral cervical X-rays showed a1=18°, a2=29°, ROM=47°, CCI=17.5%. d: The preoperative MRI showed canal stenosis and multilevel spinal cord compression. e: Lateral cervical X-ray obtained 1 week after surgery showed two anchor images and expanded spinal canal. f-h: Hyperextension, hyperflexion and lateral cervical X-rays obtained 6 months after surgery showed a1=14°, a2=29°, ROM=43°, CCI=18.8%. i: MRI obtained 2 month after surgery showed well-decompressed spinal cord. j: CT showed no closure of lamina at the last follow-up.
Discussion
Open door laminoplasty is an ideal operation for treating multilevel cervical stenosis caused by cervical spondylosis or OPLL due to the significant improvement of neurological function of spinal cord [10,11]. There are several advantages of laminoplasty, including providing the widened spinal canal, avoiding postoperative instability of the cervical spine and protecting the spinal cord. It also has some postoperative complications, such as postoperative early-stage neck pain, C5 nerve root palsy, postoperative axial symptoms, postoperative laminar closure and so on [12-15]. The neck pain during early postoperative period may be related to the intraoperative damage to the musculo-ligament complex, which can be obviously relieved after physical therapy. In the current study, 41 patients (71.9%) had neck pain during early postoperative period and all of them were relieved after 3 weeks with antiinflammation therapy. The C5 nerve root palsy, which exhibits deltoid muscle paralysis, is mainly caused by mechanical stretch on the nerve root migrating from posterior cord in the foramina [16-18]. C5 nerve root palsy can be improved by symptomatic treatments.
Postoperative axial symptoms include shoulder pain, shoulder spasm, and neck pain. The postoperative incidence could be as high as 60% [14]. Postoperative axial symptoms last long and the therapeutic outcomes are poor. The persistent postoperative axial symptoms often adversely affect the patients’ quality of life. The mechanism of axial symptoms is still unclear. Most scholars consider that it may be related to the intraoperative damage to the musculo-ligament complex, which may cause instability of the cervical spine. Sun et al. [19] introduced three main causes of the axial symptoms as follows: (1) the suture stimulation-induced facet joint inflammation and subsequent local aseptic inflammation caused by the postoperative neck motion; (2) the damage to dorsal ramus of the cervical nerve resulting in muscle spasm and pain; (3) the cervical muscles disuse atrophy caused by the long-term application of neck collar and scar contraction. Therefore, more and more modified open door laminoplasties were performed to reduce the occurrence of postoperative axial symptoms [20-22].
Recently, with the rapid development of internal fixation technique and devices, some scholars tried to stabilize posterior elements in the open position with titanium miniplates and reestablish an intact spinal canal [23,24]. This method could significantly reduce the incidence of axial symptoms by preventing the postoperative suture stimulationinduced facet joint inflammation. However, those miniplates were expensive and the procedure was relatively complicated compared to the typical open door laminoplasty. Nakama et al. [25] suggested that the postoperative axial symptoms were related to the postoperative imbalance of flexor and extensor muscles in the neck, which mainly shown as a reduced power of the extensor. Semispinalis cervicis is an important structure maintaining the posterior cervical stabilizations. Most parts of the muscle are inserted into the C2 spinous process. During the traditional laminoplasty, the muscle insertion at C2 spinous process should be dissected totally or partially to expose C3 lamina. The dissection to the insertion of the semispinalis cervicis might significantly restrict the extension of the cervical spine. The loss of normal cervical lordosis and decreased ROM of cervical spine after surgery would cause and aggravate the postoperative axial symptoms. Takeuchi et al. [26-28] introduced the modified laminoplasty preserving the semispinalis cervicis inserted into C2 and suggested that this operation could effectively reduce the axial symptoms and maintain postoperative ROM of cervical spines. Compared with these methods, we performed a novel modified operation and C3 lamina was exposed by using the Shiraish’s method and performed total laminectomy of C3. After decompression, we reattached two parts of the separated spinous process by suturing to minimize the damage to the semispinalis cervis as possible. The main advantage of our method was that the decompression level was the same as that of traditional method and the function of posterior extensor muscles of the cervical spine could be effectively protected simultaneously. Moreover, anchoring method was applied in this operation to avoid the stimulation of suturing the lamina to the facet joint capsule and a “rigid door-hinge” fixation was provided to ensure early postoperative functional exercise and reduce the occurrence of postoperative cervical muscle atrophy, which played key role in reducing the incidence of postoperative axial symptoms. Therefore, our method could not only provide adequate decompression to effectively relieve the patients’ symptoms but also significantly reduce the axial symptoms. However, there were also several disadvantages of our methods, including the limitation in ROM of cervical spines caused by inappropriate anchoring and high incidence of neck pain due to the lack of standards for early postoperative functional exercise. Although the mean operative time was only 70 min and the surgical difficulty did not increase significantly, more applying experiences and more studies about this modified operation were still necessary to orthopedic surgeons for comprehensively pre-, intra- and post-operative treatment of multilevel cervical myelopathy.
Conclusion
In conclusion, the combined C3 laminectomy preserving the semispinalis cervicis into axis and modified C4-C7 open-door laminoplasty using anchoring method can improve the postoperative neurological function for patients with multilevel cervical myelopathy. In addition, the surgical procedure is relatively simple and its complications are relatively few. Therefore, this technique should be widely used in the clinical practice.
Acknowledgement
None
Competing Interests
The authors declare that no competing interests exist.
References
- Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983; 8: 693-699.
- Duetzmann S, Cole T, Ratliff JK. Cervical laminoplasty developments and trends, 2003-2013: a systematic review. J Neurosurg Spine 2015; 23: 24-34.
- Lee CH, Lee J, Kang JD, Hyun SJ, Kim KJ, Jahng TA. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: a meta-analysis of clinical and radiological outcomes. J Neurosurg Spine 2015; 22: 589-595.
- Sayana MK, Jamil H, Poynton A. Cervical laminoplasty for multilevel cervical myelopathy. Adv Orthop 2011; 2011: 241729.
- Luk KD, Kamath V, Avadhani A, Rajasekaran S. Cervical laminoplasty. Eur Spine J 2010; 19: 347-348.
- Nishituzi T. Roentgenographic studies on the cervical spine ofpatients with cervico-omo-brachial syndrome. Cent Jpn J Orthop Traumat l963; 6: 890-917.
- Ishihara A. Roentgenographic studies on the mobility of thecervical colunm in the sagittal plane. Nippon Seikeigeka Gakkai Zasshi 1968; 42: 1045-1056.
- Shiraishi T. A new technique for exposure of the cervical spine laminae. Technical note. J Neurosurg 2002; 96: 122-126.
- Zeng Y, Dang GT, Ma QJ. Curvature change of fused segment and axial syndrome/neurological function after anterior cervical fusion. Chinese J Spine Spinal Cord 2004; 14: 520-523.
- Jiang YQ, Li XL, Zhou XG, Bian C, Wang HM, Huang JM. A prospective randomized trial comparing anterior cervical discectomy and fusion versus plate-only open-door laminoplasty for the treatment of spinal stenosis in degenerative diseases. Eur Spine J 2017; 26: 1162-1172.
- Lara-Almunia M, Hernandez-Vicente J. Open door laminoplasty: creation of a new vertebral arch. Int J Spine Surg 2017; 11: 6.
- Cho CB, Chough CK, Oh JY, Park HK, Lee KJ. Axial neck pain after cervical laminoplasty. J Korean Neurosurg Soc 2010; 47: 107-111.
- Kurakawa T, Miyamoto H, Kaneyama S, Sumi M, Uno K. C5 nerve palsy after posterior reconstruction surgery: predictive risk factors of the incidence and critical range of correction for kyphosis. Eur Spine J 2016; 25: 2060-2067.
- Kimura A, Endo T, Inoue H, Seichi A, Takeshita K. Impact of Axial Neck Pain on Quality of Life After Laminoplasty. Spine (Phila Pa 1976) 2015; 40: 1292-1298.
- Lee DH, Park SA, Kim NH, Hwang CJ, Kim YT. Laminar closure after classic Hirabayashi open-door laminoplasty. Spine (Phila Pa 1976) 2011; 36: 1634-1640.
- Basaran R, Kaner T. C5 nerve root palsy following decompression of cervical spine with anterior versus posterior types of procedures in patients with cervical myelopathy. Eur Spine J 2016; 25: 2050-2059.
- Shou F, Li Z, Wang H, Yan C, Liu Q, Xiao C. Prevalence of C5 nerve root palsy after cervical decompressive surgery: a meta-analysis. Eur Spine J 2015; 24: 2724-2734.
- Cheung JP, Luk KD. Complications of anterior and posterior cervical spine surgery. Asian Spine J 2016; 10: 385-400.
- Sun Y, Zhang FS, Pan SF. The clinical application of a modified open door laminoplasty using anchor method. Chinese J Spine Spinal Cord 2004; 14: 517-519.
- Kihara S, Umebayashi T, Hoshimaru M. Technical improvements and results of open-door expansive laminoplasty with hydroxyapatite implants for cervical myelopathy. Neurosurg 2005; 57: 348-356.
- Yeh KT, Chen IH, Yu TC, Liu KL, Peng CH, Wang JH. Modified expansive open-door laminoplasty technique improved postoperative neck pain and cervical range of motion. J Formos Med Assoc 2015; 114: 1225-1232.
- Son S, Lee SG, Park CW, Kim WK. Combined open door laminoplasty with unilateral screw fixation for unstable multi-level cervical stenosis: a preliminary report. J Korean Neurosurg Soc 2013; 53: 83-88.
- Liu FY, Ma L, Huo LS, Cao YX, Yang DL. Mini-plate fixation versus suture suspensory fixation in cervical laminoplasty: A meta-analysis. Medicine (Baltimore) 2017; 96: 6026.
- OBrien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine 1996; 21: 474-483.
- Nakama S, Nitanai K, Oohashi Y, Endo T, Hoshino Y. Cervical muscle strength after laminoplasty. J Orthop Sci 2003; 8: 36-40.
- Takeuchi K, Yokoyama T, Ono A, Numasawa T, Wada K, Kumagai G. Cervical range of motion and alignment after laminoplasty preserving or reattaching the semispinalis cervicis inserted into axis. J Spinal Disord Tech 2007; 20: 571-576.
- Takeuchi K, Yokoyama T, Ono A, Numasawa T, Wada K, Itabashi T. Limitation of activities of daily living accompanying reduced neck mobility after laminoplasty preserving or reattaching the semispinalis cervicis into axis. Eur Spine J 2008; 17: 415-420.
- Takeuchi K, Yokoyama T, Aburakawa S, Saito A, Numasawa T, Iwasaki T. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3-C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine 2005; 30: 2544-2549.