ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2018) Volume 29, Issue 12
Quitting smoking: experiences from the Southwestern region, Saudi Arabia
Awad S. Alsamghan*
Family and Community Medicine Department, College of Medicine, King Khalid University, Abha, Kingdom of Saudi Arabia
- *Corresponding Author:
- Awad S. Alsamghan
Family and Community Medicine Department
College of Medicine
King Khalid University
Kingdom of Saudi Arabia
Accepted date: May 4, 2018
DOI: 10.4066/biomedicalresearch.29-17-2665
Visit for more related articles at Biomedical ResearchBackground: Tobacco a huge global public health problem with 1.3 billion smokers worldwide contributed to 8.8% of all deaths and 4.1% of DALYs. Current prevalence of tobacco in Saudi is 12.1% considering the extent of tobacco smoking as a health issue.
Objective: This study aims to find out the smoking patterns, quitting trials and determinants of smoking cessation among smokers in Aseer region.
Methods: This study was conducted in six main antismoking clinics located in Abha city, Aseer region using a purposive sampling technique, this medical-record based, retrospective cohort study included data of all smokers (695) who attended the centers for the sake of quitting smoking.
Results: A small percentage (12.8%) had successfully quit smoking i.e. they were smoking free for more than one year. A large proportion (78.3%) reported a previous attempt to quit smoking. Among those who tried to quit smoking, the number of trials ranged from to 1 to 6 times with an average of 2.34 ± 1.46 times and a median of 2 times. The average age of those trying to quit smoking (30.69+10.18 years) was significantly (t=2.127, P=0.034) lower than the corresponding figures of those who did not (32.69 ± 10.31 y).
Conclusion: A good proportion of the respondents have a desire to quit and attempts quitting. The tobacco control program in Saudi Arabia has made great efforts with setting up of smoking cessation clinics that are manned with family physicians.
Keywords
Smoking, Tobacco, Quitting, Saudi Arabia, Ministry of Health
Introduction
Tobacco in its various forms of use is a huge global public health problem with 1.3 billion smokers worldwide. In an initial estimate of factors responsible for the global burden of disease, tobacco contributed to 8.8% of all deaths and 4.1% of DALYs [1]. In Saudi Arabia, tobacco smoking is emerging as a gross public health problem among young and older adults. This has been confirmed through the recent report of the Saudi Health Interview Survey [2], a large national survey developed in partnership between the Ministry of Health in Saudi Arabia and the Institute for Health Metrics and Evaluation of the University of Washington, which was conducted in 2013 in all Saudi regions and included 10,827 participants. Overall, 12.1% of Saudis reported that they currently smoke tobacco. Males accounted for majority of the current as well as daily smokers, however a small percentage of female smokers was also revealed [2].
Considering the extent of tobacco smoking as a health issue, it is essential that public health experts should concentrate on smoking cessation activities and programs. Irrespective of age, quitting smoking is beneficial to health, so much so, that if a smoker quits before the age of 35 years have his premature mortality rates are similar to those of persons who never smoked [3,4]. The prevalence of cigarette smoking among adults (aged ≥ 18 y) in the United States decreased from 42.4% to 18.1%, over the past four decades. This decline is explained partly due to increase in smoking cessation [3,4]. In the Saudi study, almost half of the smokers; i.e. 49.1% reported having attempted to quit smoking within the last 12 months [2].
In Saudi Arabia, the Tobacco Control Program is affiliated to the Ministry of Health (MOH). It was established in 2002. The program provides scientific and advisory services on all aspects of smoking awareness and its harms as well as methods to combat it. It also oversees a series of tobacco control clinics set up in a number of cities in the Kingdom. The policy of this programme includes a number of factors including offering help to quit and warning of the dangers of tobacco [5].
The use of counselling, along with smoking cessation aids like nicotine replacement therapy, can improve the chances of successful smoking cessation [6]. Clinical trials provide strong evidence that pharmacotherapy for smoking cessation, including various forms of Nicotine Replacement Therapies (NRT), bupropion or varenicline, greatly increases the chances of a successful smoking cessation attempt [7,8].
Saudi Ministry of health has established smoking cessation clinics, equipped with trained personnel, to offer free consultation as well as provision of free NRT for the full course of treatment [5]. Notwithstanding, a notable finding in the Saudi study pointed that just a little more than half of the smokers reported having been advised by their physician or a health care professional to quit smoking during any visit within the last year.
Quitting has been described as an elaborate process that needs to be understood for optimizing interventions. Moreover, there is a need to explore the reasons for quitting and the choice of methods to assist quitting. The information, about previous quitting attempts, experiences and preferences could help in guiding the future attempts at quitting and improve chances of successful quitting. This would in turn, ensure efficient use of clinicians’ time and limited healthcare resources [9].
A number of studies in Saudi Arabia have focused on the epidemiology of smoking [10,11]. However, there is lack of information on the other important aspect, i.e. smoking cessation. This study aims to find out the smoking patterns, quitting trials and determinants of smoking cessation among smokers in Aseer region. It hopes to provide seminal information on these aspects, which would provide a better understanding of the smoking control programme in Saudi Arabia, particularly in Aseer region.
Method
Study setting: This study was conducted in the main antismoking clinics located in Abha city, the capital of Aseer region, Southwestern Saudi Arabia. The smoking-cessation clinics are six specialized clinics covered mainly by family doctors, having special training in smoking cessation. The centers are also equipped with pharmacy containing most commonly used medications in smoking cessation and are dispensed free of cost for the entire treatment period for the patients. Study period: The study extended for a period of eleven months, from January to November 2016. Study procedure: Using a purposive sampling technique, this medical-record based, retrospective cohort study included data of all smokers (695) who attended the centers for the sake of quitting smoking during the study period. Information was collected on a data driven form, based on the patient record maintained in the smoking-cessation clinic. A group of five intern doctors helped to collect the data. Any incomplete records were excluded. Study tool: The data collected include patient characteristics including: Age, gender, marital status, educational and occupational status, residence ownership, residential area, monthly family income and any smoker family member. Smoking characteristics included age at starting smoking, reason for starting smoking, number of cigarettes smoked per day, morning smoking, desire to quit, previous quitting trials, longest period of abstinence, reasons for wanting to quit, knowledge of side effects, use of medication for quitting and type of quitting aid (medication used).
Data analysis
Data was coded and entered into SPSS 20. Descriptive statistics (frequency, percentage, mean and standard deviation) was used to present the basic data about patient sociodemographic and smoking characteristics, quitting characteristics and reasons for quitting attempt. Chi square and t-test was used to find association between the various sociodemographic and smoking characteristics and quitting attempt.
Results
The present study included 695 smokers who attended antismoking clinics during the study period. The age of the study group ranged between 14-80 y, with a mean age of 31.13 y, and a standard deviation of 10.23 y. The basic characteristics are described in Table 1.
| Patient characteristic | Number | % |
|---|---|---|
| Age | ||
| <20 | 70 | 10.1 |
| 20-29 | 265 | 38.1 |
| 30-39 | 242 | 34.8 |
| 40-49 | 74 | 10.7 |
| >50 | 44 | 6.3 |
| Gender | ||
| Male | 690 | 99.3 |
| Female | 5 | 0.7 |
| Education Level | ||
| Illiterates | 7 | 1 |
| Primary | 18 | 2.6 |
| Intermediate | 40 | 5.8 |
| Secondary | 288 | 41.4 |
| University | 325 | 46.8 |
| Postgraduate | 17 | 2.4 |
| Work | ||
| Unemployed | 11 | 1.6 |
| Student | 157 | 22.6 |
| Govt. Job | 355 | 51.1 |
| Private | 104 | 15 |
| Others | 68 | 9.7 |
| Income | ||
| No fix income | 165 | 23.8 |
| < 3000 SR | 101 | 14.5 |
| 3000-6000 SR | 118 | 17 |
| 6001-10000 SR | 167 | 24 |
| >10000 SR | 144 | 20.7 |
| Marital Status | ||
| Married | 407 | 58.6 |
| Single | 288 | 41.4 |
| Home | ||
| Own | 342 | 49.2 |
| Rented | 353 | 50.8 |
| Smoker in family member | ||
| Yes | 378 | 54.4 |
| No | 317 | 45.6 |
Table 1. Basic socio-demographic characteristics of smokers attending the anti-smoking clinics.
Almost all (99.3%) of the smokers were males. About 41% were educated to secondary school level and (46.8%) university level. While 22.6% of our respondents were still students, more than half (51.1%) were government employees. Unemployment was not commonly found in the study group. The income level of respondents varied widely and was equally distributed between most groups as depicted in the table. More than one-fifth of our study population (23.8%) reported not having a fixed income. Fifty eight percent of the respondents were married and house ownership was reported by about half of them. More than half of the respondents (54.4%) reported having a smoker within their family.
Smoking practices of the study group
Table 2 describes the smoking practices of the study group. The age at initiation shows that most of the respondents started smoking in their adolescence (67.8%), with cigarette being the most common type of agent used (61.6%).In more than 47% smokers, the influence to smoke was from their friends. About 40% smokers reported using 11-20 cigarettes per day, and 46.2% reported having the first cigarette in the morning within 5 min of waking.
| Types of smoking | Number | % |
|---|---|---|
| Cigarette | 428 | 61.6 |
| Shishah | 21 | 3 |
| Cigar | 3 | 0.4 |
| Cigarette and Shishah | 34 | 4.9 |
| Cigarette and Tinbak | 182 | 26.2 |
| More than two types of tobacco use | 27 | 3.9 |
| Age at starting smoking | ||
| ≤ 10 | 14 | 2 |
| 11/19 | 471 | 67.8 |
| 20-29 | 200 | 28.8 |
| 30 and above | 10 | 1.4 |
| Influence for starting of smoking | ||
| Friends | 330 | 47.5 |
| Co-workers | 65 | 9.3 |
| Family | 20 | 2.9 |
| Stress | 118 | 17 |
| Advertisement | 28 | 4 |
| Combination of the above | 41 | 5.9 |
| Friends and co-workers | 31 | 4.5 |
| Friends and Stress | 62 | 8.9 |
| Cigarette consumption per day | ||
| 1/10 | 190 | 27.3 |
| 11/20 | 283 | 40.7 |
| 21-30 | 134 | 19.3 |
| >31 | 88 | 12.7 |
| Morning smoking | ||
| Within first five minutes | 321 | 46.2 |
| After 31-60 min from waking | 203 | 29.2 |
| After one hour | 171 | 24.6 |
| Smoking side effects (*HTN, IHD, COPD, teeth staining, cough, bad smell). | ||
| Yes | 202 | 29.1 |
| No | 493 | 70.9 |
Table 2. Smoking characteristics of the study population.
Quitting characteristics
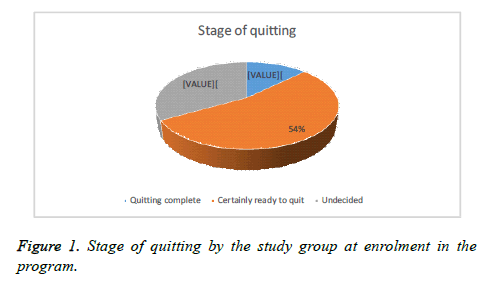
Out of a total of 695 smokers, small percentage (12.8%) had successfully quit smoking i.e. they were smoking free for more than one year. Fifty four percent reflected a desire to quit, while about one third were still undecided about quitting (Figure 1). A large proportion i.e. 544 (78.3%) reported a previous attempt to quit smoking. Among those who tried to quit smoking, the number of trials ranged from to 1 to 6 times with an average of 2.34 ± 1.46 times and a median of 2 times. The longest period of quitting smoking ranged from 1 day to 360 days with an average of 31.1 ± 52.9 d and a median of 7 d. Table 3 describes reasons mentioned among those who tried to quit smoking. The mostly frequent mentioned reasons were health and religious. The majority of those who tried to quit smoking (407, 74.8%) were not using any medication to stop smoking. Among those who used medication (n=137), champix (vareniclline) was the most frequently used drug (52.6%) (Table 4).
| Reasons for attempting a quitting trial | Number | % |
|---|---|---|
| Religious | 82 | 11.8 |
| Health | 107 | 15.4 |
| Economic | 20 | 2.9 |
| Social | 26 | 3.7 |
| Religious and health | 152 | 21.9 |
| Religious and economic | 11 | 1.6 |
| Religious and Social | 38 | 5.5 |
| Religious , health and social | 127 | 18.3 |
| Religious, health, social and economic | 117 | 16.7 |
| No particular reason | 15 | 2.2 |
Table 3. Reasons for attempted quitting among the smokers.
| Use of medication in previous quitting trial | Number | % |
|---|---|---|
| No | 407 | 74.8 |
| Yes | 137 | 25.2 |
| Medication used* | ||
| Varenicline (Champix) | 72 | 52.6 |
| Nicotine patch | 40 | 29.2 |
| Nicotine lozenge | 13 | 9.5 |
| Nicotinell | 4 | 2.9 |
| Champix+nicotine patch | 4 | 2.9 |
| Champix+nicotinell | 1 | 0.7 |
| Others | 3 | 2.2 |
Table 4. Use and type of nicotine replacement therapy in quitting.
The average age of those trying to quit smoking (30.69 ± 10.18 y) was significantly lower (t=2.127, P=0.034), than the corresponding figures of those who did not (32.69 ± 10.31 y).
Table 5 shows the univariate analysis of factors that affected attempts to quit smoking. The table shows that significantly more smokers of younger age attempted quitting smoking as compared to older (COR=1.497, 95% CI=1.038-2.159). Also, married subjects attempted quitting smoking significantly more than the singles (COR=1.631, 95% CI=1.115-2.386). Those who experienced smoking related disease attempted quitting significantly more than those who did not (COR=1.69, 95% CI=1.09-2.59). People in private jobs were more likely to attempt quitting smoking, though it was not significant. On the other hand, education, income, home ownership, number of daily cigarette smoking, having any chronic disease having any smoker in the family were of no significant association with smoking quitting trial.
| Variables | Previous quitting attempt | p-value* | |||
|---|---|---|---|---|---|
| Yes (N=544) | No (N=151) | ||||
| Age | |||||
| >20 | 58 | 82.9 | 12 | 17.1 | 0.174 |
| 20-29 | 216 | 81.5 | 49 | 18.5 | |
| 30-39 | 186 | 76.9 | 56 | 23.1 | |
| 40-49 | 52 | 70.3 | 22 | 29.7 | |
| 50 up | 32 | 72.7 | 12 | 27.3 | |
| Education level | |||||
| Illiterate | 6 | 85.7 | 1 | 14.3 | 0.77 |
| Primary | 13 | 72.2 | 5 | 27.8 | |
| Intermediate | 28 | 70 | 12 | 30 | |
| Secondary | 227 | 78.8 | 61 | 21.2 | |
| University | 256 | 78.8 | 69 | 21.2 | |
| Postgraduate | 14 | 82.4 | 3 | 17.6 | |
| Income | |||||
| No fix income | 129 | 78.2 | 36 | 21.8 | 0.47 |
| Less than 3000 | 82 | 81.2 | 19 | 18.8 | |
| 3000-6000 | 98 | 83.1 | 20 | 16.9 | |
| 6001-10000 | 127 | 76 | 40 | 24 | |
| More than 10000 | 108 | 75 | 36 | 25 | |
| Job | |||||
| Jobless | 10 | 90.9 | 1 | 9.1 | 0.06 |
| Student | 126 | 80.3 | 31 | 19.7 | |
| Government | 264 | 74.4 | 91 | 25.6 | |
| Private | 90 | 86.5 | 14 | 13.5 | |
| Others (e.g. Retired) | 54 | 79.4 | 14 | 20.6 | |
| Marital status | |||||
| Married | 305 | 74.9 | 102 | 25.1 | 0.01 |
| Single | 239 | 83 | 49 | 17 | |
| Smoke related disease (HTN ,IHD, COPD) | |||||
| No | 374 | 75.8 | 119 | 24.2 | <0.01 |
| Yes | 170 | 84.1 | 32 | 15.9 | |
Table 5. Relationship of quitting attempt with socio-demographic factors.
Discussion
The present study included 695 smokers who attended antismoking clinics in Aseer region. Most of the smokers were young males about one fourth being students. Most of the respondents started smoking in their adolescence and friends were the most common influence to start smoking. All these findings are supported by existing smoking literature. Smoking in the United States has displayed prevalence among those aged 18-30 y is the highest of all adult age groups [12].
In the current study, 78.3% smokers reported a previous attempt to quit smoking, and most of them expressed a desire to quit. These are positive findings as attempted quitting indicates seriousness in the smoker’s attitude to cease smoking and is considered as the final stage in the process of contemplation and preparation for quitting [13]. In studies on some Western populations, 10-20% of smokers report planning to quit or seriously thinking about making an attempt in the next month [14]. Other studies have found higher proportions (46%) of smokers saying that they intend to quit within the next year [15]. A prospective cohort study across four western countries reported 82.0% of smokers having made any quit attempts at recruitment. In a US study, 65.9% smokers reported attempts at quitting [16].
Among those who tried to quit smoking, the number of trials ranged from to 1 to 6 times and the longest period of quitting smoking ranged from 1 day to 360 d.
The four country study revealed that though most quit attempts end rapidly, the majority of smokers succeeded in staying quit for more than 1 month and around one third could stop for more than 6 months [16]. In this study, 12.8% smokers had successfully quit smoking i.e. they were smoking free for more than one year.
A similar finding has been observed in the four country study that reported 15.5% successful quitters.
The findings in the present study point that younger smokers reported more quitting desire than the older smokers. The average age of those trying to quit smoking at 30.69 ± 10.18 y was significantly lower than the corresponding figures of those who did not. This finding finds support in a US study that reported lower quit attempts in older age groups [16]. In the four country study, findings revealed that those with prior attempts were more likely to be older and female. Quitting smoking is beneficial to health at any age, and cigarette smokers who quit before age 35 years have mortality rates similar to those of persons who never smoked [16]. Another socio-demographic factor that significantly affected quitting behavior was marital status; with married subjects significantly more likely to attempt quitting smoking as compared to singles.
The mostly frequent mentioned motivations for quitting attempts were health and religious reasons. Although the Saudi government has raised taxes over imported cigarettes to 100% [5] this does not seem to affect the smokers enough to act as a motivator for quitting, probably due to a high per capita GDP in the kingdom. Studies have revealed many motivators for quitting. Among Japanese smokers, the rise in cigarette prices was reported as a main motivator especially among the nicotine dependent [17]. Other studies reported that smokers acknowledged that concerns or problems related to personal health as motivating factors for stopping smoking [18].
Researchers, advocates and healthcare practitioners have emphasized that the chances of quitting successfully can be increased by using Nicotine-Replacement Therapy (NRT), or other pharmacotherapies like bupropion and varenicline. This could be complemented with behavioral support in the form of counseling from a healthcare professional [5,19]. However, it is revealed from studies that most quit attempts are unassisted [20] and most smokers quit without pharmacological or professional assistance [21]. Qualitative studies on smoking and quitting behaviors have reported a number of interesting factors that inhibit the smokers from effective seeking and utilization of healthcare. Not seeking help for quitting seems not to result from a lack of knowledge about the assistance available, but due to complex factors like evaluation of the perceived costs and benefits of using assistance compared with the costs and benefits of quitting unassisted. Many participants assumed that quitting is their individual responsibility or identified quitting without any assistance to be the ‘right’ or ‘better’ option [21]. In these studies, the subjects who quit on their own were reluctant to consult their physician, basically as they did not view smoking or quitting as an illness [22,23].
The present study also focused on the use and type of pharmacotherapy used in quitting trials. There are many studies that have reported increased cessation rates with the use of pharmacotherapy [24,25], but in the current study, more than three quarters of those who tried to quit smoking were not using any medication to stop smoking. Among those who used medication (n=125), verincline was the most frequently used drug (54.4%). In this study, the use of NRT did not show any association with successful quitting. Though this finding is similar to population-based studies that have shown no difference in cessation rates between those who use and those who do not use pharmacotherapy [12,26,27], it points to inadequate counseling process and suggests a lack of knowledge regarding use and benefits of using pharmacotherapy for quitting smoking.
Helping tobacco users to quit can reduce tobacco-related disease, death, and health care costs [3,28]. Increasing taxes on tobacco products, passing and implementing indoor smoke free laws, improving health insurance coverage of cessation services, and integrating tobacco dependence treatment into routine clinical care have all helped increase cessation rates [3,28].
Conclusion
The study findings conclude that a good proportion of the respondents have a desire to quit and attempts quitting. The findings of this study point to an association between quitting attempts and patient characteristics (younger smokers, married smokers, and smokers suffering from side effects). These findings suggest that smoking cessation services can be targeted to these groups in order to improve the utilization of services. The tobacco control program in Saudi Arabia has made great efforts with setting up of smoking cessation clinics that are manned with family physicians, which is an advantage as they have the ability to manage comorbidities like DM,HTN, asthma or psychiatric problems like depression and anxiety, besides offering full course of free NRT for attempters. It is expected that the study findings will help in better directing of the smoking cessation services and consequently improve the utilization of existing services in the tobacco control program in this region.
Acknowledgement
The author wishes to acknowledge Dr. Aesha Siddiqui, Assistant professor, Department of Family and Community Medicine King Khalid University for her expert guidance in bringing this work into its present form. Appreciation is also extended to the interns and clinical staff at the PHCCs, without whose help this work would not have been possible.
References
- WHO report on the global tobacco epidemic 2015.
- Saudi Health Interview Survey. http: //www.healthdata.org/sites/default/ files/files/Projects/KSA/Smoking-KSA-Findings-from-the-Saudi-Health-Interview-Survey.pdf. Retrieved on March 8, 2017.
- U.S. Department of Health and Human Services. The health consequences of smoking-50 years of progress: a report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
- Xu F, Town M, Balluz LS, Bartoli WP, Murphy W, Chowdhury PP. Surveillance for certain health behaviors among states and selected local areas-United States, 2010. MMWR Surveill Sum 2013; 63: 1.
- Al-Munif. Report on tobacco control program of Ministry of Health in Saudi Arabia Ministry of Health, Riyadh, 2009.
- Stead LF, Buitrago D, Preciado N. Physician advice for smoking cessation. Cochrane Database Syst Rev 2013; 5: 000165.
- Cahill K, Stevens S, Perera R. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev 2013; 5: 009329
- Raupach T, van Schayck CP. Pharmacotherapy for smoking cessation: current advances and research topics. CNS Drugs 2011; 25: 371-382.
- Thomas D, Abramson MJ, Bonevski B. Quitting experiences and preferences for a future quit attempt: a study among inpatient smokers. BMJ Open 2015; 5: 006959.
- Bassiony MM. Smoking in Saudi Arabia. Saudi Med J 2009; 30: 876-881.
- Siddiqui S, Ogbeide DO, Al Khalifa I. Smoking in a Saudi community: prevalance, influencing factors, and risk perception. Fam Med 2001; 33: 367-370.
- Buller DB, Halperin A, Severson HH, Borland R, Slater MD, Erwin P. Effect of nicotine replacement therapy on quitting by young adults in a trial comparing cessation services. J Public Health Manag Pract 2014; 20: 7-15.
- Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Country Cohort Survey Addiction 2012; 107: 673-682.
- Kaida A, Edwards J, Fraser-Lee N, Kunyk D, Lightfoot P, Marko J, Spence JC, Spinola C. Smoking in the Capital Health Region-Report, Population Health Survey 2002. Edmonton, Alberta Capital Health 2004.
- West R, McEwen A, Bolling K, Owen L. Smoking cessation and smoking patterns in the general population: a 1-year follow-up. Addiction 2001; 96: 891-902.
- René Lavinghouze S, Ann M, Amal J, Linda N, Karen D, Laura W. Trends in quit attempts among adult cigarette smokers-United States, 2001-2013. MMWR Morb Mortal Wkly Rep 2015; 64: 1129-1135.
- Tanihara S, Momose Y. Reasons for smoking cessation attempts among Japanese male smokers vary by nicotine dependence level: a cross-sectional study after the 2010 tobacco tax increase. BMJ Open 2015; 5: 006658.
- Ministry of Health, Labour and Welfare. The survey for smoking and health problems in Japan 2017.
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev 2009; 2: 001007.
- Edwards SA, Bondy SJ, Callaghan RC. Prevalence of unassisted quit attempts in population-based studies: a systematic review of the literature. Addict Behav 2014; 39: 512-519.
- Smith AL, Carter SM, Chapman S. Why do smokers try to quit without medication or counselling? A qualitative study with ex-smokers. BMJ Open 2015; 5: 007301.
- Fu SS, Burgess D, Ryn MV. Views on smoking cessation methods in ethnic minority communities: a qualitative investigation. Prev Med 2007; 44: 235-240.
- Levinson AH, Borrayo EA, Espinoza P. An exploration of Latino smokers and the use of pharmaceutical aids. Am J Prev Med 2006; 31: 167-171.
- Kasza KA, Hyland AJ, Borland R. Effectiveness of stop-smoking medications: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction 2013; 108: 193-202.
- Miller N, Frieden TR, Liu SY. Effectiveness of a large-scale distribution programme of free nicotine patches: a prospective evaluation. Lancet 2005; 365: 1849-1854.
- Alpert HR, Connolly GN, Biener L. A prospective cohort study challenging the effectiveness of population-based medical intervention for smoking cessation. Tob Control 2013; 22: 32-37.
- Pierce JP, Gilpin EA. Impact of over-the-counter sales on effectiveness of pharmaceutical aids for smoking cessation. JAMA 2002; 288: 1260-1264.
- Smoking and tobacco use: best practices for comprehensive tobacco control programs-2014. Atlanta, GA: US Department of Health and Human Services, CDC; 2014. Available at http: //www.cdc.gov/tobacco/ state and community/best_practices