ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2016) Volume 27, Issue 4
Protection of privacy and confidentiality as a patient right: physicians' and nurses' viewpoints
Nilüfer Demirsoy* and Nurdan Kirimlioglu
Department of History of Medicine and Medical Ethics, Faculty of Medicine, Eskisehir Osmangazi University, Eskisehir, Turkey
- *Corresponding Author:
- Nilüfer Demirsoy
Department of History of Medicine and Medical Ethics, Faculty of Medicine, Eskisehir Osmangazi University, Eskisehir, Turkey
Accepted on May 04, 2016
The purpose of patient rights, as a basic component of human rights, is to support patients and to strengthen them in social terms. The right to privacy and confidentiality, initially dealt with as a part of personal rights, has become a right in its own way over time, and is now recognized and guaranteed by many constitutions, laws, and international conventions. A cross-sectional survey was conducted on health care professionals at the Training and Research Hospital of the Faculty of Medicine of Eskisehir Osmangazi University in Eski?ehir, Turkey, in April, May and June in 2010 with the aim of determining health care professionals' (physicians' and nurses') attitudes towards the right to privacy and confidentiality of private life, which are important components of patient rights. The research data were collected through a questionnaire. The sample of the study consists of 174 nurses and 183 physicians. In this sample, 71 (40.8%) nurses and 49 (26.8%) physicians reported that they were informed about patient rights. 112 (64.4%) nurses and 103 (56.3%) physicians strongly agreed with the protection of privacy, and 90 (51.7%) nurses and 97 (53%) physicians strongly agreed with the confidentiality of information related to patients, as a patient right. Therefore, with a view to protecting and implementing patient rights, it is required to inform and raise awareness of health care professionals about patient rights, legal responsibilities of patients and health care professionals, and communication techniques.
Keywords
Physicians, Nurses, Confidentiality, Patient rights.
Background
Patient rights has been discussed as a part of the concept of human rights since the adoption of the universal declaration of human rights [1,2]. The fundamental aim of patient rights is to support patients and strengthen them in social terms [3]. Main patient rights involve respect for human dignity, receiving high-quality health services, right to being informed, prior consent of patient to medical interventions, respect for privacy and private life and sustainability of care and treatment [1,2].
As technological developments make it easier to intervene in individuals' private life, the demand for the protection of privacy increases and differentiates. This demand affects the provision of health care services and brings about new practices. This causes new discussions in the field of medical ethics and health law with regard to guaranteeing the right to privacy of individuals benefiting from health care services. The discussion and suggestions related to legal and ethical aspects of the right to privacy in health care services are of particular importance for the protection and maintenance of this right [3].
The Concept of Privacy
The concept of privacy originates from "privatus" and "privo" in latin and means "deprive of". The root of privacy is "priv", which means "an opportunity in one's favor" [4]. Privacy was used to refer to a private issue in 1590s, isolation as from 1600s and restriction on freedom in 1814 [5].
The concept of privacy does not have a widely accepted definition. It is usually accepted as a fundamental human need and a human right [6].
Privacy has been defined as the control of a situation, freedom of choice, mutual interaction, avoidance of communication and an unreachable area. Additionally, privacy may be defined as a restriction put by an individual on access to his/her bodily and mental integrity [7].
Privacy, besides being a fundamental quality of human beings and bearing an essential value in its own right, is an instrumental 'good' that enable individuals to achieve other good values. In Kant's theory, autonomy is a fundamental value of being a human. If privacy constitutes an essential to autonomy and autonomy cannot be understood without privacy, then losing privacy poses a threat to our most fundamental values [8].
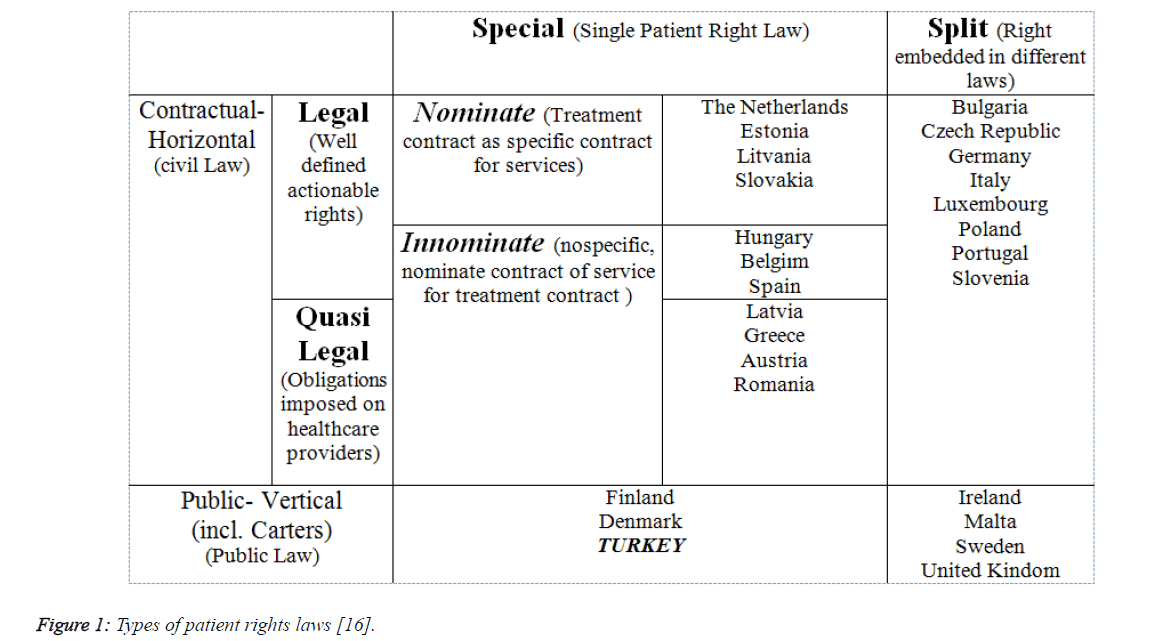
Figure 1: Types of patient rights laws [16].
The Right to Privacy
Private life or privacy generally refers to a sphere where individuals can remain on their own, think and behave as they like, and decide themselves personally where, when and under which conditions to communicate and have a relationship with others, as well as the right to control this sphere [9].
The right to privacy was first introduced by Warren and Brandie in 1890, who considered privacy equal to the right of an individual to be left on their own [10]. Warren and Brandie argued that general law guarantees individuals' right to determine to which extent they communicate feelings and ideas to others [4]. The right to privacy characterized by the right to self-determination provides individuals with moral authority about their personal characteristics.
Privacy is the right to autonomy and comprises the right to be left alone. It provides individuals with the right to control the information related to them, including the restriction of access to this information. It also involves the right to keep secrets confidential and to share them only in private conversations [11].
Patients' Right to Privacy
A patient's right to privacy involves the confidentiality of information related to the patient and bodily privacy of the patient [7,12,13]. From a historical perspective, an overview of legal instruments related to patient rights show that privacy and confidentiality of private life were involved in all relevant instruments (i.e. American Hospital Association's Patient's Bill of Rights 1972, World Medical Association's Declaration of Lisbon on the Rights of the Patient 1981, Amsterdam Declaration on the Promotion of Patients' Rights in Europe 1994, Bali Declaration 1995, European Charter of Patients' Rights 2002).
Confidentiality and privacy are vital for establishing and maintaining an effective and respectful clinical relationship. The right to privacy constitutes a social merit as it encourages the explicit discussion of health-related problems between clinicians and patients. Privacy requires physicians to keep confidential information that patients provide or they obtain in their professional interaction with patients [14].
Privacy is important as it provides a secure environment for patients where they receive medical care and provide complete and accurate information, and which reinforces confidence in health care and emphasizes the importance of respect for patient autonomy [15].
Patient Rights and Privacy in Turkey and the European Countries
Patient rights are being debated in an intensive manner, both at the national and international level. Many countries have added patient rights to the legislation related to health. The rights concerning health are generally structured in the constitutions or principal legislations of countries. While some European countries have reviewed and updated their existing laws related to patient rights, some other countries have passed new laws.
The European Patient Rights Charter (2003), which was prepared in the context of the Constitution of the European Union and the protocols connected to it, and which aims for harmony in terms of patient rights in Europe, includes both additional new rights on top of the patient rights contained in the previous documents, and explanatory information related to the scope and content of all patient rights. The content of this Charter was adopted by the European Countries a short time after the Charter was published. Following the publication of the Charter, the Ministry of Health in Turkey also benefited from this Charter in its activities related to patient rights, and in fact shared the translation of the Charter on its official website. The European Charter of Patient Rights which is the most important document in respect of patient rights contains many concepts concerning bio-ethics, medical ethics and medical legislation. The EU Charter of Patient Rights was prepared by taking into account the content of the documents published by the WHO and the European Union on patient rights, the illustrative actions and attitudes of health professionals and the parameters related to the services. The objectives of the document were that the rights of individuals are ensured and not violated when they benefit from health services, ensuring that there is harmony between the European countries in the context of respect to patient rights and the prevention of violations which may arise from the national health system.
| European Countries | The Legal Status in Respect of Patient rights | References to the Matters of Privacy and Confidentiality in their Legislation |
|---|---|---|
| Denmark | There are numerous articles concerning patient rights in their principal legal system. The patient rights legislation also came into effect in 1998. | |
| Finland | The first European country which passed a law giving rights to patients (1 March 1993). | Sanctions ensuring that the patients are provided assurance in terms of the confidentiality of information and the protection of secrets, and resulting in penalty in the event of violations, have been put in place. |
| Greece | Patient rights were taken into account with the Codes of Medical Practice, published in 1939 and the Codes of Conduct published in 1995. | |
| Iceland | The Patient Rights Legislation dated 17 May 1997. | It is emphasized that a private relationship exists between the patient and the health worker, and that this needs to be protected. |
| Italy | Patient rights have been regulated under the Codes of Medical Ethics in Italy. However, the codes are not legislative and only give examples and recommendations. | Emphasizes the privacy of confidential information. |
| The Netherlands | The Medical Contracts Legislation was passed in 1995. | Contains provisions related to consent, access to medical data and privacy. |
| France | Provisions related to patient rights have been included in different laws. The law entitled patient rights and the nature of the health system came into effect in March 2002. | Contains legal regulations concerning the confidentiality of records. |
| Portugal 1968, 1989, 1993 (new regulations were put on the agenda of the Ministry) | The Government has published Patient Rights Regulations. | |
| Ireland (1995) | The right to privacy / maintaining the confidentiality of hospital records in full, especially under circumstances where the nature of the clinical status of the patient is subject to debate. | |
| Portugal (1997) | The right to the protection of personal privacy. | |
| Lithuania 1996 | ||
| The United Kingdom (1991) (1995 revised) | Has been dealt with under the title of “Respecting Privacy”. | |
| Turkey 1998-(2014 revised) | ||
| Georgia-health services legislation in 1997 and patient rights regulations in 2000 | ||
| Israel 1 May 1996 | ||
| Norway 1999 | ||
| Austria | Regulations on Patient Rights have been added to the regulations governing the health sector, with different laws. | The Right to a Private Life (consists of strong provisions directed at respecting the privacy, personal data and consent of the patient). |
| Bulgaria | Public health legislation. | |
| Czech Republic | Consent to or refusing the participation of medical students in treatment procedures and respecting privacy. | |
| France (2002-revised) | The Patient Rights Clearly Set Out in the Public Services Legislations and Public Regulations. | |
| Slovakia | ||
| Slovenia (2008) | ||
| Spain 1986-2003 (revised) | ||
| Uzbekistan | ||
| Romania 1978 | ||
| Hungary 1997 | ||
| Poland | ||
| Sweden (1999) | ||
| Hungary |
Table 1: The Legal Status in Respect of the Rights and Privacy and Confidentiality of the Patients in Certain European Countries [17].
Article 6
Right to privacy and confidentiality: Every individual has the right to the confidentiality of personal information, including information regarding his or her state of health and potential diagnostic or therapeutic procedures, as well as the protection of his or her privacy during the performance of diagnostic exams, specialist visits, and medical/surgical treatments in general. All the data and information relative to an individual's state of health, and to the medical/surgical treatments to which he or she is subjected, must be considered private, and as such, adequately protected. Personal privacy must be respected, even in the course of medical/surgical treatments (diagnostic exams, specialist visits, medications, etc.), which must take place in an appropriate environment and in the presence of only those who absolutely need to be there (unless the patient has explicitly given consent or made a request) [18].
The rules of the European guidelines concerning confidentiality and privacy for health workers in health services (May 2006): The right to privacy of each patient and the obligation of privacy of each health worker, are independent of the manner in which this information is stored or transmitted (e.g. in the form of electronic photographs or biological samples). These guidelines are valid for all health workers and are addressed at the fields of privacy and the confidentiality of information in health services. The guidelines are a part of the European Standards Concerning Confidentiality and Privacy in the Provision of Health Services, and these standards explain the Guidelines in more detail, and present recommendations to the organizations which provide health services within the framework of the ethical and legal foundations [18].
Patient Rights and Privacy in Turkey
In Turkey, "The Patient Rights Regulation" drafted by the Ministry of Health was adopted on August 1, 1998 [19]. The Regulation was revised on May 8, 2014 by the Regulation Amending the Patient Rights Regulation no. 23420 [20]. The sub-heading of the respect for privacy in the Patient rights Regulations, which were updated in 2014, has been maintained in full, in its former state.
The fourth part of the Patient Rights Regulation, titled "Protection of Patient Rights", deals with the confidentiality of information related to patients and protection of bodily privacy under the title of respect for privacy, and explains as follows the scope of respect for privacy and the right to demand privacy. In this respect, it is required:
• to keep confidential any medical evaluation related to the health condition of patients,
• to protect confidentiality, to the reasonable extent, in examination, diagnosis, treatment and other procedures that require direct contact with patients,
• to let the patient be accompanied by another person in cases where there is no medical disadvantage,
• not to let the presence of people in the medical intervention who are not directly related to the treatment,
• not to intervene in personal and family life of the patient unless the nature of disease requires,
• to keep confidential, the funding of health care costs. It is clearly indicated that the death of a patient does not allow the violation of the right to privacy.
The final provision of the fourth part stipulates the obligation to keep confidential the information obtained during the provision of health care services.
The regulation further includes the statement that "information is obtained in a suitable environment where the patient's privacy is protected" [20].
Methods
Patients' knowledge and willingness are important in the use and protection of these rights appropriately. Because patients usually do not know their rights, they need a guide who will inform them about how to acquire and use these rights. That is why physicians' and nurses' viewpoints about patient rights and how they reflect these viewpoints on their behaviors are important.
This study was conducted in the Training and Research Hospital of Eskişehir Osmangazi University in order to determine health care professionals' (physicians' and nurses') attitudes towards the right to privacy and confidentiality of private life, which are important components of patient rights.
Before the data were collected, permission was granted from research and ethics board. Health care professionals were informed about the aim and content of the study, and volunteering professionals were included in the study. The research data were collected through a questionnaire.
In the questionnaire form:
Part I sought information about the age, sex, title, department and the the years of experience;
Part II asked whether the participants were informed about patient rights and the presence of a unit responsible for patient rights;
Part III, based on "The Patient Rights Regulation", included 26 statements for the purpose of determining patients' and health care professionals' attitudes towards patient rights. The following choices were available for each statement: strongly disagree, disagree, neutral agree and strongly agree. On the other hand, the data used in the study covers an evaluation of the clauses which consist of the right to privacy contained in this questionnaire.
The questions used in the data analysis
Part II
10. Do you know your patient rights? ( ) 1. Yes ( ) Partially ( ) 2. No
11. If yes, where did you learn them?
12. Is there any committee which protects Patient Rights at our hospital?
( ) 1. Yes
( ) 2. No. Is there a requirement for one? ( ) Yes ( ) No
( ) 3. I don’t know
Part III
10. Patients have the right to request that their privacy is protected while their examinations and treatment procedures are being implemented.
11. Patients have the right to demand the confidentiality of information related to their health condition, diagnosis, prognosis and treatment as well as all other personal information
In data analysis, arithmetic mean, standard deviation, frequency and percentages were used to describe the participants' replies with regard to research variables, in consideration of measurement level of the variables.
It was considered whether there is a statistical relationship between the demographic characteristics of participants and research variables. Chi-square (χ2) test was used to determine the difference and relationship between the groups of physicians and nurses with regard to variables, and t-test was used to define the differences between the groups of physicians and nurses. The present paper offers the significant relationships and differences found as a result of the analyses. On the other hand, regression analysis was used in order to determine the factors which influence the perception of privacy. The statistical software SPSS 21.0 was used for the analysis of data.
On limitation of the study
The information concerning patient rights was evaluated in line with the responses given by individuals to the questions in the questionnaire. The very busy working conditions in the departments and the wishes of certain hospital workers about not to implement the questionnaire due to the intensity of their work were the difficulties faced during the implementation of the questionnaire. The questions used in the study were prepared by the researchers in line with the relevant literature, and this, together with the responses given by the participants and the fact that the study was only performed on the doctors and nurses employed at one hospital in Eskişehir are the limitations on the generalization of the study.
Results
In the group of nurses, 128 (73.6%) of them work in clinics, 21 (12.1%) work in outpatient clinics, 20 (11.5%) are head nurses and 5 (2.9%) are supervisor nurses. In the group of physicians, 126 (68.9%) are residents, 38 (20.8) are specialists, 15 (8.2%) are academics and 4 (2.2%) are family physicians (Table 2).
| Descriptive Characteristics of Nurses and Physicians | Hemşire | Hekim | |||
|---|---|---|---|---|---|
| Sex | n | % | n | % | |
| Women | 160 | 92 | 74 | 40.4 | |
| Men | 14 | 8 | 109 | 59.6 | |
| Age | 36.00 ± 5.83131 | 4200 ± 9.69247 | |||
| Age group (nurse) | Age group (physician) | n | % | n | % |
| 20-26 | 24-29 | 38 | 21.8 | 70 | 38.3 |
| 27-33 | 30-36 | 83 | 47.7 | 68 | 37.2 |
| 34-40 | 37-43 | 44 | 25.3 | 17 | 9.3 |
| 41 and over | 44 and over | 9 | 5.2 | 28 | 15.3 |
| Clinic | n | % | n | % | |
| Internal | 97 | 55.7 | 88 | 48.1 | |
| Surgical | 77 | 44.3 | 95 | 51.9 | |
| Length of experience (years) | n | % | n | % | |
| 0-1 | 18 | 10.3 | 54 | 29.5 | |
| 1-5 | 64 | 36.8 | 84 | 45.8 | |
| 6-10 | 31 | 17.8 | 12 | 6.6 | |
| 11-15 | 30 | 17.2 | 6 | 3.3 | |
| 16 and over | 31 | 17.8 | 27 | 14.8 | |
Table 2: Descriptive characteristics of nurses and physicians.
71 (40.8%) nurses and 49 (26.8%) physicians reported they knew patient rights, 98 (56.3%) nurses and 119 physicians (65%) reported they partially knew patient rights, and 5 nurses (2.9%) and 15 physicians (8.2%) reported they did not know patient rights.
70 (40.2%) nurses and 91 (49.7%) physicians reported that there is a patient rights unit, 97 (55.7%) nurses and 26 (14.2%) physicians reported that there is not a patient rights unit, and 7 (4%) nurses and 66 (36.1%) physicians reported that there should be a patient right unit in the hospital.
With the statement that "patients have the right to demand the protection of privacy in the provision of care and treatment", 112 (64.4%) nurses strongly agreed, 61 (35.1%) agreed and 1 (0.6%) disagreed; and 103 (56.3%) physicians strongly agreed, 71 (38.8%) agreed, 4 (2.2%) were undecided and 5 (2.6%) disagreed.
With the statement that "patients have the right to demand the confidentiality of information related to their health condition, diagnosis, prognosis and treatment as well as all other personal information", 90 (51.7%) nurses strongly agreed, 81 (46.6%) nurses agreed, 2 (1.1%) nurses were undecided and 1 (0.6%) nurse disagreed; and 97 (53%) physicians strongly agreed, 76 (41.5%) physicians agreed, 4 (2.2%) physicians were undecided and 6 (3.3%) physicians disagreed.
There is a significant relationship, in the case of nurses, between knowing that there is a patient rights unit in the hospital and being informed about patient rights. The majority of nurses having told that there was no patient rights unit in the hospital reported that they partially knew patient rights. This suggests that they were not informed enough about patient rights and the protection of such rights. Furthermore, over half of nurses that were informed about patient rights also knew the presence of a patient rights unit in the hospital. (χ2=29.042, df=4, p=0.000, p<0.05).
There is a statistically significant relationship, in the case of physicians, between knowing that there is a patient rights unit in the hospital and agreeing that patients have the right to demand the confidentiality of information related to their health condition, diagnosis, prognosis and treatment as well as all other personal information. Physicians knowing that there is a patient rights unit in the hospital agree more than physicians not knowing the presence of such a unit with patients' right to demand the confidentiality of all their information. (χ2=17.953, df=6, p=0.006, p<0.05).
There is a statistically significant relationship, in the case of physicians, between the length of experience and agreement with patients' right to demand the protection of privacy during care and treatment provision. The physicians working for 1 to 5 years agree more with patients' right to demand the protection of privacy in the provision of care and treatment compared to the other physicians. (χ2=26.318 df=16, p=0.05, p ≤ 0.05).
There is a significant relationship, in the case of physicians, between knowing that there is a patient rights unit in the hospital and being informed about patient rights. Almost all physicians who mentioned they knew patient rights were also informed that there is a patient rights unit in the hospital. (χ2=23.624, df=4, p=0.000, p<0.05).
Knowing patient rights in force and knowing the presence of patient rights cause a significant difference in physician and nurse groups with respect to agreement with patients' right to demand the protection of their privacy in care and treatment and their right to demand the confidentiality of information related to health condition, diagnosis, prognosis and treatment as well as all other personal information. The difference is in favor of physicians (Table 3).
| Levene's Test for the Homogeneity of Variances | t-test | ||||
|---|---|---|---|---|---|
| F | p | t | df | ||
| Knowing patient rights | Physicians | 5.39 | 0.021* | 3.304 | 355 |
| Nurses | 3.307 | 354.93 | |||
| Knowing the presence of a patient rights unit | Physicians | 139.876 | 0.000* | 2.783 | 355 |
| Nurses | 2.816 | 303.222 | |||
| Patients' right to demand the protection of privacy | Physicians | 12.512 | 0.000* | 2.27 | 354 |
| Nurses | 2.286 | 330.719 | |||
| Patients' right to demand the confidentiality of information | Physicians | 4.662 | 0.032* | 0.769 | 355 |
| Nurses | 0.774 | 344.254 | |||
| *p<0.05 | |||||
Table 3: t-test results concerning the comparison of physician and nurse groups' replies to questions on patient rights and privacy.
A multi-variable regression analysis was performed in order to evaluate the roles of the factors, but no significant results could be reached. The results we obtained through the regression analysis are as follows:
The regression analysis of the responses given by doctors to the statement, “Patients have the right to demand that their privacy is protected while their examinations and treatment procedures are being implemented”, and the factors which influence these: age (t= -0.971, Sig. 0.333), gender (t= 0.693, Sig. ,0.489), title (t= -1.019, Sig. 0.310), clinic employed at (t= -0.016, Sig. 0.987), number of years employed (t=0.797, Sig. 0.426).
The regression analysis of the responses given by doctors to the statement, “Patients have the right to demand the confidentiality of information related to their health condition, diagnosis, prognosis and treatment as well as all other personal information.”, and the factors which influence these: age (t= -0.558, Sig. 0.579), gender (t=1.380, Sig. 0.169), title (t= -0.322, Sig. 0.748), clinic employed at (t=0.442, Sig. 0.659), number of years employed (t=0.513, Sig. 0.608).
The regression analysis of the responses given by nurses to the statement, “Patients have the right to request that their privacy is protected while their examinations and treatment procedures are being implemented”, and the factors which influence these: age (t=1.085, Sig. 0.279), gender (t=0.443, Sig. 0.658), title (t=1.078, Sig. 0.283), clinic employed at (t=1.530, Sig. 0.128), number of years employed (t=0.083, Sig. 0.934).
The regression analysis of the responses given by nurses to the statement, “Patients have the right to demand the confidentiality of information related to their health condition, diagnosis, prognosis and treatment as well as all other personal information.”, and the factors which influence these: age (t=1.273, Sig. 0.205), gender (t= -1.499, Sig. 0.136), title (t=1.419, Sig. 0.158), clinic employed at (t=1.235, Sig. 0.219), number of years employed (t= -0.167, Sig. 0.868).
Discussion
Emphasis on patient rights in the health care services particularly maintains patient dignity as a rank of a human, and is considered as important especially when patient's vulnerability easily exposes him to the violations and weaknesses of the health care system.
Observing patients’ rights is the most important ethical issue in a hospital which should absolutely be considered. Regarding patients' rights and respecting them are two main factors for patients' care. It is important that medical staff pay enough attention to its various aspects. Observing patients’ rights means the accountability of all health care staff to the patients at the time of treatment and care giving [21].
Patient rights should be known by both professionals providing health care and patients receiving health care services and their relatives so that the quality of service offered and received can be improved. Legal instruments alone are not sufficient. What is important is to put these legal instruments into practice. That is why, all health care professionals, primarily physicians, are required to be informed, aware and practitioners of patient rights [22]. In order to ensure an integrated approach in the field of health, it is necessary for health workers to consciously reflect patient rights in their implementations. The needs of individuals should be met in the physical, mental, social, cultural, spiritual and intellectual dimensions within the integrated approach to health. The concept of patient rights deals with all of these needs in the legal dimension [23].
In some studies related to patient rights in both Turkey and the world [24-28], it has been demonstrated that health workers are aware of the relevant regulations concerning patient rights in their own countries to different degrees, and in the study of Kagoya et al., it was indicated that 69.4% of them had not heard about these at all [29].
In the present study, 71 (40.8%) nurses and 49 (26.8%) physicians reported that they knew patient rights and 98 (56.3%) nurses and 119 physicians (65%) reported that they partially knew patient rights while 5 (2.9%) nurses and 15 (8.2%) physicians reported that they were not informed about patient rights. This finding of our study does not support the above-mentioned studies that dealt with physicians separately, but provided results that are similar to the studies involving nurses. The comparison of our findings with above-mentioned studies conducted abroad suggests that health care professionals in Turkey are less informed about patient rights.
Özer and Günay found in their study that male physicians were more informed than female physicians about patient rights [25].
The present study did not provide any statistical difference between female and male physicians with regard to being informed about patient rights. However, it has been observed that a higher rate of male physicians knew patient rights compared to female physicians. This is probably related to the fact that the number of male physicians involved in this study was higher than the number of female physicians. That is why this finding of our study is considered inconsistent with the finding of Özer and Günay.
With the increasing interest in patient rights in the world and in Turkey, a regulation [19,20] and some instructions [30] were adopted in Turkey. Departments related to patient rights were established in hospitals in parallel with the putting into practice of the directives. The departments of patient rights are of much importance in terms of determining whether the services provided have reached the desired results and whether the needs of patients and their relatives have been met.
In our study, 70 of the nurses (40.2%) and 91 of the doctors (49.7%) stated that there was a patient rights department at the hospital they were employed at, 97 of the nurses (55.7%) and 26 of the doctors (14.2%) stated that there wasn’t, and 7 of the nurses (4%) and 66 of the doctors (36.1%) stated that there should be. This shows that they are aware of the patient rights department at higher rates than the other studies conducted in Turkey that we have been able to reach [31,32].
Physicians and nurses, as health care professionals, have primary responsibilities with regard to the protection of patient rights. Tappen, et al. stated that the Patient Rights Declaration of the American Hospitals Association had been presented with the expectation that patient care could be performed in a more effective manner, and that effective care for patients could be achieved thanks to the cooperation between the doctors and other health professionals [33]. Nurses seem to have more responsibilities since they spend more time with patients than physicians do, and patients mostly tend to feel closer to nurses [34].
In the present study, there is a significant relationship between being informed about the presence of a patient rights unit and knowing patient rights. The majority of nurses who said that there was no patient rights unit in the hospital reported that they partially knew patient rights. This suggests that they were not informed enough about patient rights and the protection of such rights. Furthermore, over half of the nurses that knew patient rights also knew the presence of a patient rights unit in the hospital. (χ2=29.041, df=4, p=0.000, p<0.05).
People that are informed about the privacy of others are expected to respect the privacy during and after a medical intervention. The source of this expectation is the relationship based on the confidence between patients and health care professionals [35]. The confidence derives from patients' belief that health care professionals do not share the information about patients they obtain during the provision of health services with others. Patients' right to the protection of privacy, included in the "confidentiality of private life"-one of the fundamental human rights, is one of the most important points to be considered in the provision of health care services.
Privacy, a concept with no specific definition, is affected by various perceptions. Patients', nurses' and physicians' knowledge and awareness of various aspects of this concept are likely to affect how they perceive privacy aspect of their practices. Furthermore, patients, nurses and physicians may have different perceptions of privacy because of differences in cultural and educational background as well as socialization processes [36].
Virginia Henderson has stated that the objective of the care professions is to make them independent in terms of meeting the fundamental needs of individuals. She argued that these fundamental needs are comprised of the physiological, psychological, sociological, spiritual and intellectual fields, and defined 14 principal needs [37]. When the right to privacy is evaluated within the general framework, it is included in all of these fundamental needs as an important element. The right to privacy of patients is not a new concept in nursing. The first principle taught to nurses is the need to protect the privacy of patients during their practices. However, this privacy is thought to be limited only to the use of curtains and screens. Curtains, screens and sheets only make the patient invisible and privacy consists of much more than this. As a fundamental need, privacy is the principal component of the right to autonomy.
Nursing is a patient-centered profession, which involves interventions that require being close to physical, psychological, social and personal information related to individuals. Among the responsibilities of nurses are to help patients get adapted to the hospital environment, to protect an individual's health as their proxy when required, to make them have control in their personal sphere, to ensure their comfort and to protect and maintain the protection of privacy and confidentiality of their physical, psychological, social and cognitive information related to patients in this new environment [36].
Despite the efforts of experts in the field of health to emphasize the privacy of privacy, there are not enough studies in this area, especially in the field of nursing [38,39]. The concept of privacy has been referred to for many years together with the regulations and new practices in the Turkish health system in the area of patient rights, but there have been no specific research on patient privacy.
In certain studies where the views of health workers on patient rights have been questioned-both in Turkey and throughout the world [13,22,25,28,38,40], while health workers have stated that patient privacy is important, and that it is supported at a high rate, in certain national studies [41,42], it has been stated that the treatment of the patient takes priority over their privacy.
In the present study, with the statement that "patients have the right to demand the protection of privacy in the provision of care and treatment", 112 (64.4%) nurses and 103 (56.3%) physicians strongly agreed, and 61 (35.1%) nurses agreed and 71 (38.8%) physicians agreed. Almost all of the health workers in our study were in agreement with the need for the protection of the privacy of patients. This clearly shows that they believe that the protection of the privacy of patients is just as important as their treatment.
Özay and Günay found in their study that as physicians' years of experience increases, they are more informed about patient rights [25].
There is a statistically significant relationship between physicians' years of experience and their agreement with patients' right to demand the protection of privacy. The physicians working for 1 to 5 years agree more with patients' right to demand the protection of privacy in the provision of care and treatment compared to the other physicians. (χ2=26.318, df=16, p=0.05, p ≤ 0.05) This finding in our study is not considered to support Özer and Günay's relevant finding.
Private life is known and shared by an individual's immediate vicinity in personal and professional life. Private law considers private life confidential and protects its confidentiality. Patients mostly provide information about their personal life and disease to the physician who they accept him/her as a close person. Physicians are required to keep such information confidential, complying with the principle of respect for confidentiality, which is an important medical ethics rule.
Physicians and nurses necessarily and naturally witness patients' bodies, moral defects and disabilities. They have to keep confidential the information related to their patients they obtain when fulfilling their profession. Disclosure of confidential information and observation is a violation of not only a patient's but also their relatives' personal rights, and physicians are required not to disclose confidential information related to their patients [43].
Information related to patients cannot be obtained and disclosed without their consent, and digital patient records can only be used by related people. Information related to patients cannot be exchanged in public spheres and in the presence of unrelated people [44].
Guaranteeing the respect for confidentiality of patients' private life enable them to provide more accurate information to health care professionals. This guarantee not only reinforces the confidence between patients and physicians but also contributes to the improvement of treatment practices. Besides, the physician contributes to the formation of a strong partnership and effective cooperation between nurses and patients as the administrators of the treatment. Furthermore, they motivate patients to establish a “partnership” with physicians and the administrators of the treatment, as a method of giving them the self-confidence and motivation to gradually make the behavioral changes which may affect their own health [45].
The Ethical Codes of Nursing of the International Council of Nursing recommends that nurses keep personal information confidential, and use their common sense at the point where they need to share this information (ICN, 2001). The principle of care referred to in the Nightingale Oath is confidentiality. The principle of confidentiality can only be questioned when faced with a circumstance where it is necessary to prevent damage to innocent individuals [46].
In certain studies conducted in Turkey and throughout the world [28,47-49] while it is stated that the confidentiality of the information belonging to patients is supported at a high rate, in a study which includes health workers in Britain, it was determined that the rate of participation and the level of awareness of health workers on the matter of confidentiality was low [13].
In our study, the responses given to the statement, “Patients have the right to demand the confidentiality of information related to their health condition, diagnosis, prognosis and treatment as well as all other personal information.”, were as follows: 90 of the nurses (51.7%) and 97 of the doctors (53%) were in full agreement; and 81 of the nurses (46.6%) and 76 of the doctors (41.5%) were in agreement. These responses show that almost all of the health workers agreed with the protection of the confidential information belonging to patients, as a right.
There is a statistically significant relationship, in the case of physicians, between knowing that there is a patient rights unit in the hospital and agreeing with patients' right to demand the confidentiality of information related to health condition, diagnosis, prognosis and treatment as well as all other personal information. Compared to the others, the physicians who were informed about the presence of such a unit were in much agreement with patients' right to demand the confidentiality of all information related to them (χ2=17.953, df=6, p=0.006, p<0.05).
Conclusion
Respect for patient privacy is a professional responsibility. Patients' right to privacy as a right recognized in international human rights conventions and protected in the national health legislation, is substantially known and supported by health care professionals that participated in our study.
Nurses are more informed than physicians about patient rights, and physicians are more informed than nurses about the presence of a patient rights unit in the hospital.
From the perspective of health care professionals, patients' privacy is as important as their treatment. However, the physicians with work experience of 1 to 5 years agree more with patients' right to the protection of privacy than others. Furthermore, nurses are in much agreement with patients' right to the protection of privacy than physicians.
Almost all health care professionals agree that the confidentiality of information related to patients is a right. The rate of agreement is greater among nurses than doctors.
The physicians who are informed that there is a patient rights unit in the hospital agree more with patients' right to demand the confidentiality of all their information than the physicians who are not informed about the presence of a such unit.
Training and guidance by health care professionals are required for the protection of patient rights. Furthermore, it is required to clearly define the responsibilities and status of patients and health care professionals. The reinforcement of the independence of people responsible for the use of patient rights and opportunities related to the fulfillment of these responsibilities will ensure the adoption of more positive approaches to patient rights in the society.
Privacy is not only a psychological need that is related to individuals. It is also a phenomenon that is closely and deeply related to social life. In this respect, it is important to lay a philosophical foundation regarding the respect for privacy and to perform best practices for each specific case. The sentiment of privacy should give patients the confidence that the disclosed information will not be revealed to other by any means and should encourage them for a true form of communication. As the patient will not be comfortable in an environment where there is no privacy and much of his/her personal information is disclosed to others, he/she may keep certain personal information as well as his/her demands a secret from health workers to a certain extent. For instance, patients need to be sure about that attention is paid to privacy when they disclose information to health workers or need recommendations on matters related to sexual problems, the use of medication for urinary infections, the use of rectal or intra-vaginal medication, physical examinations in the departments, etc. For health organizations which target quality services, the attitudes of health workers are among the essential factors in order to establish the legal and institutional regulations directed at patient rights in general, and the protection of privacy and confidentiality in particular, and ensure that these are operational.
Confidentiality of information is important in clinical practice in that it is a sign of respect for the patient and encourages the patient to provide personal information required to offer highquality health care service. Confidentiality of information, as an ethical issue, is primarily based on the principle of respect for autonomy. It is related to the person's body and extensions of information related to that person. Therefore, it is an ethical liability of clinicians to respect patients' decisions involving such information [50].
Nurses working closely with patients need to be informed and aware of individuals' rights and sensitive to the use of these rights in order to meet patients' needs, protect their prestige, honor and privacy while providing service and improve quality of service. Given the defensive role of nurses in the hospital and their functions falling within the scope of this role, there is a need for greater focus on patient rights in the orientation process and in-service trainings.
Therefore, with a view to protecting and implementing patient rights, it is required to inform and raise awareness of health care professionals about patient rights, legal responsibilities of patients and health care professionals and communication techniques. It will thus be possible to solve related problems, improve the quality of health services, provide health care services in line with human dignity and avoid the violation of patient rights.
The findings of this study concerning the confidentiality of the personal information of patients and the protection of their rights to privacy provide empirical data directed at the creation of an ethical environment for the future. Therefore, there is a need for similar studies and comparisons and for the results of these to be published.
References
- Elçioglu ÖS. Confidentiality in terms of patients rights. TurkiyeKlinikleri J Med Ethics 1997; 5:16-19.
- Ünsal A, Bulucu GD, Kura E, Ercan Y. The levels of knowledge concerning the rights of patients of patients receiving outpatient services. FiratSaglikHizmetleriDergisi 2011; 6: 27-40.
- Zaybak A, Eser I, Ismailoglu EG. An analysis of the attitude of patients towards using their patient rights at a university hospital. IÜFN Hem.Derg 2012; 20: 104-111.
- Leino-Kilpi H, Välimäki M, Dassen T, Gasull M, Lemonidou C, Scott A, Arndt M. Privacy: a review of the literature. Int J Nurs Stud 2001; 38: 663-671.
- www.etymonline.com.
- Heikkinen A, Wickström G, Leino-Kilpi H. Understanding privacy in occupational health services. Nurs Ethics 2006; 13: 515-530.
- Sert G. Medical ethics and the right of privacy. Istanbul: Babil Publications 2008.
- Dedeoglu G. Surveillance, privacy and human dignity. TBD BilisimDergisi 2004; 89.
- Yüksel M. The right of privacy and its socio-historical development. Ankara Üniversitesi SBF Dergisi 2003; 58: 181-213.
- Woogara J. Human rights and patients' privacy in UK hospitals. Nurs Ethics 2001; 8: 234-246.
- www.tbd.org.tr/usr_img/cd/kamubib12/raporlarPDF/RP2-2007.pdf/.
- Ocaktan E, Yildiz A, Özdemir O. Knowledge and attitudes of health care personel working at Abidinpasa Health Group Directorate. Ankara Üniversitesi Tip FakültesiMecmuasi 2004; 57: 129-137. Turkish.
- Woogara J. Patients' privacy of the person and human rights. Nurs Ethics 2005; 12: 273-287.
- J Braunack-Mayer AC, Mulligan E. Sharing patient information between professionals: confidentiality and ethics. MJA 2003; 178: 277-279.
- Beauchamp TL, J Childress JF. Principles of Biomedical Ethics. 6 ed. Oxford University Press 2009.
- http://europatientrights.eu/types/general_overview_of_types_of_legislation.html.
- Sert G. Patients' Rights: International Declarations and Medical Ethics BabilYayinlari-Istanbul; 2004.
- Emre Ö, Sert G. European Charter of Patients' Rights. Turkish Journal of Bioethics 2014; 1: 198-205.
- The Patient Rights Regulation. Official Gazette. Number: 23420.
- The Regulation Amending the Patient Rights Regulation. Official Gazette. Number: 28994.
- Mohammad Nejad E, Begjani J, Abotalebi G, Salari A, Ehsani SR. Nurses awareness of patients rights in a teaching hospital. J Med Ethics Hist Med 2011; 4: 2.
- Yürümez Y, Çevik T, Yavuz Y. Do we know the patient rights? AkademikAcil Tip Dergisi 2010; 9: 67-71.
- Demirsoy N, Degirmen N, Kirimlioglu N. The place and Importance of the concept of Holism in Health Service. TurkiyeKlinikleri J Med Ethics 2011; 19.
- Zincir H, Erten ZK. Knowledge levels of the health care employees working at the primary health institutions about patient rights. UluslararasiInsanBilimleriDergisi 2009; 6: 877-885.
- Özer A, Günay O. Knowledge levels of physicians working in Kayseri on patient rights. Erciyes Tip Dergisi 2007; 29: 56-63.
- Özdemir MH, Ergönen AT, Sönmez E, Can IÖ, Salaçin S. The approach taken by the physicians working at educational hospitals in Izmir towards patient rights. Patient Education and Counseling 2006; 61: 87-91.
- Ducinskiene D, Vladickiene J, Kalediene R, Haapala I. Awareness and practice of patient's rights law in Lithuania. BMC International Health and Human Rights 2006; 6: 10.
- Alghanim SA. Assessing knowledge of the patient bill of rights in central Saudi Arabia: a survey of primary health care providers and recipients. Ann Saudi Med 2012; 32: 151-155.
- Kagoya HR, Kibuule D, Mitonga-Kabwebwe H, Ekirapa-Kiracho E, Ssempebwa JC. Awareness of, responsiveness to and practice of patients' rights at Uganda's national referral hospital. Afr J Prim Health Care Fam Med 2013; 5: 491.
- http://www.saglik.gov.tr/TR/dosya/1-16101/h/hastahaklariuygulamayonergesi.pdf.
- Kurtcebe ZÖ. The Evaluation of Knowledge, Attitude and Utilization of Patient Rights of the Patients and Their Relatives Who Applied to A University Hospital and The Residents. [Medical Specialty Thesis]. Gazi University Medical Faculty Department of Public Health; 2009.
- Savaskan F. Determination of Sensitivity on Patient Rights of Nurses and Physicians Working at Public Hospitals in TRNC. [Master’s Thesis]. Istanbul University Graduate School of Health Sciences Department of Nursing; 2006.
- Tappen RM, Weiss SA, Whitehead DK. Essentials of Nursing Leadership And Management. Philadelphia: FA Davis Company; 2001: 263-265.
- Zülfikar F, Ulusoy MF. Are patients aware of their rights? A Turkish study. Nurs Ethics 2001; 8: 487-498.
- Elçioglu Ö, Kirimlioglu N. Principles of Medical Ethics. In: Erdemir AD, Öncel Ö, Aksoy S (eds.) Contemporary Medical Ethics. Istanbul: Nobel Medical Publications, Istanbul; 2003: 26-40.
- Burkhardt MA, Nathaniel AK. Ethics and Issues in Contemporary Nursing. Istanbul: Istanbul Medical Publications, Istanbul; 2013.
- Pektekin Ç. Nursing philosophy. Theories-Maintenance Model Political approaches Istanbul Tip Kitapevi; 2013.
- Öztürk H, Özçelik SK, Bahçecik N. Taking Pains Over Patient Privacy by Nurses. Journal Of Ege University Nursing Faculty 2014; 30: 19-31.
- Bekmezci H, Özkan H. The Importance of Privacy in Midwifery Practices. HSP 2015; 2: 113-124.
- Topbas M, Özlü T, Çan G, Bostan S. How much doctors know about patients’ rights? Knowledge level of residents and interns in a medical school. T Klin J Med Ethics 2005; 13: 81-85.
- Bostan S. The investigation of health employees’ attitudes related patient rights: Instances of Farabi Hospital. HÜ. SaglikIdaresiDergisi 2007; 10: 1-18.
- Kiliçarslan N, Yilmaz FT, Tarim M. The health care providers’ perceptions about patient rights. SagliktaPerformansveKaliteDergisi 2012; 3: 47-62.
- Elçioglu Ö, Erdemir AD. Emerging Ethical Obligations in Every Situation in Clinical Practices. In: Erdemir AD, Oguz Y, Elçioglu Ö, Dogan H (eds.) Clinical Ethics. Istanbul: Nobel Medical Publications, Istanbul; 2001: 104-148.
- Hakeri H. Tip Hukuku. 9. Baski, SeçkinYayincilik, Ankara; 2015.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E, Rollo R, Caldarola P, Giorgino F, Pomo V, Bux F. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag 2010; 6: 297-305.
- Nathaniel AK, Burkhard MA. Contemporary nursing ethics. Istanbul Tip Kitapevi 2013.
- Günay O, Naçar M, Horoz D, Özdemir M, Çitil R, Mutlu SS, Borlu A, Akpinar F. The level of knowledge of inpatiens at Erciyes University hospital on the patient rights. Erciyes Medical Journal 2007; 29: 303-311.
- Teke A, Uçar M, Demir C, Çelen Ö, Karaalp T. Evaluation of knowledge and attitudes of the nurses working in a training hospital about patients’ rights. TSK KoruyucuHekimlikBülteni 2007; 64: 259-266.
- Tanriverdi H, Özmen ME. Effect of patient rights knowledge level on hospital service quality. TSA 2011; 15: 85-109.
- Olsen DP, Dixon JK, Grey M, Deshefy-Longhi T, Demarest JC. Privacy concerns of patients and nurse practitioners in primary care--an APRNet study. J Am Acad Nurse Pract 2005; 17: 527-534.