ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 1
Multidirectional suture using arthroscopic suture anchors in treating superficial avulsion fractures of anterior cruciate ligament tibial insertion
Department of Joint Surgery, The Eighty-Ninth Hospital of People's Liberation Army, Weifang, PR China
- *Corresponding Author:
- Zhaoxun Pan
Department of Joint Surgery
The Eighty-Ninth Hospital of People's Liberation Army, PR China
Accepted date: June 2, 2016
Objective: This study aims to comparatively study the clinical efficacies of cruciate ligament reconstruction (CLR) and multidirectional suture using arthroscopic suture anchors (MSASA) in treating superficial avulsion fractures of anterior cruciate ligament tibial insertion (SAF-ACLTI).
Methods: This is a prospectively randomized control study. From March 2009 to April 2012, 46 patients were randomly allocated to two groups in average by random chart method. The trial group (n=23) were performed MSASA, and the control group (n=23) were performed CLR. The postoperative Lysholm scores, KT-2000 compliance indexes, PC708 balancer results, Biodex proprioception test results between the two groups were compared.
Results: The two groups were both followed up for more than 2 years, and the Lysholm scores 3 months after the surgery had no statistically significant difference (p>0.05), while such knee stability indicators as KT-2000, PC708 and Biodex, as well as the proprioception indicators, had the significantly statistical difference (p<0.05); the observation indexes all exhibited the statistically significant differences at 6 months, 1 year and 2 years after the surgery (p<0.05).
Conclusions: MSASA had better long-term efficacies than CLR in treating SAF-ACLTI.
Keywords
Arthroscopy, Anterior cruciate ligament reconstruction, Multidirectional suture of arthroscopic suture anchors, Avulsion fracture of tibial insertion.
Introduction
In recent years, with the growing popularity of various sports and the increasing of confrontational training intensities, avulsion fractures of anterior cruciate ligament tibial insertion (AF-ACLTI) accounted for about 14% of anterior cruciate ligament injuries [1], among which a considerable part of these cases exhibited the avulsion of anterior cruciate ligament lower insertion and a thin-layer sclerotin, namely the "superficial avulsion fractures of anterior cruciate ligament tibial insertion".
The ordinary fracture reduction and internal fixation method could not be used towards this particular type of damage; many clinicians would generally perform the anterior cruciate ligament reconstruction surgery towards this type of injury [2-7], and had achieved good clinical efficacies. However, many reports pointed out that the long-term of ligament reconstruction would cause more problems [8-11]: such as the fixation failure, later-stage relaxation, wiper effect, etc., and this kind of damage could not retain the original ligament lower insertion when performed the anterior cruciate ligament reconstruction, the synovia penetrated into the bone tunnel, and it would be much more likely to cause the occurrence of tendon-bone healing difficulty, proprioception deficiency and other problems. Therefore, in order to preserve the good structures of original anterior cruciate ligament, and avoid the disadvantages existed in anterior cruciate ligament reconstruction (ACLR), we performed multidirectional suture using arthroscopic suture anchors (MSASA) in superficial avulsion fractures of anterior cruciate ligament tibial insertion (SAF-ACLTI), and compared with the cases that were treated by ACLR.
Materials and Methods
General data
Inclusion criteria: 1) The patients’ general conditions could tolerate the surgery; 2) Knee anterior drawer test was significantly positive; 3) The imaging examination confirmed the Meyers-McKeever type II and III fractures of tibial plateau, the bone masses were located at the anterior cruciate ligament lower insertion and exhibited the obvious displacement; 4) the arthroscopic exploration revealed that the forms of anterior cruciate ligament was complete, with normal tensile strength, the avulsed bone masses were small or fractured but exhibited good connection with ACL, while it could not be fixed by using the tension screws; 5) with or without the meniscal tear. 6) Could cooperate the postoperative functional rehabilitation.
Exclusion criteria: 1) older than 55 years old, or associated with other osteoporosis, and diabetes; 2) associated with the knee or other part fracture and needed the fixation; 3) the injuries in the caudomedial part of ACL were severe, and lost the normal shape and tensile strength; 4) associated with knee’s other ligament injury (such as the posterior cruciate ligament, medial and lateral collateral ligaments, etc.); 5) refused to follow the treatment regimens of this study or quit the clinical trial for any reason (such as re-damaged the knee during the recovery, etc.); 6) with serious knee deformity, severe osteoarthritis and other diseases.
This study totally included 46 patients, including 33 males and 13 females, aged 13 to 44 years old, with the mean age as 28 years old, among which 16 cases were caused by traffic accidents, 21 cases were caused by sports, and 9 cases were caused by other traumas in life. The interval from getting injured to the operation was 3 to 31 days, and the average interval was 9 days. The patients were randomly divided into two groups by the random chart method, namely the trial group (n=23), who were performed MSASA, and the control group (n=23), who were performed ACLR. The present study was approved by the Ethical Committee of Eighty-Ninth Hospital of People's Liberation Army (Weifang, Shandong, China). All patients provided written informed consent before participating in the study.
This study used the 3.5 mm dual-suture anchor for the internal fixation (Arthrex, Inc., USA), Rigidfix (Johnson & Johnson, USA), Intrafix (Johnson & Johnson, USA). The surgical instruments were the arthroscopic surgical equipment set (Smith & Nephew, USA), Jesse radio frequency (Jesse, USA). The postoperative follow-up detection instrument was KT-2000 (MEDmetric Corporation, San Diego, USA), PC708 balancing instrument (Metitur Oy, Finland) and Biodex polyarticular constant speed system (Biodex, USA) for detecting the laxity degree of knee ligament and proprioceptive differences.
Surgical procedures
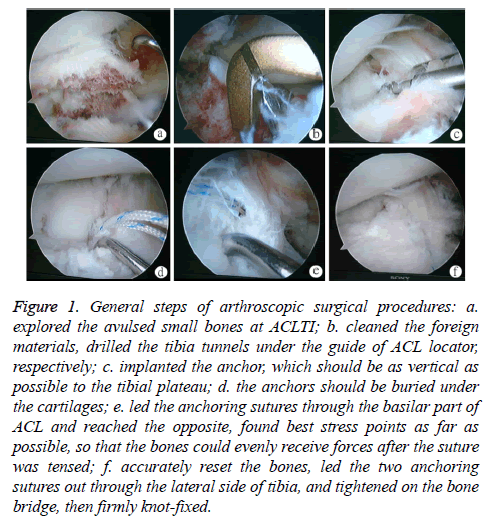
The patient was placed in the supine position, and after the successful epidural anaesthesia, the tourniquet was used to increase the blood pressure to 68 kpa for 1 hour; then, the patient was performed the routine disinfection, paved the towels, prepared the knee-arthroscopic anterior interior and lateral incisions for the conventional arthroscopic exploration (Figure 1a). One disposable planning knife was then used to clean the intra-articular haematoceles and sludged blood, during which the bone bed and the proliferation and scar tissues around the avulsed fracture blocks should be carefully cleaned to make the wound fresh, if any callus formed, it should be properly cleared, meanwhile the ligament contracture should be noted. Firstly, probed whether the patient was associated with the meniscus injury, and if there existed the combined injury, appropriate procedures should be processed. As for the damaged meniscus, the meniscal forming or suture should be performed according to the site, type and extent of the injury, and the damaged articular cartilage should be trimmed by the Jesse RF method. After that, according to the grouping situations, the trial group was performed MSASA, and the control group was performed ACLR.
Figure 1: General steps of arthroscopic surgical procedures: a. explored the avulsed small bones at ACLTI; b. cleaned the foreign materials, drilled the tibia tunnels under the guide of ACL locator, respectively; c. implanted the anchor, which should be as vertical as possible to the tibial plateau; d. the anchors should be buried under the cartilages; e. led the anchoring sutures through the basilar part of ACL and reached the opposite, found best stress points as far as possible, so that the bones could evenly receive forces after the suture was tensed; f. accurately reset the bones, led the two anchoring sutures out through the lateral side of tibia, and tightened on the bone bridge, then firmly knot-fixed.
MSASA
The 23 patients of the trial group were performed MSASA: firstly, under the arthroscopic monitoring, the probe hook was used to reset the fractured fragments, and then the angles of knee flexion were adjusted to allow the optimal reset of fractured blocks. Secondly, the anterior cruciate ligament locator was placed into, two bone tunnels were drilled from both anterior sides of avulsed site of anterior cruciate ligament tibial insertion, respectively (Figure 1b), and the anchoring suture was then led out from the anterior part of avulsed fractured parts, with the diameter as 3 mm, which could be used to pass the suture, the two bone tunnels were then led out from the anterior-inferior tibial cortex of medial tibial plateau, and the exits of these two bone tunnels should be kept 10 mm bone bridge.
The assistant was responsible for maintaining the bone position, which used the patellar lateral approach and implanted one 3.5 mm dual-suture anchor into the tibial plateau, which located in the partial outer side of avulsed site of anterior cruciate ligament tibial insertion, and the implantation direction should be as vertical as possible to the tibial plateau, or slightly sloped towards the inferior direction of lateral intercondylar ridge of tibial plateau (Figures 1c, 1d), the line-transferor was then used to lead the anchoring suture to transfer through the basilar part of anterior cruciate, as well as the surface of avulsed fractures, until finally reached the opposite side, followed by piercing out from the tibial tunnel of this side (Figure 1e), through the lateral patellar approach, the second anchoring suture was implanted onto the tibial plateau, which was on the posterior-interior edge of avulsed site of anterior cruciate ligament tibial insertion, and pierced out from the contralateral tibia tunnel by the same method. So, these two suture anchors would form the cross-fixation state on the surface of SAF-ACLTI. The avulsed bones were then further confirmed for the good contact with the bone bed, and the suture was forced tightened when the knee flexion was at 40°, followed by the knot-fixation onto the bone bridge. The arthroscopy was then performed to make sure the stability of reset bones, stretched the knee within 0° ~ 130°, and there should be no bone moving, and the tension of anterior cruciate ligament should be good (Figure 1f).
ACLR
The 23 patients of the control group were performed ACLR, folding the semitendinosus and the gracilis into four shares (with the diameter as 7 ~ 8 mm) for the single-bundle reconstruction. The ACL tibial bone tunnel was located about 2 mm posterior-interior to the original ligament centre, the ACL femoral bone tunnel was operated with the "timing position method", namely the right knee was set at the angle of 10:00 ~ 10:30; the left knee was set at the angle of 1:30-2:00. The femoral end was cross-fixed by the Rigidfix method, and the tibial end was fixed by the Intrafix method. Before fixing the tibial end, the isometric feature of reconstructed ligament should be good, stretched the ligaments to the flex the knee 30 times (0° ~ 0°), and during the Intrafix fixation, one tensioner was used to draw 100 N force.
When the two groups were completed processed, the radio frequency was used for the intra-articular complete haemostasis, and the arthroscopy was performed to completely explore the joint cavity, cleaned up the debris left. The results of Lachman test and anterior drawer test should be negative.
Postoperative processing
The two groups were performed the rehabilitation training according to the most appropriate methods.
The trial group: 1 week within the surgery, the patient exercised the isometric contraction exercises of quadriceps, performed the straight-leg rising under the brace protection daily, exercised the muscles, and performed the non-weightbearing ambulation with crutches.
1 week after the surgery, the patient started the knee flexion and extension exercises, flexed the knee to 90°, 3 weeks after the surgery and should obtain the normal flexion and extension motions 2 months after the surgery, and should wear the brace for the full weight-bearing daily activities. The brace protection could be removed three months after the surgery according to the physical examination and X-ray examination, which should show that the fractures healed, and the patient should start the gradual training, and return to normal training 6 months later.
The control group: the patient was performed the muscle strength training 3 days after the surgery, as well as the nonweight- bearing ambulation, and exercised the knee flexionextension three days later, which should reach 90° about one week after the surgery, and the flexion-extension activities should reach the normal range six weeks after the surgery.
Within 6 weeks to six months or longer, the patient should be recommended to perform the daily full weight-bearing activities with the brace protection, and returned to the normal training 12 months after the surgery.
Statistical analysis
The SPSS 17.0 software package (IBM, USA) was sued for the analysis. The measurement data were firstly performed the normal distributed test, if the measurement data met the normal distribution, the data were expressed as (x? ± s), the intergroup comparison used the paired t-test, otherwise the data were performed the rank sum test of multiple independent samples; the counting data were performed the chi-square test, with p<0.05 considered as the statistical significance.
Results
Comparison of the result about different surgery
There were none additional damage during the operation in all patients of two groups, including nerve and vascular complications. Knee Lachmann test and anterior drawer test were negative. In the first week, 3 cases in trial group and 8 cases in control group caused knee swelling. That didn’t affect the functional exercise, because it was gradually reduced a week later.
All patients were followed up for more than 2 years, the trial group was followed up for 31 ± 6 months, and the control group was followed up for 30 ± 5.5 months (t=0.59, P>0.05). The conventional X-ray examination revealed that at the postoperative three months, the tibial avulsed bone edge of 1 patient in the trial group was slightly cocked up, and the Lachman test and anterior drawer test of this patient were all negative.
The 2-year follow-up revealed that the position of bone mass was stable and exhibited no displacement, and there appeared no phenomena of pain and knee instability. The rest patients all achieved the synostosis at the postoperative 3 months. All the patients of the control group exhibited normal X-ray results at the postoperative 3-month follow-up, while the 2-year followup revealed that 4 patients exhibited the widening of tibial bone tunnel.
Comparison of Lysholm score between two groups
The postoperative Lysholm scores of the two groups were gradually increased (Table 1). In the trial group it increased from 81.8 ± 2.5 (3 months) to 87.5 ± 2.6 (2 years) and 81.6 ± 2.3 (3 months) to 85.2 ± 2.3 (2 years) in the control group.
| Group | 3 months | 6 months | 1 year | 2 years |
|---|---|---|---|---|
| Trial group | 81.8 ± 2.5 | 84.1 ± 3.3 | 85.8 ± 3.1 | 87.5 ± 2.6 |
| Control group | 81.6 ± 2.3 | 81.8 ± 3.6 | 83.3 ± 3.2 | 85.2 ± 2.3 |
| t-Test | t=0.42 | t=2.650 | t=2.551 | t=4.03 |
| P>0.05 | P<0.05 | P<0.05 | P<0.05 | |
| There were statistically significant differences between two groups (P<0.05) excluding 3 months (P>0.05) | ||||
Table 1. Comparison of lysholm score between trial group and control group.
At the postoperative 3-month follow-up, Lysholm score showed no statistically significant difference between two groups (P>0.05), while at 6 months, 1 year and 2 years followup, Lysholm score of the trial group was higher than the control group, which showed significant statistical differences (P<0.05).
Comparison of KT-2000 compliance index between two groups
With the increase of follow-up time, the KT-2000 compliance index had a gradually declining trend in trial group, which was contrary to the control group (Table 2).
| Group | 3 months | 6 months | 1 year | 2 year |
|---|---|---|---|---|
| Trial group | 0.88 ± 0.11 | 0.69 ± 0.11 | 0.64 ± 0.10 | 0.51 ± 0.12 |
| Control group | 1.38 ± 0.22 | 1.39 ± 0.20 | 1.58 ± 0.23 | 2.2 ± 0.33 |
| t-Test | t=-11.63 | t=-13.691 | t=-17.410 | t=-29.55 |
| P<0.05 | P<0.05 | P<0.05 | P<0.05 | |
| There were statistically significant differences between two groups (P<0.05). | ||||
Table 2. Compliance index detected by KT-2000 (mm).
At 2 years follow-up, the index was 0.51 ± 0.12 in trial group, and 2.2 ± 0.33 in control group. There were significant statistical differences between two groups (P<0.05).
Comparison of PC708 balancer results about two groups
At 3 months, 6 months, 1 year and 2 years, two groups' PC708 balance instrument results were statistically significant differences (P<0.05, Table 3). The trial group was 83.71 ± 1.90 and the control group was 78.22 ± 3.71 at 2 years follow-up.
| Group | 3 months | 6 months | 1 year | 2 years |
|---|---|---|---|---|
| Trial group | 81.68 ± 3.04 | 83.43 ± 2.79 | 83.39 ± 1.60 | 83.71 ± 1.90 |
| Control group | 78.99 ± 3.37 | 80.03 ± 4.21 | 77.79 ± 4.26 | 78.22 ± 3.71 |
| t-Test | t=3.25 | t=3.085 | t=6.198 | t=8.27 |
| P<0.05 | P<0.05 | P<0.05 | P<0.05 | |
| There were statistically significant differences between two groups (P<0.05). | ||||
Table 3. Score of PC708 balancing training system.
Comparison of the biodex multi-joint constant speed system results
We found that the data measured by biodex multi-joint constant speed system increased with the increasing knee flexion angle but decreased with the increasing follow-up time (Table 4).
| Follow-up time | Angle | Results | t-Test | ||
|---|---|---|---|---|---|
| Trial group | Control group | ||||
| 3months | 15° | 2.04 ± 0.22 | 2.32 ± 0.33 | t=-4.98 | P <0.05 |
| 30° | 3.14 ± 0.36 | 3.66 ± 0.37 | t=-5.64 | P <0.05 | |
| 45° | 3.58 ± 0.29 | 3.63 ± 0.33 | t=-2.18 | P <0.05 | |
| 6 months | 15° | 1.92 ± 0.24 | 2.25 ± 0.33 | t=-3.79 | P <0.05 |
| 30° | 2.53 ± 0.31 | 3.32 ± 0.41 | t=-8.23 | P <0.05 | |
| 45° | 2.75 ± 0.40 | 3.07 ± 0.33 | t=-3.33 | P <0.05 | |
| 1 year | 15° | 1.90 ± 0.34 | 2.26 ± 0.37 | t=-3.45 | P <0.05 |
| 30° | 2.37 ± 0.35 | 2.92 ± 0.50 | t=-5.29 | P <0.05 | |
| 45° | 2.56 ± 0.38 | 3.31 ± 0.35 | t=-7.66 | P <0.05 | |
| 2 years | 15° | 1.91 ± 0.32 | 2.59 ± 0.43 | t=-7.62 | P <0.05 |
| 30° | 2.14 ± 0.27 | 3.53 ± 0.39 | t=-22.27 | P <0.05 | |
| 45° | 2.54 ± 0.21 | 3.32 ± 0.37 | t=-11.23 | P <0.05 | |
| At 3 months, 6 months, 1 year and 2 years follow-up, There were significant statistical differences between two groups in each angle (P<0.05). | |||||
Table 4. Results of Biodex multi-joint constant speed detection.
At 2 years follow-up, the results of trial group were 1.91 ± 0.3 (15°), 2.14 ± 0.27 (30°) and 2.54 ± 0.21 (45°) which were 2.59 ± 0.43 (15°), 3.53 ± 0.39 (30°) and 3.32 ± 0.37 (45°) in the control group.
There were significant statistical differences between two groups (P<0.05).
Discussion
SAF-ACLTI was a special type of injury, and many scholars classified it into the cruciate ligament injury, and performed the cruciate ligament reconstruction for the treatment of SAFACLTI. However, when performing ACLR towards the SAFACLTI patients, it would be pitiful to resect the ligament entity that still had the good caudomedial part. Ma, et al. [8] thought that the ligament reconstruction would cause too large damage to the original structures, and there existed such postoperative potential risks as the synovia penetrated into the bone tunnel [9,10], poor tendon bone healing and late-stage relaxation, etc. [11]. Due to the deficiency of fractured bone fragments, the ligament reconstruction would even be short of reliable positioning markers [12,13], so that the unequal-length ligament reconstruction might be easily resulted in, thus the "bungee effects" would be led to, while would finally result in the failure of ligament reconstruction [14]. The recent studies [15-18] had proved that the reservation technology of ACL stump could provide the blood supply for the reconstructed ligament, and promote the healing of lower insertion of reconstructed ligament, thus partial knee proprioceptive feeling could be reserved. But as for the SAF-ACLTI patients, the lower insertion and its bone mass could be removed when performing ACLR, so it could not retain the advantages of ACL stump technology, meanwhile, it would lose the closure effects of inner stoma of tibial tunnel, so the synovia might easily penetrate into the bone tunnel. Therefore, in this study, the patients of the control group occurred more cases of latestage ligamentous laxity, proprioceptive deficiency and tibial tunnel enlargement. Therefore, MSASA was the best treatment method towards the SAF-ACLTI patients. In addition, the patients of the trial group could be applied the normal training gradually when reaching the synostosis (3-6 months), while the control group still needed 12 months before returned to the normal training gradually.
Indeed, the fixation methods of ACL-ASA of tibial insertion were various [19-22], and the fixation usually used a single suture, suture anchors, steel wire, absorbable nail and cannulated screw for the inner fixation. It was found in the actual clinical applications that the screw was usually used to fix large and relatively complete fractured bone blocks; the steel wire had been rarely used because of its too large shearing force towards the fractured blocks, which might easily lead to the further fractures; the suture was suitable for smaller fractures, even the comminuted fractures. When performing arthroscopic suture fixation towards the fractures, many scholars would stretch a single suture across the bone and pull it towards the tibia bed, this method could not provide the 3D fixation force, and would be prone to produce the micromovement and shifting, thus leading to the non-healing of bone blocks; especially towards the small bone blocks of SAF or broken bones, it could not maintain the good contraposition, even the suture might be loose and the bones cocked up after that [23]. The two suture anchors used in this study was formed a crosswise fixation on the surface of SAF, the anchor implanted at the rear part and the sutures led out from the anterior bone tunnel could produce enough longitudinal tension after tightened, meanwhile, the bones that were reset in the bone bed were cross wisely re-tied, so they could be firmly fixed on both anterior-posterior direction and left-right direction, which provided a firm 3D fixation pattern for the bones of ACL tibial insertion. Wang, et al. [24] reported 18 cases of tibial eminence fractures, who were performed arthroscopic absorbable suture dual-anchor for the fracture reduction and fixation, and the last follow-up revealed that except for two cases with positive Lachman test and weak positive anterior drawer test, the rest 16 cases all achieved the satisfactory results. We believed that MSASA had the following advantages: 1) could provide good fixation method of SAF; 2) could effectively prevent the shearing force caused by the steel wire; 3) could completely retain the original ACL, as well as its blood supply and proprioceptive nerves; 4) could provide a reliable 3D fixation to meet the needs of early postoperative rehabilitation; 5) could transfer the slow ligament reconstruction process after ACLR to a simpler process of fracture healing process.
In order to achieve good surgical results, the following aspects should be noticed: 1) before reset the bones, the foreign materials and bone callus within the spaces of bone bed needed to be carefully cleaned to ensure the healing interface to be fresh, and the bones could be reset well; 2) the patient with old fractures might have already existed the cruciate ligament contracture, so when stretched the cruciate ligament for the pre-expansion, the bony callus tissues should also be appropriately retained to prevent the separation gap; 3) as for the patient with stretched damages in the cruciate ligament, when cleaned the tibial plateau and bone bed, the bone bed should be appropriately deepened until the examination revealed that the tension of reset cruciate ligament was good; 4) the anchors should be implanted into the bones as perpendicularly as possible, while be prevented from implanting into to the cartilage or soft tissues. The implantation location should be at the edge of bone bed, with the anchor nail completely buried below the subchondral bone, so that the loosing and swing of anchors could be prevented; 5) used the line-transferor to introduce the suture into the contralateral bone tunnel through the basilar part of ACL, and close to the bone as much as possible, so that it could prevent to mingle excessive ligament tissues and form the elastic fixation. Because the locations of implanted anchors were deeper, and the rear anchoring and the anterior bone tunnel were located at the edge of bone bed, they would produce the downward longitudinal tension when the sutures were frapped; 6) if the bones of avulsed fracture were already broken or with poor reset of old fracture, four-suture anchoring could be performed, the two sutures could form the crisscross fixation, the other two sutures were stretched from one side and introduced into the ipsilateral bone tunnel; 7) if the patient was associated with the meniscal anterior angle injury, it could be dealt with when sewing the bone masses.
As for SAF-ACLTI, MSASA could obtain better short-term therapeutic effects than CLR. Compared with ACLR, it could retain ACL that had the normal anatomic structures, shorten the rehabilitation and protection processes, the effects of proprioception recovery were better, and it could effectively avoid the adverse events of ACLR. However, because of the relatively small case numbers in this study, the deficiency of follow-up time, as well as the difference in understanding the individual patients, the postoperative follow-up scores exhibited the difference, which might cause certain bias towards the results of this study, and its long-term efficacies till remained to be further studied.
Conflicts of Interest
All of the authors declare that they have no conflicts of interest regarding this paper.
References
- Meyers MH, McKeever FM. Fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1970; 52: 1677-1684.
- Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res 2007; 458: 180-187.
- Lidén M, Sernert N, Rostgård-Christensen L, Kartus C, Ejerhed L. Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy 2008; 24: 899-908.
- Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Individualized anterior cruciate ligament surgery: a prospective study comparing anatomic single-and double-bundle reconstruction. Am J Sports Med 2012; 40: 1781-1788.
- Marx RG. Anatomic double-bundle anterior cruciate ligament reconstruction was superior to conventional single-bundle reconstruction. J Bone Joint Surg Am 2013; 95: 365.
- Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3 to 5-year follow-up. Am J Sports Med 2012; 40: 512-520.
- Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S. Stability evaluation of single-bundle and double-bundle reconstruction during navigated ACL reconstruction. Sports Med Arthrosc 2008; 16: 77-83.
- Ma Y, Ao YF, Yu JK. Failed anterior cruciate ligament reconstrction: analysis of factors leading to instability after primary surgery. Chin Med J 2013; 126: 280-285.
- Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med 2006; 34: 1790-1800.
- Berg EE, Pollard ME, Kang Q. Interarticular bone tunnel healing. Arthroscopy 2001; 17: 189-195.
- Wen CY, Qin L, Lee KM, Wong MW, Chan KM. Influence of bone adaptation on tendon-to-bone healing in bone tunnel after anterior cruciate ligament reconstruction in a rabbit model. J Orthop Res 2009; 27: 1447-1456.
- Iriuchishima T, Shirakura K, Yorifuji H, Aizawa S, Murakami T, Fu FH. ACL footprint size is correlated with the height and area of the lateral wall of femoral intercondylar notch. Knee Surg Sports Traumatol Arthrosc 2013; 21: 789-796.
- Ferretti M, Doca D, Ingham SM, Cohen M, Fu FH. Bony and soft tissue landmarks of the ACL tibial insertion site: an anatomical study. Knee Surg Sports Traumatol Arthrosc 2012; 20: 62-68.
- Blagojevi? ZB, Crnobari? AS, Stevanovi? VM, Dikli? ID, Glisi? M, Grani? Z. Unusual position of bone tunnels in failed ACL reconstruction. Acta Chir Iugosl 2010; 57: 81-84.
- Adachi N, Ochi M, Uchio Y, Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 2000; 120: 128-133.
- Ochi M, Iwasa J, Uchio Y, Adachi N, Kawasaki K. Induction of somatosensory evoked potentials by mechanical stimulation in reconstructed anterior cruciate ligaments. J Bone Joint Surg Br 2002; 84: 761-766.
- Lee BI, Min KD, Choi HS, Kim JB, Kim ST. Arthroscopic anterior cruciate ligament reconstruction with the tibial-remnant preserving technique using a hamstring graft. Arthroscopy 2006; 22: 1-7.
- Lee BI, Kwon SW, Kim JB, Choi HS, Min KD. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy 2008; 24: 560-568.
- Wang RY, Arciero RA, Obopilwe E, Mazzocca AD. Comparison of the retro screw and standard interference screw for ACL reconstruction. J Knee Surg 2012; 25: 227-235.
- Lawrence JT, Trivedi V, Ganley TJ. All arthroscopic suture-bridge ?xation of a delaminated chondral fragment. Univ PA Orthop J 2011; 21: 83-86.
- Vega JR, Irribarra LA, Baar AK, Iñiguez M, Salgado M, Gana N. Arthroscopic ?xation of displaced tibial eminence fractures: a new growth plate-sparing method. Arthroscopy 2008; 24: 1239-1243.
- Sawyer GA, Hulstyn MJ, Anderson BC. Arthroscopic suture bridge fixation of tibial intercondylar eminence fractures. Arthrosc Tech 2013; 2: 315-318.
- Zhao J, Huangfu X. Arthroscopic treatment of nonunited anterior cruciate ligament tibial avulsion fracture with figure-of-8 suture fixation technique. Arthroscopy 2007; 23: 405-410.
- Wang Q, Li Z, Liu Y, Wang Z, Cai X, Wei M, Fu Y, Zhu J, Liu Y. Arthroscopic treatment for tibial eminence avulsion fracture using absorbable double suture anchors. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2011; 25: 220-224.