ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 1
Radiological measurements of the wrist in intraoperative positions
1Department of Orthopedic Surgery, Nagasaki University Graduate School of Biomedical Sciences, 1-7-1, Sakamoto, Nagasaki 852-8501, Japan
2Department of Locomotive Rehabilitation Science, Unit of Rehabilitation sciences, Nagasaki University Graduate School of Biomedical Sciences, 1-7-1, Sakamoto, Nagasaki 852-8520, Japan
3Department of Radiology, Wajinkai Hospital, 96, Nakazato, Nagasaki, 851-0103, Japan
4Department of Orthopedic Surgery, Wajinkai Hospital, 96, Nakazato, Nagasaki, 851-0103, Japan
- *Corresponding Author:
- Hironobu Koseki
Department of Locomotive Rehabilitation Science
Unit of Rehabilitation Sciences
Nagasaki University Graduate School of Biomedical Sciences
1-7-1, Sakamoto, Nagasaki 852-8520, Japan
Accepted date: June 08, 2016
Purpose: The purpose of this study was to investigate and quantify the effects of the intraoperative position on radial inclination, ulnar variance, and the position of the ulnar styloid in normal human wrists.
Methods: Plain radiographs were taken of 30 adult volunteers (15 male, 15 female) in 3 positions: a standard wrist imaging position and two different intraoperative positions (supine with the palm of the hand in contact with the cassette and supine with the dorsum of the hand in contact with the cassette).
Results: The results showed that the ulnar styloid migrated in both intraoperative positions, and radial inclination was increased in the supine position with the palm of the hand in contact, especially in males.
Conclusions: The results of this study indicate that forearm rotation in the intraoperative position may affect the accuracy of radiographic measurements. Type of study/level of evidence: Diagnostic, III
Keywords
Position, Radiography, Wrist
Introduction
The human wrist is comprised of the radius, ulna, 8 carpal bones of a unique shape, and many ligaments that connect these bones. These complex structures and multi-directional joints permit fine movements of the hand and fingers. However, these delicate structures also make the hand susceptible to functional impairment due to various disorders. Wrist disorders vary widely, including: injuries such as distal radius fractures, scaphoid fractures, and lunate dislocation; degenerative diseases such as osteoarthritis; and inflammatory diseases such as Kienböck’s disease and rheumatoid arthritis. The types and severity of residual impairments after treatment also vary.
Distal radius fractures are a particularly common fracture of the upper extremity in elderly patients. These injuries can be treated conservatively or with surgery depending on the fracture type and stability. However, poor or unstable reduction of dislocated bone fragments can lead to various complications including pain, limited range of motion, swelling, contractures, and reflex sympathetic dystrophy. Grewal et al. [1] reported poor clinical outcomes, with residual deformities such as ulnar variance (UV) ≥ 3 mm and radial inclination (RI) <15°. Moreover, even trifling abnormalities of UV and RI are associated with subsequent development of ulnocarpal abutment syndrome, scapholunate instability, distal radioulnar joint disorders, and triangular fibrocartilage complex perforation [2-5]. Therefore, careful evaluation with accurate radiographic imaging is essential. However, some reports found that the positional relationships of structures comprising the wrist joint are easily affected by limb and body position during imaging [6-9]. It is for these reasons that images acquired by standard imaging techniques are generally used for accurate wrist measurement. The standard imaging technique was proposed by Palmer et al [6]. Postero-anterior (PA) views of the wrist are taken in a seated position, with 90° shoulder abduction, 90° elbow flexion, and the forearm in neutral rotation.
However, manual reduction under fluoroscopy or intraoperative evaluation using a surgical X-ray imaging system is often performed in the supine positon with the elbow in almost full extension. The question we addressed was: Can surgeons judge UV and RI using the images obtained in intraoperative positions that are different from the standard imaging technique? However, we found no prior studies that discussed wrist radiographs from this perspective.
The objective of this study was to compare and investigate differences in measured values on plain radiographs of the wrist taken in the standard imaging positions and intraoperative positions. This study was approved by the Ethical Review Board of our institute. The nature of the study was thoroughly explained, and informed consent was obtained from each participant.
Subjects and Methods
This study included 30 healthy adult volunteers (15 men; 15 women) who had no complaints about and no prior disease of the finger or wrist joints. The mean age of the participants was 26.3 years (range: 21-43 years) (Table 1). Plain radiographs of the wrist were taken using a high voltage device (KXO-80G, Toshiba, Tokyo, Japan) and a beam-limiting device (TF-6TL-6, Toshiba). Imaging conditions were 50 kV, 8 mAs (250 mA, 32 msec), and an image distance of 100 cm.
| Height (cm) | Weight (kg) | BMI (kg/m2) | |
|---|---|---|---|
| All participants | 165.3 ± 9.2 | 59.9 ± 15.4 | 21.7 ± 3.3 |
| Males | 173.6 ± 6.8 | 70.0 ± 17.9 | 23.0 ± 3.8 |
| Females | 158.6 ± 3.7 | 51.9 ± 5.6 | 20.7 ± 2.6 |
Table 1: Physical features.
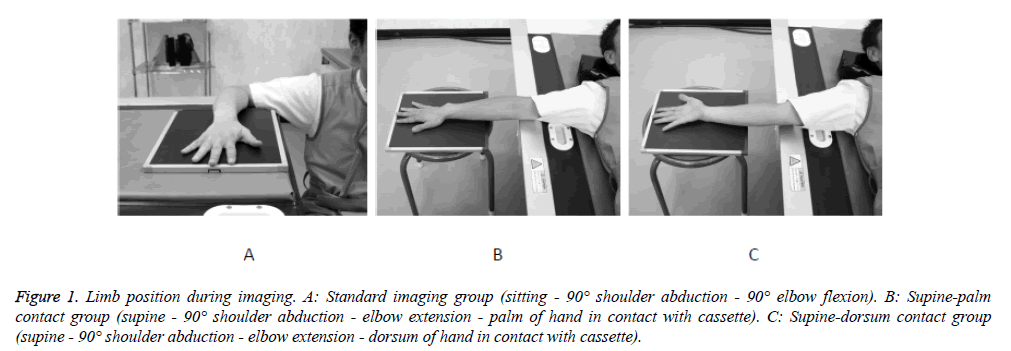
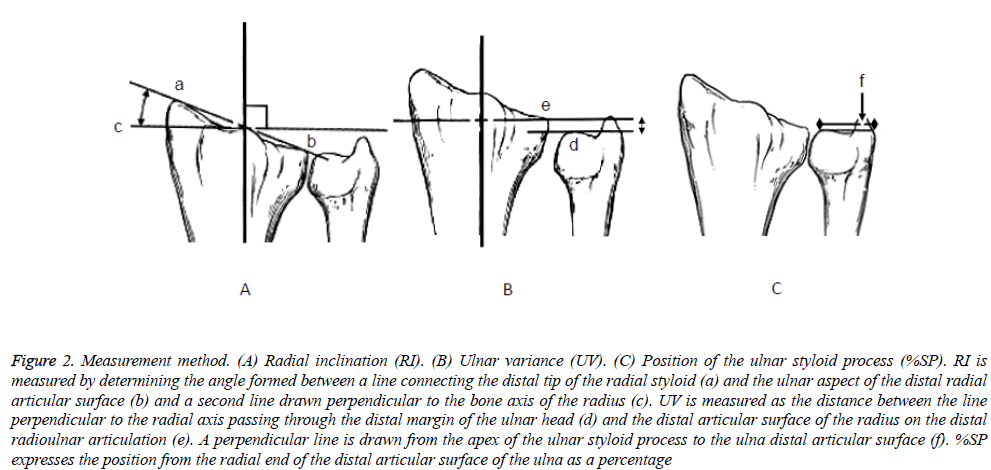
All imaging was performed by one radiological technician under uniform setting conditions. Three limb positions were used for imaging (Figures 1A-1C): a standard wrist imaging technique “sitting-90° shoulder abduction-90° elbow flexion” (standard imaging group) [6] and two typical intraoperative limb positions: “supine-90° shoulder abduction-elbow extension-palm of the hand in contact with the cassette” (supine-palm contact group); and “supine-90° shoulder abduction-elbow extension-dorsum of the hand in contact with the cassette” (supine-dorsum contact group). The wrist joint was placed on the center of the cassette surface. After adjustment to align the radius axis and the third finger bone axis, the X-ray beam was focused directly over the midpoint of the radio carpal joint. Participants were asked to relax during imaging. Radiographs were taken of the right wrist in all patients irrespective of their dominant hand. The acquired images were used to measure RI, UV, and the position of the ulnar styloid process (%SP). The bone axis of the radius was assumed to be a line that bisected the distal shaft of the radius 5 and 10 cm proximal to the distal radial articular surface. RI was measured by determining the angle formed between a line connecting the distal tip of the radial styloid and the ulnar aspect of the distal radial articular surface and a second line drawn perpendicular to the axis of radius [9-11]. UV was measured according to the Gelberman method [5]. A minus variance is when the distal end of the ulna is shorter than the ulnar aspect of the distal radial articular surface. To measure %SP, a perpendicular line is drawn from the apex of the ulnar styloid process to the ulna distal articular surface; %SP expresses the position from the radial end as a percentage (Figure 2). The %SP is a new measurement category that the authors have devised as an index to evaluate forearm rotation.
Figure 1: Limb position during imaging. A: Standard imaging group (sitting - 90° shoulder abduction - 90° elbow flexion). B: Supine-palm contact group (supine - 90° shoulder abduction - elbow extension - palm of hand in contact with cassette). C: Supine-dorsum contact group (supine - 90° shoulder abduction - elbow extension - dorsum of hand in contact with cassette).
Figure 2: Measurement method. (A) Radial inclination (RI). (B) Ulnar variance (UV). (C) Position of the ulnar styloid process (%SP). RI is measured by determining the angle formed between a line connecting the distal tip of the radial styloid (a) and the ulnar aspect of the distal radial articular surface (b) and a second line drawn perpendicular to the bone axis of the radius (c). UV is measured as the distance between the line perpendicular to the radial axis passing through the distal margin of the ulnar head (d) and the distal articular surface of the radius on the distal radioulnar articulation (e). A perpendicular line is drawn from the apex of the ulnar styloid process to the ulna distal articular surface (f). %SP expresses the position from the radial end of the distal articular surface of the ulna as a percentage
Three different observers evaluated each case twice, separated by a minimum of two weeks; intra-observer reliability was assessed using the first author’s evaluations, and inter-observer reliability was assessed by comparing the first and second authors’ evaluations. The readers were blinded for each measurement to the previous results, and the mean values were used as the measured values. The measurements for each limb position were compiled for statistical analysis, which included one-way analysis of variance (one-way ANOVA) multiple comparison tests and Tukey-Kramer and Bonferroni/Dunn multiple comparison tests for post hoc analysis. The Mann- Whitney U-test was used for two-group comparisons of sexrelated differences. Significance was defined as a P value of 0.05 or smaller.
Results
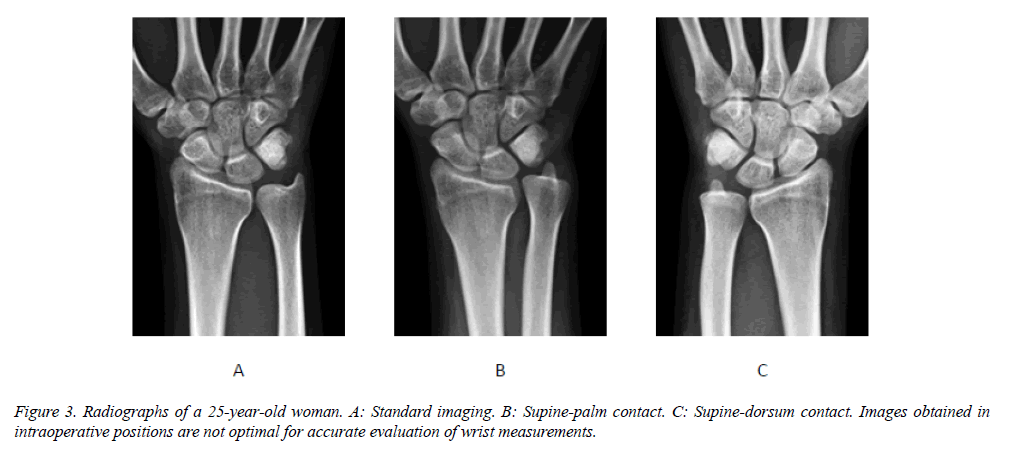
The mean values and standard deviations of RI, UV, and %SP in each group are shown in Table 2. Radial inclination was significantly greater in the supine-palm contact group than in the supine-dorsum contact group (P<0.05). The %SP was significantly different in both the supine-palm contact and supine-dorsum contact groups compared to the standard imaging group (P<0.05) (Figures 3A-C). In both groups, a high value of %SP standard deviation indicated greater variation.
| Standard imaging group | Supine-palm contact group | Supine-dorsum contact group | |
|---|---|---|---|
| Radial inclination (RI:°) | 27.3 ± 2.5 | 29.4 ± 2.5a | 27.4 ± 2.4 |
| Males | 26.3 ± 1.9 | 29.0 ± 2.0a,b | 26.7 ± 1.6 |
| Females | 28.3 ± 2.7* | 29.8 ± 2.9 | 28.0 ± 2.8 |
| Ulnar variance (UV: mm) | -0.4 ± 1.7 | -0.2 ± 1.7 | -0.9 ± 1.9 |
| Males | -0.9 ± 1.7 | -0.7 ± 1.8 | -1.4 ± 1.8 |
| Females | 0.1 ± 1.6 | 0.3 ± 1.4* | -0.4 ± 1.8 |
| Ulnar styloid process position (%SP: %) | 86.6 ± 2.5 | 74.3 ± 8.5b | 70.8 ± 9.4b |
| Males | 86.3 ± 2.8 | 73.5 ± 7.9b | 70.9 ± 9.7b |
| Females | 87.0 ± 2.2 | 75.2 ± 9.2b | 70.7 ± 9.4b |
| a: Significant difference compared with the supine-dorsum contact group (P<0.05) b: Significant difference compared with the standard imaging group (P<0.05) *: Significant sex-related difference (P<0.05) |
|||
Table 2: Measurement values.
In men, RI was greater in the supine-palm contact group than in the standard imaging group and the supine-dorsum contact group, whereas, in women, there were no significant changes in RI or UV among the three groups. However, in men and women, the %SP decreased significantly in both the supine-palm contact and supine-dorsum contact group compared to the standard imaging group (P<0.05). When differences between men and women were compared within each group, there were significant differences for RI in the standard imaging group and UV in the supine-palm contact group (P<0.05).
Discussion
Disruption and abnormalities of wrist structure are directly linked with functional impairment of the hand. Radiographic measurements to evaluate structures of the wrist are important to diagnose and avoid various subsequent disorders, thus requiring high accuracy and precision [1,2]. Distal radius fractures are commonly encountered in clinical practice, and if the dislocated bone fragments are not reduced to an optimal position, this can lead to reduced activities of daily living due to impaired hand function and other sequelae [1-3]. However, positional relationships of bones in the wrist can easily change depending on limb position [6-9]. Thus, accurate radiographs obtained by standard imaging techniques are recommended for assessment. In actual practice, however, fractures are often manually or surgically reduced in patients who are lying supine in a bed with their elbows extended. This deviates from the proper limb position required for standard imaging. Therefore, we orthopedic surgeons must investigate whether imaging by fluoroscopy and surgical X-ray imaging systems is suitable to evaluate the reduced positions of fractures. In this study, the measurements of the wrist on plain radiographs were compared with those in the standard imaging position and typical intraoperative positions.
The present study included normal wrist joints from healthy (relatively young) Japanese adults. Gartland et al. [10] reported a mean RI of 23° (13-30°) from radiographs of 60 normal wrists, and Smilovic et al. [11] reported a mean RI of 26.6 ± 2.9° (20-30°). Gelberman et al. [5] reported mean UV values in Caucasians (0.27 ± 1.7 mm) and African-Americans (0.7 ± 1.7 mm) on radiographs with the forearm in pronation. In the present study using a standard imaging technique, RI was 27.3 ± 2.5°, and UV was -0.4 ± 1.7 mm. Because of possible differences in the subjects (body habitus due to ethnicity and age) and imaging techniques, a direct comparison between the present study and previous reports is difficult. Nevertheless, the results of the present study may serve as normal reference measurements of the Japanese wrist in a correct standard radiograph. With regard to the sex-related differences in RI in the standard imaging group, carpal bone arrangement and transverse diameter may have been involved, but the detailed reasons are unknown. To develop normal RI values in the future, separate standards for men and women should be considered.
Several studies reported that measurements on wrist radiograph are significantly affected by body position [7,8,12]. The present study found that, in a supine-palm contact position, which is usually used for closed reduction of dorsally displaced bone fragments in distal radius fractures, RI was increased and %SP was decreased. The ulnar styloid process is located on the most ulnar side with the forearm in the neutral rotation position, and it migrates radially even with pronation and supination [7]. Therefore, in a supine-palm contact position, the forearm tends to pronate, and the RI is thought to be higher than normal. In a supine-dorsum contact position, often used for a volar plating procedure, there were no significant differences in RI and UV, but %SP decreased. These findings suggest that the forearm tends to rotate from the neutral position during operation. The high %SP standard deviations for both intraoperative positions indicate large individual variations in the degree of rotation.
The present results could not confirm any effect on UV. However, the mean %SP did change in both intraoperative positions, thus showing that intraoperative position can easily lead to changes in forearm rotation. Cadaver studies by Epner et al. [7] showed that forearm supination increases negative UV, whereas pronation decreases negative UV. Yeh et al. [8] and Pennock et al. [9] also found that forearm rotation affected measurements of RI and UV in human subjects. The difference of forearm rotation may be one reason why RI was increased in the supine-palm contact group. Furthermore, surgeons often put sterilized sheets and a pneumatic tourniquet around the upper arm of patients during surgery. Such situations decrease upper arm mobility and can further increase the risk of abnormal forearm rotation. For these reasons, it is difficult to say that images acquired in intraoperative positions are optimal for accurate evaluation of measurements. The surgeons must keep in mind the fact that the image obtained during surgery is not the same as a standard image, and that a patient’s forearm rotation can easily change in the intraoperative position. Our proposed measurement of %SP can help assess the rotated forearm position.
There are several limitations to the present study. It involved a small number of participants, and they tended to be relatively young. Therefore, further studies are needed to confirm whether the current findings are also seen in middle-aged and older adults, in whom most distal radius fractures occur. However, the present study provides valuable results for wrist measurements in different intraoperative positions, which are likely to have an impact on clinical practice.
All authors acknowledge no financial support for the conduct of the research and/or preparation of the article.
Acknowledgements
The authors are grateful to Dr. Shindo, Director of the Department of Orthopedic Surgery of Wajinkai Hospital, for his whole-hearted cooperation and great encouragement in this endeavor.
References
- Grewal R, MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg Am 2007; 32: 962-970.
- Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist-anatomy and function. J Hand Surg Am. 1981; 6: 153-162.
- Friedman S, Palmer A. The ulnar impaction syndrome. Hand Clin. 1991; 7: 295-310.
- Czitrom AA, Dobyns JH, Linscheid RL. Ulnar variance in carpal instability. J Hand Surg Am 1987; 12: 205-208.
- Gelberman R, Salamon P, Jurist J, Posch J. Ulnar variance in Kienbock's disease. J Bone Joint Surg Am 1975; 57: 674-676.
- Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg Am 1982; 7: 376-379.
- Epner RA, Bowers WH, Guilford WB. Ulnar variance-The effect of wrist positioning and roentgen filming technique. J Hand Surg Am 1982; 7: 298-305.
- Yeh GL, Beredjiklian PK, Katz MA, Steinberg DR, Bozentka DJ. Effects of forearm rotation on the clinical evaluation of ulnar variance. J Hand Surg Am 2001; 26: 1042-1046.
- Pennock AT, Phillips CS, Matzon JL, Daley E. The effects of forearm rotation on three wrist measurements: radial inclination, radial height and palmar tilt. Hand Surg. 2005; 10: 17-22.
- Gartland JJ, Werley CW. Evaluation of healed Colles' fractures. J Bone Joint Surg Am 1951; 33-A: 895-907.
- Smiloviæ J, Biliæ R. Conservative treatment of extra-articular Colles' type fractures of the distal radius: prospective study. Croat Med J 2003; 44: 740-745.
- Jung JM, Baek GH, Kim JH, Lee YH, Chung MS. Changes in ulnar variance in relation to forearm rotation and grip. J Bone Joint Surg Br 2001; 83: 1029-1033.