ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2018) Volume 29, Issue 11
Relationship between awareness and use of nutrition labels and obesity
Sang Dol Kim*
Department of Nursing, College of Health Science, Kangwon National University, 346 Hwangjo-gil, Dogye-eup, Samcheok-si, Gangwon-do, Republic of Korea
- *Corresponding Author:
- Sang Dol Kim
Department of Nursing
College of Health Science
Kangwon National University, Republic of Korea
Accepted on April 13, 2018
DOI: 10.4066/biomedicalresearch.31-18-554
Visit for more related articles at Biomedical ResearchPurpose: This study aimed to identify the association between awareness and use of nutrition labels and obesity among Koreans.
Materials and Methods: A total of 16,911 participants aged ≥ 19 y (7,308 men and 9,603 women) were recruited. Data were extracted from the 6th Korea National Health and Nutrition Examination Survey (2014-2016). Logistic regression was used to identify the association between awareness and use of nutrition label and obesity prevalence.
Results: Awareness of nutrition labels was significantly associated with obesity prevalence when adjusted for gender, age, monthly family income, and marital status (Odds Ratios (OR) and 95% Confidence Interval (CI): 1.18, 1.07-1.30, P<0.05; 1.13, 1.00-1.27, P<0.05; 1.15, 1.05-1.26, P<0.001; and 1.17, 1.06-1.30, P<0.05, respectively). Use of nutrition labels was significantly associated with obesity prevalence when adjusted for age, educational level, monthly family income, and marital status (OR and 95% CI: 1.16, 1.05-1.28, P<0.05; 1.19, 1.07-1.31, P<0.05; 1.14, 1.02-1.27, P<0.05; and 1.19, 1.08-1.32, P<0.05, respectively).
Conclusion: Awareness and use of nutrition labels were significantly associated with obesity prevalence. These findings imply that education, dissemination, and publicity on understandable and useable nutrition labels are needed for food consumers, particularly to control obesity.
Keywords
Obesity, Nutrition assessment, Education.
Introduction
Obesity is a critical condition to be classified as a disease [1]. Obesity causes morbidity leading to chronic diseases and is associated with increased healthcare costs for management as well as treatment of obesity-related diseases, which may be associated with high mortality rates. Thus, obesity requires national-level management and prevention interventions [2-4]. Globally, several countries have confirmed the annual prevalence rate of obesity through national health nutrition surveys and tried to reduce its increasing prevalence.
The prevalence of obesity showed an increasing trend in the 2005-2014 National Health and Nutrition Survey in the United States, and Canada has been reported to have a dramatic increase in obesity and overweight over the last 20 years [2,3]. The prevalence of overweight and obesity is approximately 50% and 16%, respectively, in European populations [5]. Obesity is a risk factor of increasing prevalence and incidence of stroke in developed countries in Asia [6].
Factors influencing obesity are diverse and complex, with food intake being the most common [7-9]. Contemporary people prefer to use ingredients purchased outside the home rather than using their self-cultivated ingredients to prepare their meal. This instigates busy modern people to prefer fast food or instant food regardless of age and gender to save time and convenience of cooking. Furthermore, the proportion of people eating out is continuously increasing because of the rapid trend in modern urbanization due to global economic development. People who habitually eat out consume less calories and were unsatisfied; therefore, they resorted to purchasing instant ingredients to cook food, which has usually increased the access to unhealthy foods [7]. Food in restaurants is generally high in fat and calories [7]. Therefore, a healthy option strategy for food consumers is needed [7]. The strategy is generally associated with nutrition label marked calorie and nutrition of the food [10]. The food that we purchase should have nutrition labels. However, despite the presence of nutritional labeling of foods that provides important information for consumers’ food purchase and consumption, food buyers are unexpectedly indifferent to nutritional values and rarely use it, which may be a factor affecting obesity [7,8]. Therefore, the prevention and management strategy of obesity should be to reinforce consumers’ perception and use of nutrition labeling of foods [8]. Previous studies have investigated the predictors, strategies, impacts, and effectiveness on nutrition label use [7,8,11-21]. Studies on the factors associating nutrition labeling and obesity are limited. The relationship between awareness and use of nutrition labeling and obesity should be confirmed. Therefore, this study aimed to identify the association between awareness and use of nutrition labeling and obesity among Koreans based on their sociodemographic characteristics.
Materials and Methods
The data used in this study were extracted from the 6th Korea National Health and Nutrition Examination Surveys (KNHNES) (2013-2015), conducted by the Korea Centers for Disease Control and Prevention (KCDC) [22]. The 6th KNHNES covered three areas, i.e., health interviews, health examination, and nutritional survey. From 2013 to 2015, the 3- year data were stratified, clustered, and weighted to produce a complex sample plan file. Sampling weight for the complex sample plan file was allocated to every sample by integrated weighting values, such as health surveys (health screenings), nutrition surveys to ensure the representativeness of the sample. The 6th KNHNES was approved by the institutional review board of the KCDC (2013-07CON-03-4C, 2013-12EXP-03-5C) [22].
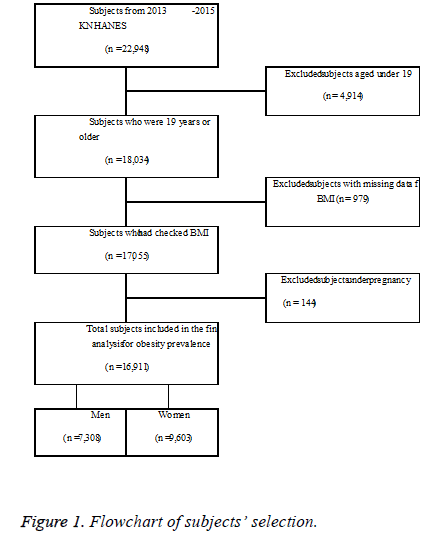
A total of 9,491 households and 22,948 participants were included. The gender ratio of participating household members was 45.4% for men and 54.6% for women. By age, 15.2% were in their 50s, 13.3% were >70 y old and 13.1% were in their 60s. Figure 1 shows the flowchart of subjects’ selection process. From 2013 to 2015, the total number of subjects was 22,948. Excluding 4,914 subjects who were <19 y old, 979 with missing Body Mass Index (BMI) data, and 144 who were pregnant, a total of 16,911 participants (7,308 men and 9,603 women) were finally included.
BMI was calculated by measuring the height and weight using portable stadiometers and electronic scale, respectively. The prevalence of obesity was calculated in participants aging ≥ 19 y, and pregnant women were excluded. BMI categories were divided based on the KNHNES BMI criteria: underweight (<18.5 kg/m2), normal weight (18.5-24.9 kg/m2), obese (≥ 25 kg/m2) [22].
Nutrition surveys were conducted by visiting households directly through an interview method. The following questions were asked to determine the nutrition labeling information: (i) “do you know the nutrition label?” and (ii) “do you read nutrition labels when buying or selecting processed foods?” These questions were answerable by “Yes or No.” The data analysis was conducted using the IBM SPSS program version 18.0 (SPSS Inc., and IBM Company, Chicago, IL). Descriptive statistics were used to determine the participants’ sociodemographic variables and rate of nutrition label awareness and use. Sampling weights were generated by considering complex sample design and non-response rate of the target population. Multiple logistic regression analysis was performed to evaluate the influence of the studied variables on the association between awareness and use of nutrition label and obesity prevalence. P-values<0.05 were considered statistically significant.
Results
Table 1 shows the general characteristics of participants in the 6th KNHANES. The mean age of participants aging ≥ 19 y was 46.4 ± 0.2 y. The gender ratio was 56.6% (women) vs. 43.4% (men). The percentage of above college graduates was 31.6%, and among the monthly household income, more than 3 million won was accounted for 47.5%. About 84.2% of the participants were single and 15.8% were married.
| Characteristics | (N (%) |
|---|---|
| Gender | |
| Men | 7,835 (43.4) |
| Women | 10,199 (56.6) |
| Age (y), mean (SE) | 46.36 (0.23) |
| 19-29 | 2,250 (12.5) |
| 30-39 | 2,946 (16.3) |
| 40-49 | 3,283 (18.2) |
| 50-59 | 3,499 (19.4) |
| 60-69 | 3,014 (16.7) |
| ≥ 70 | 3,042 (16.9) |
| Body mass index (kg/m2) | |
| BMI, mean (SE) | 23.79 (0.04) |
| Underweight (BMI<18.5) | 728 (4.3) |
| Normal weight (BMI ≥ 18.5, BMI<25) | 10,696 (62.7) |
| Obese (BMI ≥ 25) | 5,622 (33.0) |
| Education level | |
| ≤ Elementary | 3,683 (23.9) |
| Middle school | 1,640 (10.6) |
| High school | 5,225 (33.9) |
| >College | 4,876 (31.6) |
| Household income (Korea won/monthly) | |
| <100 | 3,096 (17.3) |
| 100-200 | 3,252 (18.2) |
| 201-300 | 3,047 (17.0) |
| >300 | 8,509 (47.5) |
| Marital status | |
| Single | 15,167 (84.2) |
| Married | 2,851 (15.8) |
Table 1. Sociodemographic and BMI distribution of participants (2014-2015).
Table 2 presents the associations between obesity prevalence and nutrition label awareness and use, respectively. These models are adjusted for potential confounding factors, such as gender, age, marital status, household income, and educational level. The prevalence of obesity was significantly associated with nutrition label awareness, and the obesity prevalence was 1.22 times higher in those who were unaware of nutrition label than those who were aware (OR 1.22, 95% CI 1.11-1.34, P<0.001). The confounding factors, such as gender, age, marital status, and household income, which were adjusted in the nutrition label awareness, were also significantly associated with obesity prevalence, with ORs and 95% CI of 1.18, 1.07-1.30, P<0.05; 1.13, 1.00-1.27, P<0.05; 1.15, 1.05-1.26, P<0.001; and 1.17, 1.06-1.30, P<0.05, respectively.
| Variables | Awareness | Use | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Unadjusted | 1.22 | 1.11-1.34 | <0.0001 | 1.2 | 1.09-1.33 | <0.0001 |
| Adjusted | ||||||
| Gender | 1.18 | 1.07-1.30 | 0.001 | 1.05 | 0.94-1.16 | 0.389 |
| Men | 1.66 | 1.53-1.80 | <0.0001 | 2.03 | 1.83-2.23 | <0.0001 |
| Women | 1 | Reference group | 1 | Reference group | ||
| Age | 1.13 | Reference group | 1.16 | 1.05-1.28 | 0.005 | |
| 19-29 | 1.00 | 1.00-1.26 | 0.044 | 1 | Reference group | |
| 30-39 | 1.57 | 1.34-1.84 | 0.448 | 1.56 | 1.33-1.84 | <0.0001 |
| 40-49 | 1.62 | 1.38-1.91 | 0.218 | 1.6 | 1.35-1.90 | 0.091 |
| 50-59 | 1.81 | 1.55-2.11 | 0.003 | 1.75 | 1.49-2.06 | 0.13 |
| 60-69 | 1.85 | 1.57-2.19 | 0.001 | 1.78 | 1.47-2.14 | 0.536 |
| ≥ 70 | 1.48 | 1.24-1.75 | 0.001 | 1.86 | 1.50-2.31 | 0.132 |
| Marital status | 1.15 | 1.05-1.26 | <0.0001 | 1.19 | 1.07-1.31 | 0.001 |
| Single | 1 | Reference group | 1 | Reference group | ||
| Married | 1.41 | 1.26-1.59 | <0.0001 | 1.44 | 1.27-1.64 | <0.0001 |
| Household income | 1.17 | 1.06-1.30 | 0.002 | 1.14 | 1.02-1.27 | 0.023 |
| (Korea wo/monthly) | ||||||
| <100 | 1.2 | 1.05-1.37 | 0.007 | 1.83 | 1.56-2.16 | <0.0001 |
| 100-200 | 1.18 | 1.04-1.33 | 0.008 | 1.42 | 1.18-1.71 | <0.0001 |
| 201-300 | 1.21 | 1.07-1.36 | 0.002 | 1.08 | 0.96-1.22 | 0.2 |
| >300 | 1 | Reference group | 1 | Reference group | ||
| Education level | 1.05 | 0.93-1.18 | 0.464 | 1.19 | 1.08-1.32 | 0.001 |
| ≤ Elementary | 1.55 | 1.35-1.77 | <0.0001 | 1.38 | 1.15-1.66 | 0.001 |
| Middle school | 1.38 | 1.18-1.61 | <0.0001 | 1.22 | 1.06-1.41 | 0.006 |
| High school | 1.08 | 0.96-1.20 | 0.176 | 1.22 | 1.06-1.40 | |
| >College | 1 | Reference group | 1 | Reference group | ||
These models are adjusted for potentially confounding factors including sex, age, marital status, household income, and education level.
Table 2. Association of nutrition label awareness and use with obesity by multiple logistic regression.
The prevalence of obesity was significantly associated with nutrition label use, which was 1.20 times higher on those who did not use nutrition label than those who used it (OR 1.20, 95% CI 1.09-1.33, P<0.001). The confounding factors, such as age, marital status, household income, and educational level, which were adjusted in the nutrition label use, were also significantly associated with obesity prevalence, with ORs and 95% CI of 1.16, 1.05-1.28, P<0.05; 1.19, 1.07-1.31, P<0.05; 1.14, 1.02-1.27, P<0.05; and 1.19, 1.08-1.32, P<0.05, respectively.
Discussion
Based on these findings, obesity prevalence was significantly associated with awareness of nutrition label, as well as with gender, age, marital status, and household income, adjusted for nutrition label awareness. These findings show that when the participants were unaware of the nutrition label, obesity prevalence was significantly higher among men, those with older age, the married, with lower household income, and lower educational level participants. Consistent with the present study, participants with obesity were more likely to check food labels than those with normal weight [14,19]. However, the check and use scores of nutrition labels were not different based on weight status [13]. It was found that women more likely understand nutrition labels than men. This finding is similar to a previous study’s results that women check nutrition label components more often than men [13].
Obesity prevalence was also significantly associated with nutrition label use, as well as with age, marital status, household income, and educational levels adjusted for nutrition label use. These findings show that when the participants do no use the nutrition label, obesity prevalence was significantly higher among the married, with low household income, and lower educational level participants. These findings support previous results that obese subjects did not significantly utilized food label [11]. Overweight participants were highly aware and used nutrition label than normal participants [19]. Unlike the present findings, the association between obesity and food label use was significantly low among participants with obesity than those with normal weight [13,14]. On the other hand, the association between understanding and use of nutrition label information and BMI was insignificantly correlated in six European countries [20]. Women prevalence was significantly associated with the use of nutrition label, age, marital status, household income, and educational level, adjusted for nutrition label use [13]. A review of literature reported that nutrition label use was significantly associated with nutritional knowledge [17]. As there is a saying that states knowledge is power, nutrition knowledge gives consumers an opportunity to become aware and appropriately use nutrition labels [17]. Therefore, obese subjects should be educated on the importance of understanding nutrition labels in order to determine accurate information. Further, appropriate use of nutrition labels should be promoted so that obese subjects can choose foods that are beneficial for their health. If food labels can greatly influence the public health, its rates of use should be increased among Koreans. A previous study suggested that food labels can effectively be used as a means of health prevention and the awareness of food label usefulness among all consumers should be raised [15]. A systematic review and meta-analysis findings suggested that nutrition labelling may be an effective approach to empowering consumers in choosing healthier products [16]. Another study suggested that food label was not commonly used among participants with inaccurate self-perception of body weight [14]. This means that body weight status was significantly associated with nutrition label awareness and use. Obesity is associated with adverse health consequences, which could be controlled by nutritional management and increased physical activity [23]. This study indicates that utilization rate was lower than the recognition rate of nutrition label, and obesity prevalence was significantly higher in participants who were unaware of and did not use nutrition label among Koreans. This study suggests that interventions increasing food label understanding and use should be developed and implemented. Furthermore, these findings imply that education, dissemination, and publicity on understandable and useable nutrition labels are needed for food consumers, particularly to control obesity. Further investigation is needed to determine the extent in which awareness and use of nutrition label effects obesity prevalence. Therefore, efforts should be made to determine how all consumers could use nutrition labels effectively. This study has the following strength. The association rates between nutrition label awareness and use and obesity prevalence have been confirmed by adjusting the sociodemographic variables to identify confounding variables. This provides an opportunity to develop and apply appropriate nutritional and educational interventions to manage obesity in the target groups. This study has two limitations. First, the question on whether the participants were aware of nutrition labels (“do you know the nutrition label?) is not specific. This question seems to be added to the expression “understand.” Second, BMI standards in assessing obesity differ according to countries, therefore, interpretation of obesity prevalence among Koreans should be considered.
In conclusion, awareness and use of nutrition labels were significantly associated with obesity prevalence. These findings could be used as evidence-based data for the prevention and management of obesity prevalence.
Acknowledgements
Data for this study were extracted from the 6th Korea National Health and Nutrition Examination Survey, 2015, conducted by the Korea Centers for Disease Control and Prevention.
Disclosure
No conflict of interest.
References
- Vallgarda S, Nielsen MEJ, Hansen AKK, Cathaoir KO, Hartlev M, Holm L. Should Europe follow the US and declare obesity a disease?: a discussion of the so-called utilitarian argument. Eur J Clin Nutr 2017; 71: 1263-1267.
- Campbell-Scherer D, Sharma AM. Improving obesity prevention and management in primary care in Canada. Curr Obes Rep 2016; 5: 327-332.
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016; 315: 2284-2291.
- Sharma AM1, Campbell-Scherer DL2. Redefining obesity: beyond the numbers. Obesity (Silver Spring) 2017; 25: 660-661.
- Marques A, Peralta M, Naia A, Loureiro N, de Matos MG. Prevalence of adult overweight and obesity in 20 European countries, 2014. Eur J Public Health 2018; 28: 295-300.
- Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke epidemiology in South, East, and South-East Asia: a review. J Stroke 2017; 19: 286-294.
- Talagala IA, Arambepola C. Use of food labels by adolescents to make healthier choices on snacks: a cross-sectional study from Sri Lanka. BMC Public Health 2016; 16: 739.
- Haidar A, Carey FR, Ranjit N, Archer N, Hoelscher D. Self-reported use of nutrition labels to make food choices is associated with healthier dietary behaviours in adolescents. Public Health Nutr 2017; 20: 2329-2339.
- Castro IRR. Obesity prevention and control: the urgent need for effective public policies. Cad Saude Publica 2017; 33.
- Bleich SN, Economos CD, Spiker ML, Vercammen KA, VanEpps EM, Block JP. A systematic review of calorie labeling and modified calorie labeling interventions: impact on consumer and restaurant behavior. Obesity (Silver Spring) 2017; 17.
- Satia JA. Galanko JA, Neuhouser ML. Food nutrition label use is associated with demographic, behavioral, and psychological factors and dietary intake among African Americans in North Carolina. J Am Diet Assoc 2005; 105: 392-402.
- Ollberding NJ, Wolf RL, Contento I. Food label use and its relation to dietary intake among US adults. J Am Diet Assoc 2010; 110: 1233-1237.
- Stran KA, Knol LL. Determinants of food label use differ by sex. J Acad Nutr Diet 2013; 113: 673-679.
- Chen X, Jahns L, Gittelsohn J, Wang Y. Who is missing the message? Targeting strategies to increase food label use among US adults. Public Health Nutr 2012; 15: 760-772.
- Viola GC, Bianchi F, Croce E, Ceretti E. Are food labels effective as a means of health prevention? J Public Health Res 2016; 5: 139-142.
- Cecchini M, Warin L. Impact of food labelling systems on food choices and eating behaviours: a systematic review and meta-analysis of randomized studies. Obes Rev 2016; 7: 201-210.
- Miller LM, Cassady DL. The effects of nutrition knowledge on food label use. A review of the literature. Appetite 2015; 92: 207-216.
- Fisher G. Nutrition labeling reduces valuations of food through multiple health and taste channels. Appetite 2017; 21: 120: 500-504.
- Lewis JE, Arheart KL, LeBlanc WG, Fleming LE, Lee DJ, Davila EP. Food label use and awareness of nutritional information and recommendations among persons with chronic disease. Am J Clin Nutr 2009; 90: 1351-1357.
- Grunert KG, Fernandez-Celemín L, Wills JM, Storcksdieck Genannt Bonsmann S, Nureeva L. Use and understanding of nutrition information on food labels in six European countries. J Public Health 2010; 18: 261-277.
- Persoskie A, Hennessy E, Nelson WL. US consumers understanding of nutrition labels in 2013: the importance of health literacy. Prev Chronic Dis 2017; 14: 86.
- Korea Centers for Disease Control and Prevention. The 6th Korea National Health and Nutrition Examination Survey 2015.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017; 390: 2627-2642.