ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2021) Biomedical Applications in Health Sciences
Principles and effectiveness of microbiological containment measures in COVID-19 pandemic induced by SARS-CoV-2.
Ayesha Rafiq1, Abeer Kazmi2,3*, Amir Ali3,4, Sher Mohammad3, Naeem Shah5, Kiran Shabir6, Sumaiya Khatoon7
1Department of Biotechnology, Kinnaird College for Women University, Lahore, Pakistan
2Department of Biotechnology, Abdul Wali Khan University Mardan (AWKUM), Pakistan
3Biotechnology Laboratory, Agricultural Research Institute, (ARI) Tarnab, Peshawar, Pakistan
4Department of Botany, PMAS, Arid Agriculture University, Rawalpindi, Pakistan
5Department of Psychology, Islamia College University, Peshawar, Pakistan
6Department of Nursing, Shifa Tameer-e-Milat University, Islamabad, Pakistan
7Department of Physiotherapy, Superior University, Lahore, Pakistan
- Corresponding Author:
- Abeer Kazmi Department of Biotechnology
Abdul Wali Khan University Mardan (AWKUM)
Mardan
Pakistan
Accepted date: February 11, 2021
An outbreak of deadly clinical syndrome COVID-19 in Wuhan, China has spread rapidly across the world. It is currently required to develop methods and principle of containment measures with risk assessment, categorize the laboratory design, approaches the training and procedures to evaluated compliance. Considering the transmission dynamics of coronavirus pathogen (physical contact, droplet, or aerosol), certaineffectivemeasuresshould be followed to reducetheexposure of risk. Theseguidelinesareeffective, not only for thehealthworkers but also forgeneralpublic to encouragethemforadapting protectivebehaviours whichwill help to overcomethis pandemicsituation. The rationalandoptimizeduse of PPEs willserve as an initiative measure in solving theirglobal crisis.
Keywords
Microbiology, SARS-CoV-2, COVID-19 pandemic, Personal Protective Equipments (PPEs), Psychological stress.
Introduction
COVID-19 emerges as a pandemic named as (SARSCOV- 2) [1]. On 11th March, 2020 WHO declare COVID- 19 as pandemic with 657,140 cases in 195 countries with 30,451 reported deaths with 19% severe symptom cases with 2.3% mortality rate recorded along with lower frequency gastrointestinal indications, more greater transmissibility more patients with mild symptoms, also less facilities , distinguish COVID-19 [2,3]. According to the recent updates (on 29th January, 2020), 102,041,000 are infected with COVID-19 with 2,201,043 deaths arround the world [4]. People with all ages can get infected with corona, the most vulnerable ages are old ones (65 above) however they get themselves protected by adopting good hand hygiene and good respiratory hygiene [5]. They have both direct (through personal contact and infectious droplets exposure) and indirect (aerosolized material & animal vectors) transmission [6]. Biosafety concerns and risk assessment for research facility work raised through this outbreak [7].
Literature Review
Transmission of SARS-CoV-2
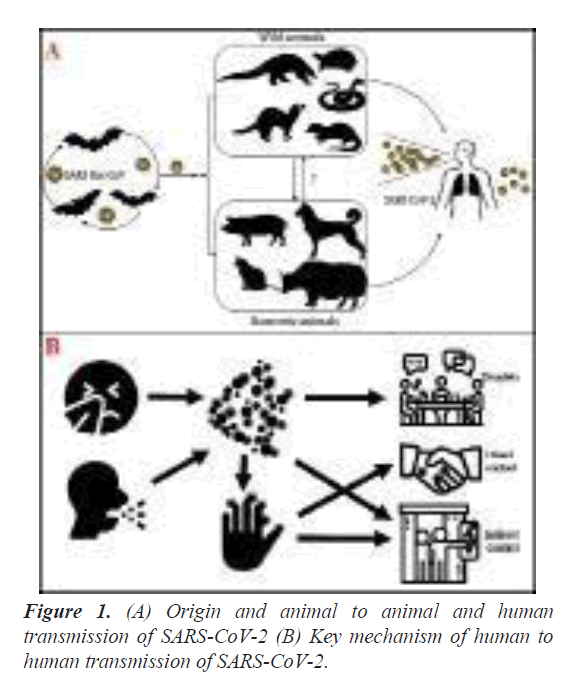
Some coronaviruses that infect animals can be spread to people and then spread between people, but this is rare. This is what happened with SARS-CoV-2, which likely originated in bats [8,9]. The first reported infections were linked to a live animal market, but the virus is now spreading from person to person [10]. The virus can spread from an infected person’s mouth or nose in small liquid particles when they cough, sneeze, speak, sing or breathe heavily. These liquid particles are different sizes, ranging from larger ‘respiratory droplets’ to smaller ‘aerosols’. Other people can catch COVID-19 when the virus gets into their mouth, nose or eyes, which is more likely to happen when people are in direct or close contact (less than 1 metre apart) with an infected person [11,12]. Current evidence suggests that the main way the virus spreads is by respiratory droplets among people who are in close contact with each other. Aerosol transmission can occur in specific settings, particularly in indoor, crowded and inadequately ventilated spaces, where infected persons spend long periods of time with others, such as restaurants, choir practices, fitness classes, nightclubs, offices and/or places of worship [13]. The virus can also spread after infected people sneeze, cough on, or touch surfaces, or objects, such as tables, doorknobs and handrails (Figure 1). Other people may become infected by touching these contaminated surfaces, then touching their eyes, noses or mouths without having cleaned their hands first [14].
Psychological effects of COVID-19
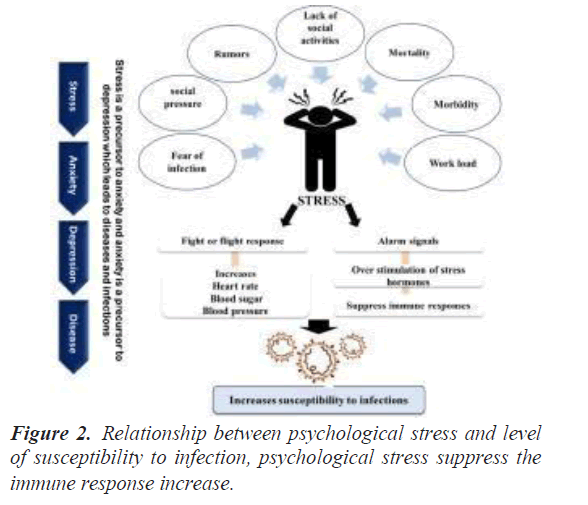
Psychological stress and depressive disorders are the major outcomes of viral epidemics, as reported for the Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) [15]. The outbreak of novel Coronavirus (2019-nCoV) in Wuhan, China, at the beginning of 2020 is thought to be the continuation of outbreaks caused by SARS-Coronavirus (SARS-CoV) in 2002 and MERS-Coronavirus (MERS-CoV) in 2009 [16]. To contain the outbreak, healthcare and management authorities imposed lockdown in several countries, suspended travelling across the country, social activities and gatherings at public places. The governments of those countries are taking every measure including deploying military doctors, and drugs and vaccine development to curb the rapid spread of infection [3]. However, considering the current epidemic and the risk of further epidemics and pandemics, attention is needed to the psychological health of normal, suspected, and infected peoples. Especially, the people working at the frontline against the infection are prone to develop depressive disorders. The current panic situation and the menace of imminent endemics related to COVID-19 have brought into forefront the urgent need to prepare for their consequences. The aftermath of such outbreaks harm both physical and mental health but currently, the healthcare service providers are focusing on physical health only that includes therapies and treatment to pneumonic symptoms of infected individuals. However, ignoring the profound importance of psychological health may culminate into serious mental problems. Thus, it is necessary to identify and properly address mental health abnormalities.
In a broader aspect, it is difficult to accurately predict the extent of mortality and morbidity and the chances of epidemics and pandemics related to the newly emerged pathogenic viruses. Considering the current situation of the world environment, viral outbreaks may affect humans, without causing extensive fatalities however their psychological impacts can be serious such as anxiety, insomnia, panic behavior, fear, and hopelessness [17].
Effects of psychological stress on immunity
In contrast, viral outbreaks in some cases may infect thousands of people, causing hundreds to thousands of fatalities and spread around the globe, thereby affecting millions of people to induce different psychiatric disorders [18]. To cope with such outbreaks and epidemics, the healthcare authorities should have affective plans according to the responses of the people. The psychological stress originating from several sources also suppress the immune system, leave the individual susceptible to several infectious respiratory illnesses including coronavirus infection, and increases mortality (Figure 2) [19]. Immune function during psychological stress is influenced either by hormone-mediated alteration of immune cells or autonomic nerves innervating lymphoid tissue [20]. Furthermore, psychological stress modulates the production of pro-inflammatory cytokines and is linked with the subsequent hospitalization and poor treatment outcomes for pneumonia [21]. Therefore, clinical psychologists or psychiatrists should come forward to encourage individuals for healthy activities. Moreover, the people should be provided with counseling and guidance at specified public centers, equipped with psychologists, and psychiatrists.
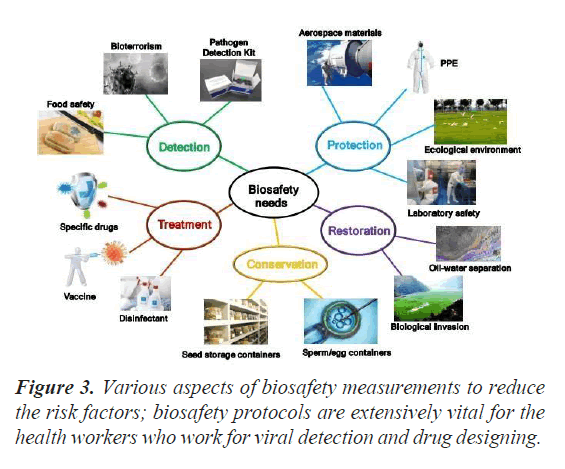
Biosafety principles and categorization of containment levels
Practices and containment measures in order of evaluation, presence of agent with infectious dose and pathogenicity, characteristic course of contamination just as different courses of disease coming about from lab controls (ingestion, parenteral, airborne), stability agent in the environment, and susceptible host presence (human or animal) [22].
Risk Group-3 of pathogens classified as animal coronaviruses causing devastating enteric respiratory syndrome in poultry and livestock [23]. In biological agents, coronavirus with SARS-COV should not be longer considered in Risk Group-2 [24,25]. BSL-3 facilities, equipment, and work practices require cell culture (viral) and controls of SARS-COV culture purpose for analysis, research, or manufacturing (e.g., arrangement of SARS diagnostic tests) (Figure 3) [26].
Definite diagnostic conditions
Light exposure of germicidal ultra-violet (UV-C) exhibited no remarkable impacts on inactivation of viruses for as long as more than two days [27]. COV was optimum at pH 6.0–6.5 while virus is inactivated under extreme acidic conditions [28]. Since no studies have yet centered on the sensitivity of corona virus to analyzed the efficiency of chemical and physical strategies for inactivation of virus.
Laboratory design (primary and secondary containment)
SARS is recorded and test the sample from different countries include the model of diagnostic activities [29]. Laboratory activities in primary section are discoveries, investigation, and creation (analytic tests assembling) [30]. Secondary laboratory activities are cell culture refeeding, centrifugation, pipetting, and cell culture initiation [31]. The biological risk assessment and the kind of manipulation introduced, SARS-COV should be handled in accordance to the proper containment measures in order to protect from research contamination [32].
Approaches with medical procedures
WHO's recommendations for the rational utilization of personal protective equipment (PPE) in health care and network settings, just as during the handling of load; include gloves, medical masks, goggles or a face shield, and gowns, just as for methods evaluated , respirators (for example N-95 or FFP-2 standard or identical) and aprons [33,34]. It is planned for those engaged with distributing and managing PPE, just as general health specialists and people in health care and network settings, and it gives data about when PPE use is generally suitable. WHO will proceed with update these suggestions as new information opens up [35]. PPE will greatly be focused on those caring about patients with symptoms or cleaning premises contaminated by droplets that may contain the virus [36]. This will permit PPE to be focused on those that require it; it is significant that you are trained in its use [37,38]. The virus lives longer on plastics than clothes, so if not accurately use and discarded, for example, masks can be become vessels for spreading disease [39,40].
Effectiveness of containment measures
WHO declared the world wide outbreak of a novel Coronavirus (nCoV) on 30, January 2020 and different containment measures are recommended for handling of coronaviruses sample and performing the serological tests or analysis with the main objective of saving lives by minimizing its adverse consequences [41,42]. Risk Communication and Community Engagement (RCCE) documented the initial response and guidelines, published by WHO to help in preventing infodemics about the COVID-19 [43] and effectively deliver the complex scientific knowledge to make it understandable by population. These guidelines encourage the people to adapt protective behaviors. The pandemic of COVID-19 has become a Public Health Emergency of International Concern and its human-to-human transmission through close contact and respiratory droplets which imparts a greater risk on Health Care Workers (HCWs) and their safety is the today’s major concern [44,46].
To protect the HCWs from potential spread of COVID-19, following containment measures plays the principle role:
Effective protective measures for healthcare facility
1. Screening and acuity-based triage: A well-defined and separate area or triage station should be created at the entrance of every health care facility for screening purpose [47]. Sorting out the suspected patients by screening of their severity helps to categorize the patient’s condition, containment risk to the work place and urgent medical treatments for deserving ones [48]. Proper hand hygiene equipment, masks and aprons should be given to the visitors under the supervision of HCW before sending them in to the COVID-19 patients as it will limit the outbreak of the virus [49,50]. To reduce the risk of co-infections, and the close relatives and closed ones should be treated as suspect individuals regardless of any prominent symptoms [51].
2. Managing patients and their placement: Isolation of suspected and confirmed case of COVID-19 is mandatory [3,52]. Proper counseling of patient will help to reduce the anxiety and proved to be effective during the treatment. Maintain 1-meter distance between all patients, HCWs all the faculty members [53]. Use fixed paths for in and out of the patient’s room as it will minimize the spreading and exposure to limited area [54,55]. Environmental Protection Agency (EPA) registered disinfectants are recommended in hospital cleaning which are proven to be effective against viral pathogens [56,57].
3. Wet-Sanitization: Regular environment cleaning and disinfection is performed for Infection Prevention and Control (IPC). According to the Biosafety Protocol documented by Centers for Disease Control and Prevention (CDC) [58,59]:
• 1% sodium-hypochlorite, 0.5% hydrogen peroxide ammonium or phenolic compounds solution is mixed with 62-71% Ethanol for surface disinfections [60].
• Donning and doffing of PPEs should be considered according to the removal instruction before visiting the next patient [61].
• To sanitize dedicated devices such as stretcher, ambulance, bio-contaminant units, ventilators and radiological equipment etc., use chlorine dioxide in the conc. ≥ 0.1% or 1000 ppm (parts per million) to rinse for 1-2 mint and then let it dry after each use as they possess the high potential load of contamination [62].
4. High-Level Disinfection (HLD): For automated and dry-sanitization, Antigermix platforms are used which has low-pressured photons of UV-C lights as a digital high level disinfectant [63].
5. Clinical sampling: Ensure that all the SOPs are being followed by the staff who are going to take samples. As it’s a respiratory virus, oral swab samples are used for standard detection of viral antigen [64]. Oral swabs should be taken twice with the gap interval of 24 hours [65]. If both are negative, the person is considered to be viral-cleansed. Suspected individuals are confirmed after Nucleic Acid Amplification Tests (NAAT) such as RTPCR. Additionally, non-respiratory samples include e.g., blood, and stool can also be used for detection as they do not possess major containment risk to the laboratories is BSL-2 is adapted. In case of endotracheal intubation, bronchoscopy or centrifuging the sample, powdered airpurifying respirators should be installed at the site for such aerosol gatherings [66].
6. Sample shipment: COVID-19 samples should be treated as category B specimens.In case of unavailability of testing equipment or materials, the sample should be appropriately labeled and transported to the nearest central laboratory in biohazard as early as possible [67]. For this purpose, specimen should be tightly capped and wrapped in zip-locked bags carried in biohazard-labeled leak-proof cryo-box [68] which should be hand-delivered to ensure the sample safety. Make sure that sample-shipment is done within 72 hours after collation and stored at -80oC temperature on dry-ice not on the frost-free freezers which certainly have temperature fluctuation, avoid the repeated freezing [69].
7. Analytical consideration of shipment: Automated messaging system such as Tiger Connect which will be uploaded the data on laboratory’s medical record and facilitate the supervisors with its tracking position [70].
8. Laboratory handling of sampling: On the mode of transmission, COVID-19 is treated under BSC level-2 due to its severity of Laboratory Associated Infections (LAIs) rate. For virus culturing, BSL-3 is recommended as aerial transmission of COVID-19 virus is the major risk of spread [71]. To ensure the safe handling, arrange the equipment precisely to minimize the hands and arms movement. Sealed-rooter centrifuge should be used for centrifugations purpose along with double gloves, N95 masks or powered air purifying respirators, face and eye protection [33]. Splash shield may be considered as a physical barrier. For isolation and viral characterization, BSL-3 laboratory is compulsory along with the proper use of PPE for safe handling. In case of spillage, use hypochlorite 1% solution (10,000ppm) for disinfecting the surfaces [72,73].
Conclusion
Because of the novelty of human coronavirus, no clear-cut solution can be reported yet as it requires huge research work. To compact the disease, prevention is the only best solution. Under this pandemic situation, ensuring the protective measures is the safest way against the human damage and transmission. But the increased requirement of PPEs resulted in their global shortage. To overcome the current health crises, along with the preventive measures, following reconditions should be considered:Recommendations
To optimize the PPEs availability for HCW’s protection, here are some recommendations for minimizing the risk of spared economically.
▪ To overcome the global shortage of PPEs, minimizing its need is a prominent factor in resolving the issue. For this purpose, use electronic mediums like video calling for initial examination of suspected cases. It will also reduce the personal exposure and risk factor.
▪ Glassware or plastic windows should implemented for triage which can easily be disinfect and provides a physical protective barrier within a hospital’s premises and pharmacy windows.
▪ Visitors should be connected to their patient via some means of telecommunication so that there will be no need to provide them the PPEs.
▪ Restrict the number of workers and specify the HCWs to monitors the COVID-19 patients which will make sure the longer use of PPEs.
▪ Use PPEs specifically such as during visual checkups, medical mask and face shield is enough, gloves or gown over the scrub suit is not necessary in that case while maintain the recommending distance.
▪ UV-C light is effective in sterilizing the N-95 masks so that paramedical staff can use it longer.
▪ Hand hygiene should be ensured timely, proper hand washing should be preferred over the use of hand sanitizers to cut the cost.
▪ Decontaminate the graywater of COVID-19 confirmed patients and PPEs used in their treatment with 0.5% sodium hypochlorite solution.
▪ The CDC devised an Al-based medical screening technique which actually monitors the respiratory blockage. It helped in scanning of suspected individuals more safely and quickly.
▪ Psychologists must be subjected to the isolations wards to cope with the metal stress conditions of COVID-19 patients.
References
- Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J Adva Res 2020; 24: 91-98.
- Shereen MA, Kazmi A. SARS-CoV-2 pandemic: Causes and current situation, historical lessons, and strategical therapeutic interventions. Biomed Res Ther 2020; 7: 3807-3812.
- Shereen MA, Ullah H, Khan S, Bashir N, Kazmi A, Saif K. COVID-19 around the world and the Chinese strategy to cope with SARS-CoV-2. Biomed Res Ther 2020; 7: 3890-3897.
- Worldometer. COVID19 Coronavirus Pandemic.
- Machida M, Nakamura I, Saito R, Nakaya T, Hanibuchi T, Takamiya T. Adoption of personal protective measures by ordinary citizens during the COVID-19 outbreak in Japan. Int J Infect Di 2020; 94: 139-144.
- Vuorinen V, Aarnio M, Alava M, Alopaeus V, Atanasova N, Auvinen M. Modelling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. Safety Sci 2020; 130: 104866.
- Aspland AM, Douagi I, Filby A, Jellison ER, Martinez L, Shinko D. Biosafety during a pandemic: shared resource laboratories rise to the challenge. Cytometry A 2021; 99: 68-80.
- Velavan TP, Meyer CG. The COVID‐19 epidemic. Trop Med Int Health 2020; 25: 278.
- Halfmann PJ, Hatta M, Chiba S, Maemura T, Fan S, Takeda M. Transmission of SARS-CoV-2 in domestic cats. N Engl J Med 2020; 383: 592-594.
- Zhou D, Zhang P, Bao C, Zhang Y, Zhu N. Emerging understanding of etiology and epidemiology of the novel coronavirus (COVID-19) infection in Wuhan, China. 2020.
- Li C, Ji F, Wang L, Wang L, Hao J, Dai M. Asymptomatic and human-to-human transmission of SARS-CoV-2 in a 2-family cluster, Xuzhou, China. Emerg Infect Dis 2020; 26: 1626-1628.
- Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat med 2020; 26: 450-452.
- Ari A. Promoting safe and effective use of aerosol devices in COVID-19: risks and suggestions for viral transmission. 2020.
- El-Wahab EWA, Eassa SM, Metwally M, Al-Hraishawi H, Omar SR. SARS-CoV-2 Transmission Channels: A Review of the Literature. MEDICC Rev 2020; 22: 51-69.
- El-Wahab EWA, Eassa SM, Metwally M, Al-Hraishawi H, Omar SR. SARS-CoV-2 Transmission Channels: A Review of the Literature. MEDICC Rev 2020; 22: 51-69.
- Jeong H, Yim HW, Song YJ, Ki M, Min JA, Cho J. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016; 38.
- Khan S, Siddique R, Li H, Ali A, Shereen MA, Bashir N. Impact of coronavirus outbreak on psychological health. J Glob health 2020; 10 : 010331.
- Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. 2019.
- Reiche EMV, Nunes SOV, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol 2004; 5: 617-625.
- Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med 1991; 325: 606-612.
- Campos-Rodríguez R, Godínez-Victoria M, Abarca-Rojano E, Pacheco-Yepez J, Reyna-Garfias H, Barbosa-Cabrera RE. Stress modulates intestinal secretory immunoglobulin A. Front Integr Neurosci 2013; 7: 86.
- Artika IM, Ma'roef CN. Laboratory biosafety for handling emerging viruses. Asian Pac J Trop biomed 2017; 7: 483-491.
- Alluwaimi AM, Alshubaith IH, Al-Ali AM, Abohelaika S. The Coronaviruses of Animals and Birds: Their Zoonosis, Vaccines, and Models for SARS-CoV and SARS-CoV2. Front vet sci 2020; 7: 655.
- Lam TTY, Jia N, Zhang YW, Shum MHH, Jiang JF, Zhu HC. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 2020; 583: 282-285.
- Georges JL, Gilles F, Cochet H, Bertrand A, De Tournemire M, Monguillon V. Positive association of angiotensin II receptor blockers, not angiotensin-converting enzyme inhibitors, with an increased vulnerability to SARS-CoV-2 infection in patients hospitalized for suspected COVID-19 pneumonia. PloS one. 2020; 15: e0244349.
- Mendoza EJ, Manguiat K, Wood H, Drebot M. Two detailed plaque assay protocols for the quantification of infectious SARS‐CoV‐2. Curr Protoc Microbiol 2020; 57: cpmc105.
- Bhullar MS. Application of Low Wave-length UV Irradiation to Inactivate Pathogenic Microbes in Highly Opaque Liquid Foods. 2016.
- Foladori P, Cutrupi F, Segata N, Manara S, Pinto F, Malpei F. SARS-CoV-2 from faeces to wastewater treatment: what do we know? A review. Sci Total Environ 2020; 743: 140444.
- Dinnes J, Deeks JJ, Adriano A, Berhane S, Davenport C, Dittrich S. Rapid, point‐of‐care antigen and molecular‐based tests for diagnosis of SARS‐CoV‐2 infection. Cochrane Database Syst Rev 2020 .
- Etherington MB. Investigative primary science: A problem-based learning approach. Aus J Teach Edu (Online) 2011; 36: 53.
- Novel CPERE. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua liu xing bing xue za zhi 2020; 41: 145-151.
- Khan S, Siddique R, Li H, Ali A, Shereen MA, Bashir N. Impact of coronavirus outbreak on psychological health. J Glob health 2020; 10 : 010331.
- Organization WH. Rational use of personal protective equipment for COVID-19 and considerations during severe shortages: interim guidance, 23 December 2020. World Health Organization, 2020.
- Taylor S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. 2019.
- Reiche EMV, Nunes SOV, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol 2004; 5: 617-625.
- Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med 1991; 325: 606-612.
- Campos-Rodríguez R, Godínez-Victoria M, Abarca-Rojano E, Pacheco-Yepez J, Reyna-Garfias H, Barbosa-Cabrera RE. Stress modulates intestinal secretory immunoglobulin A. Front Integr Neurosci 2013; 7: 86.
- Artika IM, Ma'roef CN. Laboratory biosafety for handling emerging viruses. Asian Pac J Trop biomed 2017; 7: 483-491.
- Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, van der Westhuizen HM. Face masks against COVID-19: an evidence review. 2020.
- Lam TTY, Jia N, Zhang YW, Shum MHH, Jiang JF, Zhu HC. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 2020; 583: 282-285.
- Georges JL, Gilles F, Cochet H, Bertrand A, De Tournemire M, Monguillon V. Positive association of angiotensin II receptor blockers, not angiotensin-converting enzyme inhibitors, with an increased vulnerability to SARS-CoV-2 infection in patients hospitalized for suspected COVID-19 pneumonia. PloS one. 2020; 15: e0244349.
- Mendoza EJ, Manguiat K, Wood H, Drebot M. Two detailed plaque assay protocols for the quantification of infectious SARS‐CoV‐2. Curr Protoc Microbiol 2020; 57: cpmc105.
- Organization WH. Risk communication and community engagement readiness and response to coronavirus disease (COVID-19): interim guidance, 19 March 2020. World Health Organization, 2020.
- Bhullar MS. Application of Low Wave-length UV Irradiation to Inactivate Pathogenic Microbes in Highly Opaque Liquid Foods. 2016.
- Foladori P, Cutrupi F, Segata N, Manara S, Pinto F, Malpei F. SARS-CoV-2 from faeces to wastewater treatment: what do we know? A review. Sci Total Environ 2020; 743: 140444.
- Dinnes J, Deeks JJ, Adriano A, Berhane S, Davenport C, Dittrich S. Rapid, point‐of‐care antigen and molecular‐based tests for diagnosis of SARS‐CoV‐2 infection. Cochrane Database Syst Rev 2020 .
- Organization WH. Guide for clinical case management and infection prevention and control during a measles outbreak. 2020.
- Etherington MB. Investigative primary science: A problem-based learning approach. Aus J Teach Edu (Online) 2011; 36: 53.
- Kazmi A, Kazmi A, Shams S, Sajid A, Khan K. Therapeutic role of bone marrow-derived stem cells and zinc sulfate for reduction of liver fibrosis. Progress Stem Cell 2019; 6: 269-278.
- Bain W, Lee JS, Watson AM, Stitt‐Fischer MS. Practical Guidelines for Collection, Manipulation and Inactivation of SARS‐CoV‐2 and COVID‐19 Clinical Specimens. Curr Protoc Cytom 2020; 93: e77.
- Godoy LRG, Jones AE, Anderson TN, Fisher CL, Seeley KM, Beeson EA. Facial protection for healthcare workers during pandemics: a scoping review. BMJ Glob Health 2020; 5: e002553.
- Lee C, Thampi S, Lewin B, Lim T, Rippin B, Wong W. Battling COVID‐19: critical care and peri‐operative healthcare resource management strategies in a tertiary academic medical centre in Singapore. Anaesth 2020; 75: 861-871.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaest/J canadien d'anesthésie 2020; 67: 568-576.
- Nath ND, Behzadan AH, Paal SG. Deep learning for site safety: Real-time detection of personal protective equipment. Automation in Construction 2020; 112: 103085.
- Poller B, Hall S, Bailey C, Gregory S, Clark R, Roberts P. ‘VIOLET’: a fluorescence-based simulation exercise for training healthcare workers in the use of personal protective equipment. J Hosp Infec 2018; 99: 229-235.
- Silva ALP, Prata JC, Walker TR, Duarte AC, Ouyang W, Barcelò D. Increased plastic pollution due to COVID-19 pandemic: Challenges and recommendations. Chem Engi J 2020: 126683.
- Nuccetelli M, Pieri M, Grelli S, Ciotti M, Miano R, Andreoni M. SARS-CoV-2 infection serology: a useful tool to overcome lockdown? Cell Death Disc 2020; 6: 1-9.
- Organization WH. Infection prevention and control of epidemic-and pandemic-prone acute respiratory infections in health care: World Health Organization; 2014.
- Pan Y, Li X, Yang G, Fan J, Tang Y, Zhao J. Serological immunochromatographic approach in diagnosis with SARS-CoV-2 infected COVID-19 patients. J Infect 2020; 81: e28-e32.
- Song P, Karako T. COVID-19: Real-time dissemination of scientific information to fight a public health emergency of international concern. Biosc Trends 2020; 14: 1-2.
- Possamai M. A time of fear: How Canada failed our health care workers and mismanaged Covid-19: Canadian Federation of Nurses Unions; 2020.
- Organization WH. Laboratory biosafety manual: World Health Organization; 2020.
- Karim N, Afroj S, Lloyd K, Oaten LC, Andreeva DV, Carr C. Sustainable personal protective clothing for healthcare applications: a review. ACS nano 2020; 14: 12313-12340.
- Ayowole D, Ogbonna V, Amoo A, Babarinde T, Nwafor J, Enebeli U. COVID-19 at the community level: What are the countermeasures? Nig J Med 2020; 29: 362-368.
- Christopher DJ, Isaac BT, Rupali P, Thangakunam B. Health-care preparedness and health-care worker protection in COVID-19 pandemic. Lung India 2020; 37: 238-245.
- Jensen PA, Lambert LA, Iademarco MF, Ridzon R. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. 2005.
- Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev 2020; 4: CD013582.
- Chavez S, Long B, Koyfman A, Liang SY. Coronavirus Disease (COVID-19): A primer for emergency physicians. Am J Emerg Med 2020.
- Wee LE, Fua TP, Chua YY, Ho AF, Sim XY, Conceicao EP. Containing COVID‐19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med 2020; 27: 379-387.
- Bahl P, Doolan C, De Silva C, Chughtai AA, Bourouiba L, MacIntyre CR. Airborne or droplet precautions for health workers treating COVID-19? J Infect Dis 2020.
- Huy MDN, My NN, Minh HD, Hoa TN, Phuong TDT, Ty HVT. Preventing laboratory-associated infections in the COVID-19 era: experience from a tertiary care infectious disease hospital in Southern Vietnam. 2020.
- Boškoski I, Gallo C, Wallace MB, Costamagna G. COVID-19 pandemic and personal protective equipment shortage: protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointest Endosc 2020; 92: 519-523.
- Thunstrom L, Newbold SC, Finnoff D, Ashworth M, Shogren JF. The benefits and costs of using social distancing to flatten the curve for COVID-19. J Benefit-Cost Analy 2020; 11:179-195.