ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2016) Volume 27, Issue 3
Relation between severity of hyponatremia and comorbidity in elderly patients who develop hyponatremia.
Nuket Bayram Kayar1, Yusuf Kayar2*, Iskender Ekinci2, Emrullah Duzgun Erdem2, Medine Ismailova2 and Dede Sit3
1Department of Family Medicine, Bagcilar Training and Research Hospital, Istanbul, Turkey
2Department of Internal Medicine, Bezmialem Vak?f University, Faculty of Medicine, Istanbul, Turkey
3Division of Nephrology, Department of Internal Medicine, Bagcilar Training and Research, Istanbul, Turkey
Accepted date: April 01, 2016;
Hyponatremia may affect every age group but it has a higher incidence among elderly. An increased prevalence of hyponatremia has been shown in the presence of comorbid condition, although very few studies include uptodate information on the relationship between severity of hyponatremia and comorbidity. The aims of our study are that; comorbid conditions in elderly inpatients diagnosed with hyponatremia and the relationship between hyponatremia severity and comorbid conditions. A total 978 patients aged 65 years and older admitted in hospital were considered for our study. 176 patients with serum sodium <135 mEg/L were included in the study. Sodium levels between 126-135 mEq/L were defined as mild, between 116-125 mEq/L as moderate and 115 mEq/L and below as severe hyponatremia. The relationships between severity of hyponatremia and comorbid conditions were examined. Patients’ mean age was 76.1 ± 7.2 years (65-95 years). Hyponatremia was significantly higher among women (female/male: 109/67; 61.6%/38.4%). 121 (68.7%) patients had mild, 41 (23.2%) had moderate and 14 (7.9%) had severe hyponatremia. 92 (52.2%) patients had diabetes mellitus, 130 (73.8%) had hypertension and 87 (49.4%) had chronic renal failure. A significant relationship was found between hyponatremia severity and ischemic and congestive heart diseases, neurological disorders, psychiatric disorders and thyroid dysfunction. In addition, mild hyponatremia decreased, moderate and severe hyponatremia increased with higher number of comorbidities. Comorbid conditions may cause hyponatremia through several mechanisms but severity of hyponatremia may differ. Hospitalizations, morbidity, mortality rates and healthcare expenses due to hyponatremia can be reduced with regular care of geriatric patients.
Keywords
Hyponatremia, Severity, Geriatric patients, Comorbidity.
Introduction
Hyponatremia is the most frequent electrolyte disturbances seen in clinical practice and is commonly described as serum sodium (Na) values below 135 mEq/L [1,2]. The exact prevalence and incidence is not known. While it is seen in 15-30% of hospitalized patients, more than 50% of the hyponatremic populations consists of hospitalized patients [3,4].
Although hyponatremia may affect all age groups, its incidence seems to be higher in the elderly individuals due to impaired response of fluid and electrolyte homeostasis to dietary and environmental changes [5]. Studies have shown that presence of coexisting comorbidities, physiological changes in glomerular filtration rate, altered water metabolism and polypharmacy were other explanations for the higher incidence of hyponatremia among the elderly [6-8].
Several studies have demonstrated an increased prevalence of hyponatremia in the presence of comorbid conditions [9-11]. However, there are a very few studies with uptodate information on the relationship between severity of hyponatremia and comorbidity. Previous studies involve contradictory results but they indicate significantly more severe hyponatremia in the presence of some comorbid conditions [12,13]. The purpose of our study was to determine the frequency of comorbid conditions in the hospitalized elderly patients diagnosed with hyponatremia and the relationship between severity of hyponatremia and comorbid conditions.
Material and Methods
A total 978 patients aged 65 years and above were evaluated in our study. One hundred and seventy-six elderly patients with serum sodium levels below 135 mEg/L at presented or decreased below 135 mEq/L during hospital stay were included in the study.
Patients’ age, sex, the time hyponatremia was diagnosed, any coexisting chronic conditions were documented. Patients’ duration of hospital stay and final outcome (improvement, death) were indicated. Patients were identified from determined sodium values of hospitalized patients, which were sent electronically from the chemistry department. Sodium values were determined with ion-selective electrodes (Hitachi 917, Roche, according to the manufacturer's instructions) and in all of these samples plasma osmolality and plasma glucose concentration were determined simultaneously. In all patients, the first step consisted of the exclusion of pseudo-hyponatraemia, through analysis of plasma osmolality, total protein, triglyceride and cholesterol concentrations. Patients were divided into groups according to the severity of hyponatremia. Sodium levels between 126 and 135 mEq/L were defined as mild, between 116 and 125 mEq/L as moderate and 115 mEq/L and below as severe hyponatremia [14].
Comorbid conditions in patients with hyponatremia were calculated as percentage. Number of comorbid conditions was indicated. The relationship between severity of hyponatremia and comorbid conditions was studied. The relationship between the number of comorbid conditions and severity of hyponatremia was also examined.
Statistical analysis
SPSS 22.0 software was used for statistical analysis of the data. The data were summarized as percentage, mean and standard deviation. Prevalence of hyponatremia and concomitant comorbidities in the hospitalized elderly inpatients were determined. Relationships between severity of hyponatremia and comorbid conditions, and between severity of hyponatremia and number of comorbid condition were studied using Mann Whitney U, independent T student, chi-square and Fischer’s exact tests. The results were evaluated using hazard ratio and 95% confidence interval. In these analyses, p values below 0.05 were considered statistically significant.
Result
A total of 978 patients aged 65 years and older that admitted in hospital were enrolled. Of the hospitalized patients, 530 (54%) had one or more electrolyte imbalance. Hyponatremia was detected in 176 (18%). The lowest Na was 98 mEq/L, the highest was 134 mEq/L and the mean Na was 125.9 mEq/L. 121 (68.7%) patients had mild, 41 (23.2%) had moderate and 14 (7.9%) had severe hyponatremia. Patients’ mean age was 76.1 ± 7.2 years (65-95 years); mean age of women was 75.8 ± 7.3 years (65-95 years) and mean age of men was 76.7 ± 7.2 years (65-92 years). Of the patients, 84 (47.7%) were aged 65-74 years, 66 (37.5%) were aged 75-84 years and 26 (14.8%) were aged 85 years and older. Hyponatremia was significantly more common among women (female/male: 109/67; 61.6% vs. 38.4%). Duration of hospital stay was minimum 1 day and maximum 50 days, with a mean duration of 9.9 days of hospital stay. Of the 176 patients diagnosed with hyponatremia, 113 (64.2%) were diagnosed at the time of hospitalization, while 63 (35.8%) patients developed hyponatremia following hospitalization. Of the patients diagnosed with hyponatremia, 145 (82.4%) were discharged from the hospital with improved, while 31 (17.6%) patients were died.
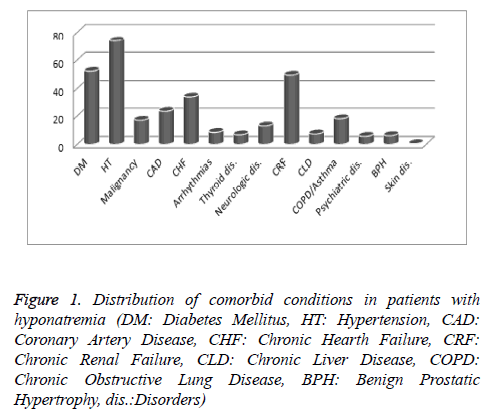
Patients diagnosed with hyponatremia were evaluated for coexisting comorbid conditions. Of the patients, 92 (52.2%) patients had Diabetes Mellitus (DM,) 130 (73.8%) had hypertension (HT), 30 (17%) had malignancies, 41 (23,3%) had Coronary Artery Disease (CAD), 60 (34%) had congestive heart failure (CHF), 87 (49.4%) had Chronic Renal Failure (CRF), 13 (7.4%) had Chronic Liver Disease (CLD), 32 (18.1%) had Chronic Obstructive Pulmonary Disease (COPD) or asthma, 10 (5.7%) had psychiatric disorders, 12 (6.8%) had thyroid dysfunction, 23 (13%) had neurological disorders, 15 (8.5%) had cardiac arrhythmias, 11 (6.2%) had Benign Prostatic Hyperplasia (BPH) and only 1 (0.5%) patient had chronic skin disease (Figure 1).
Figure 1: Distribution of comorbid conditions in patients with hyponatremia (DM: Diabetes Mellitus, HT: Hypertension, CAD: Coronary Artery Disease, CHF: Chronic Hearth Failure, CRF: Chronic Renal Failure, CLD: Chronic Liver Disease, COPD: Chronic Obstructive Lung Disease, BPH: Benign Prostatic Hypertrophy, dis.:Disorders)
The relationship between severity of hyponatremia and comorbid conditions were examined: There is no significant relationships were found between severity of hyponatremia and DM, HT, malignancy, CRF, COPD/asthma, CLD, cardiac arrhythmia and BPH but significant relationships were found between severity of hyponatremia and CHD, CHF, neurological disorders, psychiatric disorders and thyroid dysfunction. Mild hyponatremia was significantly lower and moderate hyponatremia was significantly higher in patients with CLD, compared to patients without CLD (Hazard ratio: 2.7, Cl 95%: 0.059-0.347, p<0.05). Mild hyponatremia was significantly lower and moderate hyponatremia was significantly higher in patients with CHF compared to patients without CHF (Hazard ratio: 2.5, Cl 95%: 0.045-0.373, p<0.05). Mild hyponatremia was significantly lower and moderate hyponatremia was significantly higher in patients with psychiatric disorders compared to patients without psychiatric disorders (Hazard ratio: 2.8, Cl 95%: 0.035-0.493, p<0.05).
Mild hyponatremia was significantly lower and moderate hyponatremia was significantly higher in patients with neurological disorders compared to patients without neurological disorders (Hazard ratio: 2.5, Cl 95%: 0.054-0.410, p<0.05). Mild hyponatremia was significantly lower and moderate hyponatremia was significantly higher in patients with thyroid dysfunction compared to patients without thyroid dysfunction (Hazard ratio: 2.6, Cl 95%: 0.029-0.211, p<0.05). The relationship between severity of hyponatremia and other comorbid conditions is presented in Table 1.
| Total | Mild hyponatremia | Moderate hyponatremia | Severe hyponatremia | P value | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| DM | |||||
| Positive | 92 (100) | 61 (66.3) | 26 (28.2) | 5 (5.5) | 0.18 |
| Negative | 84 (100) | 57 (67.9) | 17 (20.2) | 10 (11.9) | |
| Hypertension | |||||
| Positive | 130 (100) | 83 (63.8) | 34 (26.2) | 13 (10) | 0.26 |
| Negative | 46 (100) | 35 (76) | 9 (19.5) | 2 (4.5) | |
| Malignancy | |||||
| Positive | 30 (100) | 25 (83.3) | 5 (16.7) | 0 (0) | 0.67 |
| Negative | 146 (100) | 93 (64) | 38 (26) | 15 (10) | |
| CAD | |||||
| Positive | 41 (100) | 20 (48.7) | 16 (39) | 5 (12.3) | <0.05 |
| Negative | 135 (100) | 98 (72.6) | 27 (20) | 10 (7.4) | |
| CHF | |||||
| Positive | 60 (100) | 33 (55) | 21 (35) | 6 (10) | <0.05 |
| Negative | 116 (100) | 85 (73.3) | 22 (19) | 9 (7.7) | |
| CRF | |||||
| Positive | 87 (100) | 58 (66.6) | 22 (25.3) | 7 (8.1) | 0.95 |
| Negative | 89 (100) | 60 (67.4) | 21 (23.6) | 8 (9) | |
| CHD | |||||
| Positive | 13 (100) | 10 (77) | 3 (23) | 0 (0) | 0.49 |
| Negative | 163 (100) | 108 (66.2) | 40 (24.5) | 15 (9.3) | |
| COPD/Asthma | |||||
| Positive | 32 (100) | 21 (65.6) | 8 (25) | 3 (9.4) | 0.97 |
| Negative | 144 (100) | 97 (67.4) | 35 (24.2) | 12 (8.4) | |
| Psychiatric disorders | |||||
| Positive | 10 (100) | 3 (30) | 6 (60) | 1 (10) | <0.05 |
| Negative | 166 (100) | 115 (69.2) | 37 (22.3) | 14 (8.5) | |
| Thyroid dysfunction | |||||
| Positive | 12 (100) | 5 (41.6) | 7 (58.4) | 0 (0) | <0.05 |
| Negative | 164 (100) | 113 (69) | 36 (22) | 15 (9) | |
| Neurological disorders | |||||
| Positive | 23 (100) | 12 (52.1) | 6 (26.1) | 5 (21.8) | <0.05 |
| Negative | 153 (100) | 106 (69.3) | 37 (24.2) | 10 (6.5) | |
| Cardiac arrhythmia | |||||
| Positive | 15 (100) | 8 (53.4) | 4 (26.6) | 3 (20) | 0.22 |
| Negative | 161 (100) | 110 (68.3) | 39 (24.2) | 12 (7.5) | |
| BPH | |||||
| Positive | 11 (100) | 7 (63.6) | 3 (27.2) | 1 (9.2) | 0.96 |
| Negative | 165 (100) | 111 (67.3) | 40 (24.2) | 14 (8.5) |
(DM: Diabetes Mellitus, HT: Hypertension, CAD: Coronary Artery Disease, CHF: Chronic Hearth Failure, CRF: Chronic Renal Failure, CLD: Chronic Liver Disease, COPD: Chronic Obstructive Lung Disease, BPH: Benign Prostatic Hypertrophy)
Table 1: Relationship between severity of hyponatremia and comorbid conditions.
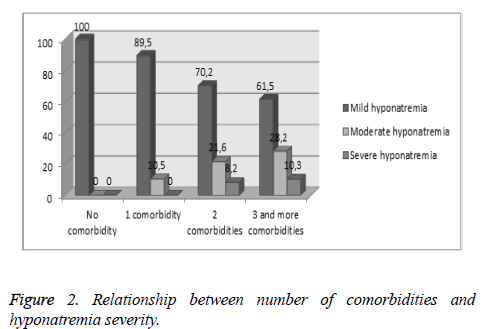
Three patients (1.7%) had no comorbid conditions, while 19 (10.7%) had one comorbid condition, 37 (21%) had two comorbid conditions and 117 (66.6%) had three or more comorbid conditions. The relationship between severity of hyponatremia and the number of comorbid conditions were examined; mild hyponatremia decreased, moderate and severe hyponatremia increased with higher number of comorbidities (Figure 2).
Discussion
Hyponatremia is the most common electrolyte disturbance in the geriatric population and among hospitalized patients [15]. Varying results are reported for the incidence and prevalence of hyponatremia due to the different variables examined like different age ranges and populations, values ranging from 2.5 to 30% have been reported from the previous studies [3]. In our study, hyponatremia was observed to develop in 18% of the geriatric population, consistent with the literature.
The leading cause to explain the higher frequency of hyponatremia in the geriatric population is coexisting comorbid conditions. In a study by Mohan et al. 51% of the patients diagnosed with hyponatremia had HT, 16% had DM, 17% had COPD, 15% had malignancies and 19% had psychiatric disorders, while 27% of then had no comorbid conditions [10]. In a study by Kang et al. 12.1% of the patients diagnosed with hyponatremia had cerebrovascular disorders, 21.6% had DM, 26.7% had CHD, 20.7% had CRF and 31% had malignancies [16]. DM, HT, CAD, CRF and malignancies were more common in our study compared to the other studies. Because only the geriatric population was examined.
Previous studies have demonstrated a relationship between hyponatremia and comorbid conditions [9,10]. In a study by Liamis et al. DM was significantly more common in patients diagnosed with hyponatremia (p<0.001), while a significant relation was not noted for hypertension and CHF [9]. Another study determined a significantly higher prevalence of hyponatremia in patients with HT, DM, CAD, malignancies, stroke, COPD and psychiatric disorders [10]. A few studies also demonstrated a significant relationship between severity of hyponatremia and comorbid conditions [12,13]. Bucher et al. demonstrated that hyponatremia was significantly more severe in patients with DM, CLD, CRF and malignancies [12]. On the other hand, in a study by Kovesdy et al. hyponatremia level was lower in subjects with CLD, CHF and depression but the authors noted no differences in other comorbid conditions [13]. In our study, patients with CAD, CHF, psychiatric disorders, neurological disorders and thyroid dysfunction had a higher frequency of moderate and severe hyponatremia. Comorbid conditions may cause hyponatremia through several mechanisms. CHF increases hyponatremia by stimulating nonosmotic Antidiuretic Hormone (ADH) [13]. The mechanism by which these drugs cause hyponatremia is believed to be the development of Syndrome of inappropriate antidiuretic hormone secretion (SIADH). However, it should be emphasized that low serum sodium levels in emotionally disturbed or psychotic patients may not be a direct consequence of these medications. Among the most frequent causes of hyponatremia in this population are the underlying psychosis itself and the compulsive water drinking [17]. SIADH Syndrome may develop due to neurological disorders and drugs taken for its treatment [17,18]. In addition, hyponatremia occurrence increases due to reduced GFR, reduced sodium reabsorption, increased ADH secretion and increased renal ADH sensitivity secondary to thyroid dysfunction [19]. We believe that the reasons of contradictory results from previous studies include age differences in subjects included in these studies, presence of other coexisting comorbidities, polypharmacy and differences in healthcare practices.
There are a very few studies examining the relationship between the number of comorbidities and prevalence of hyponatremia and severity of hyponatremia. A previous study has found a significantly higher prevalence of hyponatremia in patients with one or more comorbidities compared to patients without comorbidities [10]. In our study, the risk of developing moderate or severe hyponatremia were increased with increasing number of comorbid conditions (p<0.05).
Conclusion
Electrolyte disturbances are more common among the geriatric population due to increased incidence of chronic conditions. Given the increased frequency of coexisting comorbidities and polypharmacy, these patients should be monitored closely. Establishing more institutions to undertake the care of geriatric patients and training staff to be employed in these institutions may result in decreased hospitalization, morbidity, mortality rates and healthcare expenses due to hyponatremia.
References
- Smith MD, McKenna K, Thompson JC. Hyponatremia. ClinEndocrinol 2000;52:667-678.
- Schrier R.The patient withhyponatremiaor hypernatremia. In: Schrier RW, ed. ManualofNephrology.5thed. Philadelphia, PA: Lippincott Williams & Wilkins ; 2000:21-36.
- Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med 2006;119: 30-35.
- Hoorn EJ, Lindemans J, Zietse R. Development of severe hyponatraemia in hospitalized patients: Treatment-related risk factors and inadequate management. Nephrol Dial Transplant 2006;21:70-76.
- Clayton JA, Le Jeune IR, Hall IP. Severe hyponatraemia in medical in-patients: aetiology, assessment and outcome. QJ Med 2006;99:505-511.
- Fegan G, Begley J. Hyponatremia in the elderly. CME Geriatr Med 2005;7:76-85.
- Beck LH. The aging kidney. Defending a delicate balance of fluid and electrolyctes. Geriatrics 2000;55:26-28.
- Chua M, Hoyle GE, Soiza RL. Prognostic implications of hyponatremia in elderly hospitalized patients. Arc of Gerontol and Geriatrics 2007;45:253-258.
- Liamis G, Rodenburg EM, Hofman A, Zietse R, Stricker BH, Hoorn EJ. Electrolyte Disorders in Community Subjects: Prevalence and Risk Factors. Am J Med 2013;126:256-263.
- Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of Hyponatremia and Association with Mortality: Results from NHANES. Am J Med 2013;126:1127-1137.
- Vega J, Manríquez F, Madrid E. Hyponatremia on admission to the emergencyroom as a risk factor for hospital mortality. Rev Med Chile 2011; 139: 985-991.
- BucherC, Tapernoux D, Diethelm M. Influenceof weather conditions, drugs and comorbidities on serum Na and Cl in 13000 hospital admissions: evidence for a subpopulation susceptible for SIADH. ClinBiochem 2014;47:618-624.
- Kovesdy CP, Lott EH, Lu JL. Hyponatremia, Hypernatremia, and Mortality in Patients With Chronic Kidney Disease With and Without Congestive Heart Failure. Circulation 2012;125:677-684.
- Hawkins RC. Age and gender as risk factors for hyponatremia and hypernatremia. ClinChimActa 2003;337:169-172.
- CJ Thompson. Hyponatraemia: new associations and new treatments. Eur J Endocrinol 2010;162:1-3.
- Kang SH, Kim HW, Lee SY. Is the sodium level per se related to mortality in hospitalized patients with severe hyponatremia? ClinNephrol 2012;77:182-187.
- Liamis G, Milionis H, Elisaf M. A Review of Drug-Induced Hyponatremia. Am J Kidney Dis 2008;52:144-153.
- Robinson AG, Verbalis JG. Posterior Pituitary. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams Textbook of Endocrinology. 12thed. Philadelphia: Elsevier, 2011: 323.
- Basu G,Mohapatra A. Interactions between thyroid disorders and kidney disease. Indian J EndocrinolMetab2012;16:204-213.