ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2009) Volume 20, Issue 3
Prevalence and Clinical Aspects of Drug-induced Gingival Enlargement
Department of Oral and Maxillofacial Surgery
1Department of Periodontics and Community Dentistry,
2Department of Oral Pathology, Oral Medicine and Dental Radiology, Dr. Ziauddin Ahmed Dental College, Aligarh Muslim University, Aligarh, India
- *Corresponding Author:
- Syed Sayeed Ahmed
Department of Oral and Maxillofacial Surgery
Dr. Ziauddin Ahmed Dental College
Aligarh Muslim University
Aligarh-202 002, India.
E-mail: drssahmed@msn.com
Accepted date: June 02 2009
Drug-induced gingival enlargement is an iatrogenic condition which is usually not preventable. Certain factors like thorough tooth brushing, proper oral hygiene measures, regular dental flossing and professional care of oral cavity are helpful. Surgical excision of the gingival overgrowth is a treatment of choice but non-surgical methods should be adopted first. More research is needed to investigate measures that can prevent or reduce gingival overgrowth or prevent recurrence. A thorough review of literature reveals that inadequate data exist pertaining to prevalence and treatment options available for iatrogenic gingival hyperplasia. Studies with large number of samples, with statistical analysis, are required to make the data more scientific. Preventive measures have limited value and require regular assessment of patients. Hyperplasia does occur after surgical intervention but percentage of recurrence is not available. Hyperplasia can be managed to a certain extent by withdrawing or changing the medication. However, surgical intervention remains the mainstay of treatment. This paper reviews various aspects of prevalence, pathogenesis and treatment options available to manage drug-induced gingival hyperplasia.
Keywords
Diltiazem, drug induced, gingival enlargement, nifedipine induced
Introduction
Gingival enlargement is a clinical condition which has been widely studied and is directly associated with specific local or systemic conditions. There are several medications now available that cause gingival overgrowth. (Gingival enlargement or gingival overgrowth is the preferred term for all medication-related gingival lesions which were previously termed as “gingival hyperplasia”. The term gingival hyperplasia, in fact, did not reflect the histopatholgical composition of drug-induced gingival effects). These medications can be broadly divided into three categories: anti-convulsants, calcium channel blockers and immuno-suppressants [1]. Gingival overgrowth caused by these medications is not only aesthetically unacceptable but also impairs oral hygiene, resulting to periodontal disease, caries and nutrition [2].
Although the pharmacological effect of each of these drugs is different they produce a similar effect on gingival connective tissue causing common histopathological findings. This indicates common pathway of induction [3]. The exact mechanism of this effect is unclear, particularly of immunosuppressive agents [4]. However, the pathognomic mechanisms involve different factors such as dental plaque, presence of genetically predetermined gingival fibroblasts (named responders) and effect of drug itself, with all compounds affecting the trans-membrane flow of calcium [5]. This changes the ongoing metabolism of connective tissue fibroblasts, causing an increase in component of extra-cellular matrix [6-8]. Over all, there are at least two mechanisms which have been proposed. One is related to an interaction between the drug and gingival inflammation secondary to bacterial irritation. The other suggests that the drug might alter the complex cascade of biochemical events surrounding the inflammatory response, resulting in an increased gingival connective tissue production [9].
Prevalence
The prevalence of gingival overgrowth varies with drugs. Miranda, Brunet, Roset, Berini, Farré, Mendieta [10] performed a cross sectional study and compared the nifedipine-induced gingival growth to controls who had never received the drug. They found the prevalence of gingival enlargement was significantly higher in nifedipinetreated cases than in controls (33.8% versus 4.1%). The incidence occurred in 31% of the patients taking diltiazem and 21% in the verapamil-treated group. The prevalence of gingival enlargement was higher in the diltiazem (31%) than verapamil-treated patients (21%), however, in the diltiazem-treated group it was statistically significant [11]. The prevalence for cyclosporine therapy was 21-25% [12]. Hooda and Narula [13] in their study conversely indicated the prevalence with cyclosporine therapy as 9.5%. Ellis, Seymour RA, Steele et al. [14] performed a case control, community-based study to assess the prevalence of gingival overgrowth by calcium channel blockers and concluded that there was a remarkable variation in effect on the gingiva caused by different drugs and the subjects taking nifedipine appeared to be more at risk for developing clinically significant overgrowth than those taking amlodipine or diltiazem. The prevalence for nifedipine-induced gingival overgrowth was found to be 6.3% and males are three times sensitive as compared to females to develop clinically significant overgrowth.
Pathogenesis
Gingival epithelium plays an important role in protecting the periodontium from bacterial infections and mechanical trauma. It possesses the capacity of fast self renewal which contributes to gingival defense, since continuous desquamation of superficial epithelial cells prevents bacterial colonization. Therefore, it is suggested that changes in turnover rate of gingival epithelium may affect progression of periodontal disease [15].
Histologically, drug-induced gingival overgrowth is associated with thickening of epithelium with elongated rete pegs and fibrosis in the lamina propria, with increased number of fibroblasts [16,17]. Histo-chemically there is an increase in number of fibroblasts containing large amount of mucopolysaccharide sulphate in nifedipine and phenytoin induced gingival hyperplastic tissue [18].
Ramon et al. [19], from their studies, showed that the thickness of the oral epithelium in nifedipine-induced therapy was about five to 10 layers greater than in controls [19].
The volume density of oral epithelium significantly increased in cyclosporine A-induced gingival overgrowth as compared to non-medicated controls [20]. Epithelial thickening, induced by nifedipine [21] and cyclosporine A, is related to thickening of spinous layer [20]. Brown, Beawer, Bottomlay [22] suggested a functional heterogenecity between subgroups of fibroblasts in normal tissues. Fuji, Matsumoto, Nakao, Teshigawara, Akimoto [23] have shown that fibroblasts obtained from hyperplastic tissues synthesise protein approximately two times more than the cells of control group and accelerate the DNA and collagen synthesis. Satio, Mor, Iwakura, Sakamoto [24] have demonstrated that nifedipine and phenytoin increase the synthesis of basic-fibroblast growth factor (bFGF), transforming growth factor beta (TGF-β) and heparan sulphate glycosaminoglycon (HsgG) which probably induce gingival overgrowth.
In another study Sooriyamoorthy, Gower, Eley [25] concluded that an increase in androgen metabolism is an important factor for drug-induced gingival overgrowth and indicated that either the respective drugs or their metabolites can be cytotoxic for less active gingival fibroblasts and facilitate highly active populations of fibroblasts which are involved in the matrix synthesis.
Clinical studies performed by Seymour, Thomson, Ellis [26] indicate that gingival inflammation increases the incidence and severity of gingival overgrowth in nifedipine and/or cyclosporine A-mediated patients.
Nurmenniemi, Pernu, Knuuttila [27] found that that this increased epithelial thickness in both the groups, nifedipine and cyclosporine A is due to increased mitotic activity, especially in the oral epithelium.
Clinical appearance
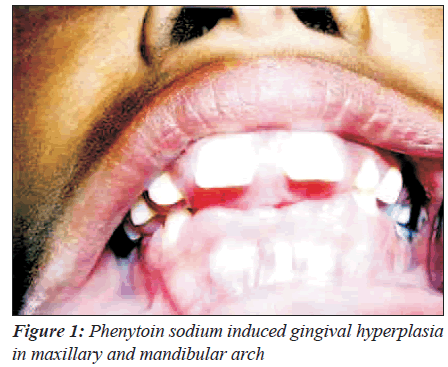
The clinical appearance of drug-induced gingival growth is mostly characteristic; however, variation is possible depending upon the site, nature of irritant and extent of inflammation. Usually there are no differences in clinical characteristics of gingival overgrowth induced by different drugs but more severe degree of gingival enlargement is seen in patient treated with phenytoin [28]. Growth normally starts from the inter-dental papilla and may favor the appearance of clinical symptoms, signs that include pain, bleeding and friability of tissue, abnormal movement of the teeth, changes of appearance, phonetics, and occlusion, as well as appearance of dental caries and other periodontal disorders (Figure 1) [29,30].
With the progress of the disease the gingivae grow into massive tissue. This extent of growth may progress to the extent that it may interfere with the common functions like speech and mastication or mastication alone. The pre-existing periodontal infection, the chemotherapy and subgingival microbiodata affect the periodontal infection and general health. If such cases are not treated, the disease leads to more severe destruction of periodontium and bone.
Treatment/prevention
The preventive measures of drug-induced gingival hyperplasia include recognition of the potential patients and rendering early intervention. Proper oral prophylaxis and good oral hygiene can prevent the phenytoin-induced gingival hyperplasia [31]. Further, a correlation exists between three variables and an increased risk of developing DIGH in patients receiving phenytoin therapy: gingivitis, a visible plaque index and duration of phenytoin therapy [32].
Prevention of recurrence after hyperplasic gingivectomy also deserves consideration. Many attempts have been made in this direction and chlorhexidine mouth wash has achieved some success. Chlorhexidine gluconate (0.1%) mouthwash is used three times daily in addition to aggressive plaque control measures. Meticulous plaque control by thorough and frequent tooth brushing and dental flossing appears to be an effective method. However, the unwanted effects of chlorhexidine of bacterial resistance and taste disturbance limit its long term use. Since phenytoin inhibits the folic acid metabolism, oral folic acid supplementation and folic acid mouthwash 1mg/ml has also been attempted, but with uncertain efficacy [33]. It has been suggested that folic acid mouthwash may reduce gingival inflammation by binding to the plaque-derived endotoxins which may ultimately reduce gingival overgrowth. This hypothesis is, however, yet to be verified.
Drug substitution/withdrawal
This is the most effective treatment of drug-induced gingival enlargement. It usually takes few weeks to resolve the gingival lesions [34,35] but response to this method varies [36].
Usually reduction in gingival overgrowth is noticed where a structurally different calcium channel blocker is used. Same therapeutic goals can be archived by using structurally different medications. However, Linderman, Lumerman, Reuben, Freedman [37] had reported the same effect where verapamil was substituted for nifedipine.
With the obvious side effects produced by phenytoin sodium, the trend of using this medication is changing. Now carbamazepine and sodium valproate are preferably used as alternatives to phenytoin sodium since they have not shown to cause drug-induced gingival hyperplasia.
The prevalence and severity of drug-induced gingival hyperplasia in patients receiving tacrolimus has been shown to be approximately half of the cyclosporine. However, even after the change in immunosuppressant medication from cyclosporine to tacrolimus, calcium channel blocker may be continued. The concomitant use of calcium channel blocker increases both the severity and prevalence of drug-induced gingival hyperplasia [38]. Thus the change in medication from cyclosporine to tacrolimus neither reduces the severity nor leads to complete resolution of overgrowth [39].
Drug therapy
Gingival hyperplasia is a known complication of cyclosporine therapy with a frequency between 21-25% in renal transplant patients [40]. A study of clinical trials revealed benefits of systemic azithromycin in such conditions [41] Hooda and Narula [13] gave azithromycin to their patients with gingival hyperplasia and symptomatic relief was noticed in all patients. They proposed that treatment with azithromycin is inexpensive and effective in short period of time, avoiding gingival surgery in large number of patients. However, patients’ refractory to treatment, discontinued cyclosporine and replacing with tacrolimus might be appropriate as gingival hyperplasia is rarely observed in tacrolimus-treated patients [13].
Systemic administration of azithromycin was found to be more effective in reducing overgrowth than the local delivery preparation [42].
The role of metronidazole in drug-induced gingival overgrowth is being regularly studied. The reported results vary. Wong, Hodge, Lewis [43] reported a total resolution of high grade cyclosporine A-induced gingival hyperplasia in each of their four patients.
Mesa, Osuna, Aneiros, Gonzalez-Jaranay, Bravo, Junco, Del Moral, O’Valle [44] conducted a double-blinded controlled randomised study image digital analysis to determine the effect of metronidazole or azithromycin on the regression of incipient cyclosporine A-induced gingival overgrowth in 40 adult renal transplanted patients. None of their patients with gingival overgrowth showed complete remission after 30 days.
However, Montebugnoli, Servidio, Prati [45] suggested that the repeated use of locally delivered metronidazole gel associated with periodontal conventional therapy as simply an additional procedure, probably providing a greater long- term efficacy in the overall management of gingival overgrowth induced by cyclosporine than conventional therapy alone. In another study, Aufricht, Hogan, Ettenger [46] observed no improvement in the gingival hyperplasia of their serially observed children after metronidazole treatment. The results differed with Wong, Hodge, Lewis, Shrpstone, Kingswood [43] for which they suggested that the variation might be due to differences in age of the patients.
However, studies on larger samples size are needed to confirm their role. The current studies have small sample size and were short term too. Further, statistical analysis is also required to decipher the significance of results. Azithromycin appeared to be more effective than metronidazole [47].
Mouth rinses
The role of antiseptic mouth rinses in the management of drug-induced gingival hyperplasia is not established. O’Neil and Figures [39] have shown that regular use of chlorhexidine mouth rinse helps reduce chances of recurrence after gingival surgery. We could not find out if any other mouthwash has been used for prophylactic or therapeutic purpose in such cases.
Non-surgical treatment
Wherever possible, non-surgical techniques should be adapted [48]. However, before rendering such treatment, local factors that enhance plaque accumulation should be eliminated. Such techniques can limit the occurrence of gingival overgrowth, reduce the plaque-induced gingival inflammation and also reduce the rate of its occurrence [49]. Professional debridement with scaling and root planning as needed had been shown to provide some relief in such cases [50]. A few individual case reports revealed that self administered oral hygiene procedures, scaling and root planning resulted in reduced drug-induced gingival over growth [51].
In extreme, medically-compromised patients in whom surgery bears more disadvantages rather than advantages, self-administered oral hygiene measures in addition to professional oral prophylaxis and root planning prove beneficial. They reduce gingival inflammation and may make surgical correction possible.
Surgical treatment
Surgical treatment is the definitive therapy of the druginduced gingival overgrowth. However, the recurrence cannot be avoided. Since the labial gingiva of anterior region is commonly involved, surgery is frequently performed, primarily for aesthetic reasons, before any functional consequences are seen. Seymour et al. [52,53] suggested that surgical interventions should be carried out when clinical overgrowth index score is evident.
External bevel gingivectomy and internal bevel gingivectomy are two commonly practised approaches. External bevel gingivectomy is the simple excision of the excessive gingival tissue with secondary healing. Internal (reverse) bevel gingivectomy is often used in place of external bevel technique, where the tissue to be excised is thick, and a long bevel incision would be required to create a knife edge margin [54]. This highly technical approach has benefit of limiting the large denuded connective tissue wound that results from external gingivectomy, thereby minimizing the post operative pain and bleeding [55]. Both the techniques of gingivectomy are essentially limited to the treatment of pseudo-pockets. The common surgical technique is the simple excision of excessive gingival tissue with secondary healing. Peri-operative haemorrhage is main intra-operative complication or disadvantage of gingivectomy [56]. There are few studies on recurrence rates.
The apically repositioned full thickness flap is a better technique and bears many advantages. It eliminates periodontal pocket, improves the alveolar bone morphology, preserves the attached gingiva and improves aesthetics in the labial region when moderate periodontitis with gingival overgrowth is treated. This technique is specially indicated in the cases with lack of keratinized tissues or in the presence of osseous defect [57].
The role of periodontal flap surgery in drug-induced gingival overgrowth has not been established. Mavrogiannis, Thomason, Seymour, Ellis [58] found no difference between the treatments with respect to gingival overgrowth. Further, flap surgery may be complicated by excessive gingival enlargement.
Lasers
There are many types of lasers available to treat gingival overgrowth. Lasers possess remarkable tissue-cutting ability and provide rapid haemostasis. Lasers with the cutting of tissues also generate a coagulated tissue layer along the surgical wound which promotes healing [59]. These properties of lasers make the management of drug-induced gingival overgrowth accurate, bloodless operative phase, less painful post-operative phase, minimal oedema and scarring [60] and avoid need of periodontal dressing. Thus CO2 laser had been used to excise gingival over growth and studies demonstrated the technique significantly lowered the rate of recurrence and patients’ preference of the technique [61]. Although the technique bears all the desired benefits, it involves costly equipment.
Conclusion
Gingival enlargement is a clinical condition which has been widely studied and is directly associated with specific local or systemic conditions. It is very rare that gingival enlargement presents without a clear underlying aetiology. Recently, McLeod et al. reported gingival enlargement in post-partum phase, treated with non-surgical and surgical periodontal therapy [62].
We have covered almost all the aspects of drug-induced gingival growth presented in literature. Clinicians would find the paper helpful in deciding the treatment strategy in drug induced gingival overgrowth. It should always be kept in mind that when drugs which cause gingival enlargement are started, the patient should be evaluated for gingivitis, educated on dental and oral hygiene, motivated to brush thoroughly, use dental floss regularly and advised for regular dental check-ups. On the other hand, physicians should also visually examine oral cavity on every visit of the patient and if any changes are noticed, consider therapy and the required dental treatment. Whatever strategy is decided, focus should be on the prevention of growth and recurrence.
References
- Seymore RA, Thomson JM, Ellis JS. The pathogenesis of drug induced gingival overgrowth. J Clin Periodontol 1996;23:165-75.
- Hassel TM, Hefti AF. Drug-induced gingival overgrowth: Old problem, new problem. Criti Rev Oral Biol Med 1991; 2:103-37 .
- Akimoto Y, Tanaka S, Omata H, Shibutani J, Nakano Y, Kaneko K, et al. Gingival hyperplasia induced by nifedipine. J Nihon Univ Sch Dent 1991;33:174-81.
- Bulut S, Uslu H, Özdemir BH, Bulut ÖE. Analysis of proliferative activity in oral gingival epithelium in immunosuppressive medication induced gingival overgrowth. Head Face Med 2006;2:13.
- Hefti AF, Eshenaur AE, Hassel TM, Stone C. Gingival overgrowth in cyclosporin A treated multiple sclerosis patients. J Periodontol 1994;65:744-9.
- Seymour RA. Calcium channel blockers and and gingival overgrowth. Br Dent J 1991;170:376-9.
- Offenbacher S. Effects of dilantin on monocyte growth factors. J Periodontol 1993;64:237-8.
- Hassel T. Evidence that Cyclpsporine, phenytoin and dihidropyridines elicit overgrowth by mechanisms. J Dent Res 1990;69:164.
- Brown RS, Beaver WT, Bottomley WK. The mechanism of drug- induced gingival hyperplasia. J Oral Pathol Med 1991;20:201-9.
- Miranda J, Brunet L, Roset P, Berini L, Farré M, Mendieta C. Prevalence and risk of gingival enlargem-ent in patients treated with nifedipine. J Periodontol 2001;72:605-11.
- Miranda J, Brunet L, Roset P, Berini L, Farre M, Mendieta C. Prevalence and risk of gingival overgro-wth in patients taking diltiazem or verapamil. J Clin Periodontol 2005;32:294-8.
- Pernu HE, Pernu LM, Knuutila ML, Huttunen KR. Gingival overgrowth among renal transplant recipients and uraemic patients. Nephrol Dial Transplant 1993;8:1254-8.
- Hooda AK, Narula AS. Azithromycin in the treatment of gingival hyperplasia in renal allograft recipients on cyclosporine. Indian J Nephrol 2004;15:53-5.
- Ellis JS, Seymour RA, Steele JG, Robertson P, Butler TJ, Thomason JM. Prevalence of gingival overgrowth induced by calcium channel blockers: A community based study. J Periodontol 1999;70:63-8.
- Komman KS, Page RC, Tonetti MS. The host response to the microbial challenge in periodontitis: Assembling the players. Periodontol 2000 1997; 14: 33-53.
- Itoiz ME, Carranza FA. The gingiva. In: Clinical Periodontlogy 8th ed. Carranza FA, Newman MG, editors. Philadelphia: WB saunders; 1996. p. 12-9.
- Barak S, Engelberg IS, Hiss J. gingival hyperplasia caused by nifedipine. Histologic findings. J Periodontol 1987;58:639-42.
- Lucas RM, Howell LP, Wall BA. Nifedipine induced gingival hyperplasia- A histochemical and ultrastructural study. J Periodontal 1985;56:211-5.
- Ramon Y, Behar S, Kishon Y, Elberg IS. Gingival hyperplasia caused by nifedipine-a preliminary report. Int J cardiol 1984;5:195-204.
- Wondimu B, Reinholt FP, Modeer T. Sterologic study of cyclosporin- A induced gingival overgrowth in renal transplant patient. Eur J Oral Sci 1995;103:199-206.
- Barak S, Engelberg IS, Hiss J. Gingival hyperplasia caused by nifedipine. Histologic findings. J Periodontol 1987;58:639-42.
- Brown RS, Beawer WT, Bottomlay WK. On the mechanism of drug induced gingival hyperplasia. J Oral Pathol Med 1991;20:201-9.
- Fuji A, Matsumoto M, Nakao S, Teshigawara H, Akimoto W. Effect of calcium channel blockers on cell proliferation, DNA synthesis, and collagen synthesis of cultured gingival fibroblasts derived from human
- nifedipine responders and non-responders. Arch Oral Biol 1994;36: 99-104.
- Sat io K, Mor i S, Iwakura M, Sakamoto S. Immunohistochemical localization of transforming growthfactor beta, b-FGF and Hs Gg in gingival hyperplasia induced by nifedipine and phenytoin. J Periodontal Res
- 1996;31:545-55.
- Sooriyamoorthy M, Gower DB, Eley BM. Androgen metabolism in gingival hyperplasia induced by nifedipine and cyclosporine. J Periodontal Res 1990;25:25-30.
- Seymore RA, Thomson JM, Ellis JS. The pathogenesis of drug induced gingival overgrowth. J Clin Periodontol 1996;23:165-75.
- Nurmenniemi PK, Pernu HE, Knuuttila ML. Mitotic activity of keratinocytes in nifedipine-and immunosuppressive medication-induced gingival overgrowth. J Periodontol 2001;72:167–73.
- Miranda J, Brunet L, Roset P, Berini L, Farré M, Mendieta C. Prevalence and risk of gingival enlargement in patients treated with nifedipine. J Periodontol 2001;72:605-11.
- Carranza FA. Gingival enlargement. In: Carranza FA, Glickman S, editors. Clinical Periodontology. Philadelphia: WB Saunders Co.; 1990. p. 125-48.
- Penarrocha M, Bagan JV, Anolina MM, Alfaro AA. Gingival enlargement induced by phenytoin. Revista Europea Odontostomatología 1989;1:41-8.
- Hall WB. Dilantin hyperplasia: a preventable lesion. J Periodont Res 1969;4:36-7.
- Modeer T, Dahlof G, Theorell K.Oral health in noninstitutionalized epileptic children, with special reference to phenytoin medication. Community Dent Oral Epidemiol 1986;14:165-8.
- Poppel TD, Keeling SD, Collins JF, Hassell TM. Effect of folic acid on recurrence of phenytoin-induced gingival overgrowth following gingivectomy. J Clin Periodontol 1991;18:134-9.
- Khocth A, Schneider LC. Periodontal management of gingival overgrowth in the heart transplant patient: A case report. J Periodotol 1997; 68:1140-6.
- Raman PG, Mishra VN, Singh D. Nifedipine induced gingival hyperplasia. Journal of the Association of Physicians of India 1988;36: 231-3.
- Marshall RI, Bartold PM. A clinical review of drug induced gingival overgrowth. Oral Surg Oral Med Oral Pathol 1993;76:543-8.
- Linderman D, Lumerman H, Reuben S, Freedman PD. Gingival hyperplasia associated with nifedipine therapy. Report of a case. Oral Surg Oral Med Oral Pathol 1984;57:620-2.
- Ellis JS, Seymour RA, Taylor JJ and Thomason JM. Prevalence of gingival overgrowth in transplant patients immunosuppressed with tacrolimus. J Clinical Periodontology 2004;31:126-31.
- O’Neil TC, Figures KH. The effects of chlorhexidine and mechanical methods of plaque control on the recurrence of gingival hyperplasia in young patients taking phenytoin. Br Dent J 1982;152:130-3.
- Pernu HE, Pernu LM, Knuutila ML, Huttunen KR. Gingival overgrowth among renal transplant recipients and uraemic patients. Nephrol Dial Transplant 1993;8:1254-8.
- Strachen D, Burton I, Pearson GJ. Is oral azithromycin effective for treatment of cyclosporine-induced gingival hyperplasia in cardiac transplant patients? J Clin Pharm Ther 2003;28:329-38.
- Nafar M, Ataie R, Einnolahi B, Nematizadeh, Firoozan A, Poorrezagholi F. A comparison between the efficacy of systemic and local azithromycin therapy in treatment of cyclosporin induced gingival overgrowth in kidney transplant patients. Transplantation Proceedings 2003;35:2727-8.
- Wong W, Hodge MG, Lewis A, Shrpstone P, Kingswood JC. Resolution of cyclosporin induced gingival hypertrophy with metronidazole. Lancet 1994;343:986.
- Mesa FL, Osuna A, Aneiros J, Gonzalez-Jaranay M, Bravo J, Junco P, et al. Antibiotic treatment of incipientdrug-induced gingival overgrowth in adult renal transplant patients. J Periodontal Res 2003;38:141–6.
- Montebugnoli L, Servidio D, Prati C. Effectiveness of metronidazole gel on cyclosporin induced gingival overgrowth in heart transplant patients. Clin Oral Invest 2002:6:24–7.
- Aufricht C, Hogan EL, Ettenger RB. Oral metronidazole does not improve cyclosporin A induced gingival hyperplasia. Pediatr Nephrol 1997;11:522-55.
- Chand D, Quatricchi J, Poe SA, Terezhalmy GT, Strife CF, Cunningham RJ. Trial of Metronidazole vs.azithromycin for treatment of cyclosporine induced gingival overgrowth. Pediatr Transplant 2004;8:60-4.
- Montebugnoli L, Servidio D, Bernardi F. The role of time in reducing gingival overgrowth in heart transplanted patients following cyclosporin therapy. J Clin Periodontol 2000;27:611-4.
- Montebugnoli L, Servidio D, Bernardi F. The role of time in reducing gingival overgrowth in heart transplanted patients following cyclosporin therapy. J Clin Periodontol 2000;27:611-4.
- Somacarrera ML, Lucas M, Scully C, Barrios C. Effectiveness of periodontal treatments on cyclosporine induced gingival overgrowth in transplant patients. Br Dent J 1997;183:89-94.
- Cianter M. Nifedipne-induced gingival overgrowth: remission following non surgical therapy. Dent Update52. Seymour RA, Smith DG, Tumbull DN. The effect of phenytoin and sodium valproate on the periodontal health of adult epileptic patients. J Clin Periodontol 1985; 12:413-9.
- Thomason JM, Seymore RA. Phenytoin induced gingival overgrowth in general medical practice. J Dent Res 1990;69:969.
- Marshal RI, Bartold PM. A clinical review of drug induced gingival oral growth. Oral Surg Oral Med Oral Pathol 1993;76:543-8.
- Grover V, Kapoor A, Marya CM. Amilodipine induced gingival hyperplasia. J Oral health Comm Dent 2007;1:19- 22.
- Liboon J, Funkhouser W, Terris DJ. A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery and constant-voltage electrocautery. Otolaryngol Head Neck Surg 1997;116:379-85.
- Popova C, Mlachkova A. Surgical Approach to druginduced gingival enlargement in real transplant patients. J IMAB-Annual Proceedings (Scientific Proceedings) 2007, book 2.
- Mavrogiannis M, Thomason JM, Seymour RA, Ellis JS. The efficacy of the three different surgical techniques in the management of drug induced gingival overgrowth. J Clin Periodontol 2006;33:434-9.
- Goharkhay K, Moritz A, Wilder-Smith P, Schoop U, Kluger W, Jakolitsch S, et al. Effect on oral tissue produced by a diode laser in vitro. Lasers Surg Med 1999;25:401-6.
- Barak S, Kaplan I. The CO2 laser in the excision of gingival hyperplasia induced by nifidipine. J Clin Periodontol 1988;15:633-5. 61. Mavrogiannis M, Thomson JM, Seymour RA and Ellis JS. The efficacy of three different surgical techniques in the management of drug induced gingival overgrowth. J Clin Periodontol 2006;33:434-9.
- Mc Leod ED, Stoeckel D, Contreras J, Reyes E. Severe Post partum gingival enlargement- A case Report. J Periodontol posted online on 16th April 2009.