ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 14
Outcomes of modified capsular tension ring versus sulcus-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome
1Department of Ophthalmology, Fujian Provincial Hospital, Fujian Medical University, Fuzhou, PR China
2Zhongshan Ophthalmic Center, Guangzhou, PR China
- *Corresponding Author:
- Wenjie Wu
Department of Ophthalmology
Fujian Provincial Hospital, Fujian Medical University, PR China
Accepted date: June 26, 2017
Purpose: To determine the outcomes of implantation of a modified Capsular Tension Ring (CTR) and a Posterior Chamber Intraocular Lens (PCIOL) in patients with subluxated lens secondary to Marfan Syndrome (MFS).
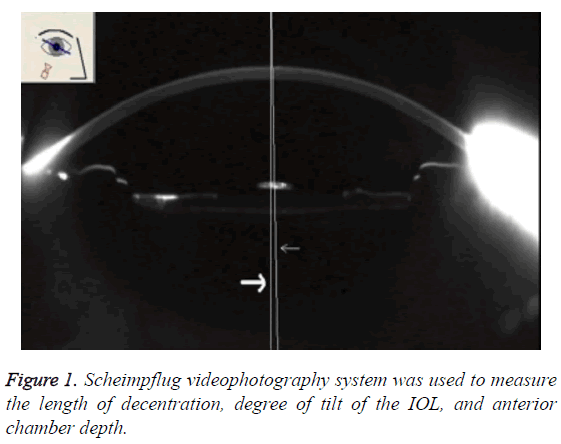
Materials and Methods: A total of 21 eyes of 12 patients with subluxated lens secondary to MFS undergoing Posterior Chamber Intraocular Lens (PCIOL) from March 2004 to February 2005 were included in this study. Scheimpflug video photography system was used to measure the degree of Intraocular Lens decentration (IOL) and tilt.
Results: The eyes of CTR group had lower degree of decentration (P=0.006) and less tilt angle (P<0.001), compared with those in Sulcus Fixation (SF) group. However, there is no difference in Anterior Chamber (AC) depth between the two groups (P=0.738). Moreover, no difference was observed in visual acuity between the two groups (P=0.676).
Conclusions: For eyes with subluxated lens secondary to MFS, a CTR technique could lead to less degree of IOL decentration and tilt. CTR technique could reduce capsular bag shrinkage and maintains the stability of the capsular bag.
Keywords
Modified capsular tension ring, Posterior chamber intraocular lens, Marfan syndrome, Decentration, Tilt.
Introduction
Marfan Syndrome (MFS), initially described by Antoine- Bernard Marfan [1], is a connective tissue disorder caused by a fibrillin-1 gene mutation which is located on chromosome band 15q21.1 [2-4]. MFS usually involves in skeletal, ocular, and cardiovascular systems with an incidence of 40 to 60 cases per million individuals [5].
The fibrillin-1 protein is a major component of the elastic microfibril of ciliary zonules, which can lead to a series of abnormal features in ocular system including ectopia lentis, myopia, axial length, astigmatism, and flat cornea [6-8]. Ectopia lentis is a major diagnostic criterion for MFS, involving in 50%-80% of patients [9]. Ectopia lentis could also result in diplopia or blurred vision if it manifested with frank subluxation. Histologic studies demonstrated that fibrillin at the equator and zonular fibers were decreased in MFS patients [10-12]. If visual acuity was progressed correctable or the refractive status unstable, lens removal was required for ectopia lentis [13,14].
Up to now, several operative approaches have been introduced, including Posterior Chamber Intraocular Lens (PCIOL) and Anterior Chamber IOL (ACIOL) implantation. It is an interesting challenge in phacoemulsification and lens implantation procedures for ocular surgeon to manage in ectopia lentis, due to zonular weakness and ectopic capsules which can lead to the failure of PCIOL. The suture fixation is often used in PCIOL procedure for most surgeons. Moreover, Capsular Tension Ring (CTR) was first introduced by Hara et al. [15] to manage in mild zonular instability. Due to inadequate recentation and stabilization of the capsular bag, CTR was modified with addition of a fixation hook by Cionni and Osher [16].
Although Takimoto et al. [17] have found that CTR with noticeable prevented the IOL decentration and tilt, few similar studies for MFS were conducted. The goal of this study is to investigate the efficacy of a CTR on prevention of marked IOL decentration and tilt after PCIOL for subluxated lens secondary to MFS.
Materials and Methods
This study was approved by the Hospital Institutional Review Board. Informed consent was collected from each patient.
The patients, who were diagnosed with subluxated lens secondary to MFS and received PCIOL surgery from March 2004 to February 2005 at our Hospital, were included in present study. Inclusion criteria were as follows: 1) patients with a diagnosis of MFS, confirmed with genetic and cardiologic evaluation; 2) patients with features of ectopia lentis and an uncorrected visual acuity. Those eyes less than a follow-up of 6 months from the time of cataract surgery and with the history of previous ocular surgery or inflammation were excluded. Finally, we selected a total of 21 eyes that underwent phacoemulsification surgery with or without implantation of a CTR for study. All examinations included visual acuity, IOL decentration and tilt, and anterior chamber depth.
Surgical procedures
All eyes surgery was performed by the same surgeon. All patients underwent the same phacoemulsification surgery procedure, except for the way of fixation, including implantation of a modified CTR and sulcus fixation of double loop. The procedure was conducted according to the description from Hayashi et al. [18]. Briefly, a no-stitch 3.2 mm clear corneal incision was performed after the eye was draped in a sterile fashion. Then, carried out the side port paracentesis and Continuous Curvilinear Capsulorhexis (CCC) with a diameter of about 5-5.5 mm. A hydrophobic acrylic IOL with 13.0 mm haptic was implanted in the insertion group after the modified CTR insertion. All foldable PCIOLs were inserted into the capsular bag. The choice about the way of fixation for PCIOL was made intraoperatively according to the surgeon’s assessment of the status of zonular weakness. When the lens subluxation ranged from 90 to 180°, a modified CTR was used. When the lens subluxation ranged from 180° to 270°, a conventional fixation was applied. The incisions were hydrated and checked for stability.
Post-operatively, all patients were managed with topical ofloxacin (0.3%) and prednisolone acetate (1%) eye drops four times daily for a month. Patients were evaluated at postoperative 3, 6 and 12 months. Scheimpflug video photography system (Figure 1) was used to measure the length of decentration, degree of tilt of the IOL and the anterior chamber depth. All examinations were conducted by experienced ophthalmic technicians who knew nothing about of this study.
Statistical analyses
All statistical analyses were performed using SPSS software. All qualitative variables are exhibited as percentages and quantitative data are expressed as mean ± Standard Deviation (SD). Comparison of discrete variables, including age and sex, was performed by χ2 test. Continuous variables of the groups were compared using Student t-test and Mann-Whitney U test. A P value less than 0.05 was considered statistically significant.
Results
In this study, six eyes received PCIOL surgery of CTR implant (CTR group), and 15 eyes received PCIOL surgery of sulcus fixation (SF group). The mean age of the patients was 21.5 ± 6.2 y in CTR group and 24.1 ± 5.9 y in SF group. The mean duration of follow-up was 13.2 ± 2.7 months (range 9 to 19 months). The characteristics of the patients were listed in Table 1. There were no difference between the two groups, including age, gender, the side of eye, and axial length.
| Characteristics | CTR | SF | P-value |
|---|---|---|---|
| No. of eyes | 6 | 15 | - |
| Age (y) | 21.5 ± 6.2 | 24.1 ± 5.9 | 0.389 |
| Gender (male/female) | 1/3 | 3/5 | 0.93 |
| Left/right | 4/2 | 8/6 | 0.577 |
| Axial length (mm) | 23.4 ± 2.1 | 23.6 ± 2.0 | 0.775 |
Table 1: Demographic characteristics.
Table 2 presented the outcomes of patients undergoing PCIOL surgery. We measured the decentration and tilt of lens using Scheimpflug videophotography system. The results showed that eyes of patients in CTR group had lower degree of decentration (P=0.006) and less tilt angle (P<0.001), compared with those in SF group. However, there was no difference in Anterior Chamber (AC) depth between the two groups (P=0.738). There were 3 eyes with visual acuity higher than 0.8, 3 were ranging from 0.5 to 0.8 in CTR group. In SF group, 6 eyes had a visual acuity higher than 0.8 and 9 9 eyes were ranged from 0.5 to 0.8. No difference was observed in visual acuity between the two groups (P=0.676).
| CTR | SF | P-value | |
|---|---|---|---|
| Decentration (mm) | 0.27 ± 0.21 | 0.56 ± 0.26 | 0.006 |
| Tilt (°) | 1.10 ± 0.69 | 2.53 ± 2.41 | <0.001 |
| AC depth (mm) | 4.38 ± 0.25 | 4.40 ± 0.86 | 0.738 |
| visual acuity | 0.676 | ||
| ≥ 76 ua | 3 | 6 | - |
| 0.5~0.8 | 3 | 9 | - |
| ≤ 0.4 | 0 | 0 | - |
Table 2: Comparison of outcomes of the PCIOL between the CTR and SF groups.
Discussions
In current study, our results demonstrated that the eyes with a modified CTR might have lower degrees of IOL decentration and tilt than those with SF technique. Moreover, we found no difference in AC depth and visual acuity between the two groups.
It is difficult to perform the PCIOL surgery in eyes with a subluxated lens. PCIOL surgery with sclera or iris suture might cause some complications, including retinal detachment and glaucoma [19]. Therefore, some surgeon introduced modified CTR technique for PCIOL surgery. Cionni and Osher reported a modified CTR technique with a fixation hook, which did not disrupt the integrity of the capsular bag and obtained good zonular stability [16]. Some studies demonstrated that the application of this modified CTR for in-the-bag IOL surgery was a relatively safe and effective choice for the management of lens subluxation and zonular deficiency [20,21]. Moreover, Takimoto et al. [17] in their study comparing the effect of CTR with no-CTR for phacoemulsification surgery found that CTR could prevent the degree of IOL decentration and tilt, and reduced the incidence of refractive prediction error. However, few reports of the outcomes of modified CTR implantation had been done for the patients with subluxated lens secondary to MFS.
In our study, there were significant difference in the degrees of IOL decentration and tilt between CTR and the control group. Although SF technique was introduced by many surgeons, it might lead to astigmatism, glare, and the loss of visual acuity, due to zonular weakness and ectopic capsules. Moreover, modified CTR could not only obtain lower decentration and tilt angle, but also hold the zonular stability. Takimoto et al. [17] suggested that there was no significant difference in the degrees of IOL decentration and tilt between CTR and no-CTR group. This was not consisted with our findings. However, they revealed CTR could also improve the degree of IOL decentration and tilt. Furthermore, experimental studies have presented that implantation of a CTR reduced capsular bag shrinkage and maintained the stability of the capsular bag, which could prevent the incidence of marked decentration and tilt of the IOL [22-24]. Lee et al. [25] showed that the degree of decentration and tilt of the IOL were lower in eyes implanted with a CTR than in eyes without a CTR. These results above were similar to our findings. Therefore, The CTR was an effective technique for subluxated lens secondary to MFS, due to its role in the extension for the capsular bag and the preservation of the circular contour of the bag for several years after surgery by preventing the degree of the decentration and tilt of the IOL. Regarding to AC depth and visual acuity, no significant differences were found between the two groups, which were consistent with previous study [17,25].
Our study had several limitations to be considered. Firstly, this study was just a retrospective designed study. Next, relatively small amount of samples might lead to bias in final results. Finally, because the option of fixation technique was made based on the surgeon’s experience and preference, some bias may be inevitable.
Conclusions
In conclusion, in eyes with subluxated lens secondary to MFS, a CTR technique could lead to less degree of IOL decentration and tilt compared to sulcus fixation. CTR technique could reduce capsular bag shrinkage and maintain the stability of the capsular bag. Further study with larger samples will be needed involving well-designed randomized control.
Acknowledgements
No funding was received in this study. We would like to thank Wenjie Wu for collecting the clinical data.
References
- Hirashima DE, Soriano ES, Meirelles RL, Alberti GN, Nose W. Outcomes of iris-claw anterior chamber versus iris-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome. Ophthalmol 2010; 117: 1479-1485.
- Sakai LY, Keene DR, Engvall E. Fibrillin, a new 350-kD glycoprotein, is a component of extracellular microfibrils. J Cell Biol 1986; 103: 2499-2509.
- Dietz HC, Cutting GR, Pyeritz RE, Maslen CL, Sakai LY, Corson GM, Puffenberger EG, Hamosh A, Nanthakumar EJ, Curristin SM, Stetten G, Meyers DA, Feancpmano CA. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 1991; 352: 337-339.
- Kainulainen K, Pulkkinen L, Savolainen A, Kaitila I, Peltonen L. Location on chromosome 15 of the gene defect causing Marfan syndrome. N Engl J Med 1990; 323: 935-939.
- Pyeritz RE, McKusick VA. The Marfan syndrome: diagnosis and management. N Engl J Med 1979; 300: 772-777.
- Dean JC. Marfan syndrome: clinical diagnosis and management. Eur J Hum Genet 2007; 15: 724-733.
- Nemet AY, Assia EI, Apple DJ, Barequet IS. Current concepts of ocular manifestations in Marfan syndrome. Surv Ophthalmol 2006; 51: 561-575.
- De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE. Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet 1996; 62: 417-426.
- Rabie HM, Malekifar P, Javadi MA, Roshandel D, Esfandiari H. Visual outcomes after lensectomy and iris claw artisan intraocular lens implantation in patients with Marfan syndrome. Int Ophthalmol 2016.
- Judge DP, Dietz HC. Marfans syndrome. Lancet 2005; 366: 1965-1976.
- Mir S, Wheatley HM, Hussels IE, Whittum-Hudson JA, Traboulsi EI. A comparative histologic study of the fibrillin microfibrillar system in the lens capsule of normal subjects and subjects with Marfan syndrome. Invest Ophthalmol Vis Sci 1998; 39: 84-93.
- Traboulsi EI, Whittum-Hudson JA, Mir SH, Maumenee IH. Microfibril abnormalities of the lens capsule in patients with Marfan syndrome and ectopia lentis. Ophthalmic Genet 2000; 21: 9-15.
- Maumenee IH. The eye in the Marfan syndrome. Trans Am Ophthalmol Soc 1981; 79: 684-733.
- Kazemi S, Wirostko WJ, Sinha S, Mieler WF, Koenig SB, Sheth BP. Combined pars plana lensectomy-vitrectomy with open-loop flexible anterior chamber intraocular lens (AC IOL) implantation for subluxated lenses. Trans Am Ophthalmol Soc 2000; 98: 247-251; discussion 251-243.
- Hara T, Hara T, Yamada Y. Equator ring for maintenance of the completely circular contour of the capsular bag equator after cataract removal. Ophthalmic Surg 1991; 22: 358-359.
- Cionni RJ, Osher RH. Management of profound zonular dialysis or weakness with a new endocapsular ring designed for scleral fixation. J Cataract Refract Surg 1998; 24: 1299-1306.
- Takimoto M, Hayashi K, Hayashi H. Effect of a capsular tension ring on prevention of intraocular lens decentration and tilt and on anterior capsule contraction after cataract surgery. Jpn J Ophthalmol 2008; 52: 363-367.
- Hayashi K, Hayashi H. Influence on posterior capsule opacification and visual function of intraocular lens optic material. Am J Ophthalmol 2007; 144: 195-202.
- Buttanri IB, Sevim MS, Esen D, Acar BT, Serin D, Acar S. Modified capsular tension ring implantation in eyes with traumatic cataract and loss of zonular support. J Cataract Refract Surg 2012; 38: 431-436.
- Chee SP, Jap A. Management of traumatic severely subluxated cataracts. Am J Ophthalmol 2011; 151: 866-871.
- Marques DM, Marques FF, Cionni RJ, Osher RH, Freitas LL. Evaluation of the modified capsular tension ring in cases of traumatic lens subluxation. Arq Bras Oftalmol 2007; 70: 746-751.
- Sun R, Gimbel HV. In vitro evaluation of the efficacy of the capsular tension ring for managing zonular dialysis in cataract surgery. Ophthalmic Surg Lasers 1998; 29: 502-505.
- Lee DH, Lee HY, Lee KH, Chung KH, Joo CK. Effect of a capsular tension ring on the shape of the capsular bag and opening and the intraocular lens. J Cataract Refract Surg 2001; 27: 452-456.
- Kurz S, Krummenauer F, Dumbach C, Pfeiffer N, Dick HB. Effect of a closed foldable equator ring on capsular bag shrinkage in cataract surgery. J Cataract Refract Surg 2006; 32: 1615-1620.
- Lee DH, Shin SC, Joo CK. Effect of a capsular tension ring on intraocular lens decentration and tilting after cataract surgery. J Cataract Refract Surg 2002; 28: 843-846.