ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2011) Volume 22, Issue 4
Role of plasma lactate and arterial blood gas as prognostic marker in Acute respiratory distress syndrome patients receiving mechanical venti-lation
Sunil Kumar Nanda and Hamsaveena Murthy
Department of Biochemistry, Sri Siddhartha Medical College, Agalakote, Tumkur 572107, Karnataka. India
- *Corresponding Author:
- Sunil Kumar Nanda
Department of Biochemistry
Sri Siddhartha Medical College
Agalakote, Tumkur 572107
Karnataka, India
Accepted date: June 10 2011
The present study was conducted to study the significance of lactate and arterial blood gas (ABG) as prognostic marker in patients admitted to intensive care unit receiving mechanical ventilation. This study was conducted on 50 critically ill patients between the age group of 20-60 years and 50 controls. Plasma lactate was determined among controls. Plasma lactate and ABG were determined among patients. Arterial blood gas analysis for pO2, pCO2 and pH was carried out among patients. Higher lactate, low pO2 and high pCO2 were observed among patients. Lactate was positively correlated with pCO2 and negatively with pO2 among patients. Patients developing hyperlactatemia during the course of intensive care unit treatment have poor prognosis. Lactate can be used as a prognostic tool in intensive care unit patients receiving mechanical ventilation.
Key words
Acute respiratory distress syndrome, Arterial blood gas, Hyperlactatemia, Lactate, multiple organ failure.
Introduction
Patients receiving mechanical ventilation have a poor prognosis. The prognosis of the patients receiving mechanical ventilation is highly unpredictable. Clinical parameters like pulse rate and blood pressure cannot predict the prognosis in these patients. The cause for mortality in these patients is mainly multiple organ failure. The cause for multiple organ failure is occult hypoxia [1]. Plasma lactate levels may be used as a surrogate marker of tissue hypoxia in critically ill patients. Few studies indicate increased lactate levels in patients receiving mechanical ventilation while some studies indicate that there was no significant relation between lactate levels and severity of lung disease [2]. The aim of this study was to determine lactate and ABG as prognostic tool in critically ill patients.
Materials and Methods
This study was conducted at J.S.S. Medical College and Hospital, Mysore. The patient group included Acute respiratory distress syndrome patients receiving mechanical ventilation between the age group of 20-60 years [38 males and 12 females]. Patients with diabetes mellitus and who were on medications causing hyperlactatemia at the time of admission were excluded from the study. The control group consisted of 50 age and sex matched, normal healthy volunteers (38 males and 12 females) without any systemic illnesses or any chronic diseases and who were not on any medications causing hyperlactatemia. The study was conducted after informed consent was obtained from them and the study has been approved by the ethical committee of the institution. 4 ml of venous blood drawn aseptically was immediately placed in oxalate fluoride tubes, put on ice, and centrifuged for 10 min at 3,000 rpm. The lactate concentration was determined on each plasma sample. Lactate was determined by lactate oxidase method [3] using RX Daytona Randox Auto analyzer. Lactate is oxidized by the enzyme lactate oxidase to give pyruvate and hydrogen peroxide. In the presence of peroxidase, hydrogen oxidatively couples with 4 amino antipyrine and Nethyl-N-2 hydroxy-3-sulphopropyl mtoluidine to produce purple coloured complex which is measured at 550 nm, the intensity of the colour formed is directly proportional to the concentration of lactate in the sample. Arterial blood gas analysis using AVL Compact 3 analyzer for pO2, pCO2 and pH was carried out on the arterial blood samples from the patients collected in a sodium heparin syringe [4].
Statistical Analysis
Statistical comparisons were carried out using student’s ‘t’ test. All the statistical operations were done through SPSS for Windows (Version 15 evaluation version, 2006), SPSS Inc. New York.
Results
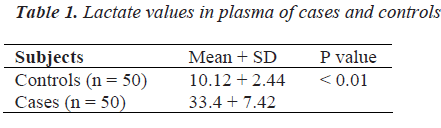
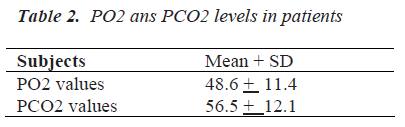
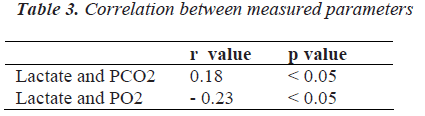
Patients receiving mechanical ventilation had higher lactate 33.4 + 7.42 mg/dl compared to controls 10.12 ± 2.44 mg/dl [p < 0.05] [Table 1], low pO2 46.6 ± 11.4 mm Hg and high pCO2 56.5 ± 12.1 were observed among the patients [Table 2]. Positive correlations were observed between lactate and pCO2 (r = 0.18, p < 0.05) among the patients. Negative correlations were observed between lactate and pO2 (r = - 0.23, p < 0.05) among the patients. These correlations were statistically significant [Table 3].
Discussion
Determination of pCO2, and plasma lactate concentration may be useful as metabolic markers of tissue hypoxia [8]. ARDS is characterized by severe acute injury, directly or indirectly via the blood, to the endothelial and epithelial surfaces of the lung leading to noncardiogenic respiratory failure [1]. Some studies demonstrated hyperlactatemia in patients with ARDS which is proportional to the severity of the lung injury and few studies indicate that there is no significant relation between lactate levels and severity of lung disease [9, 10]. Hyperlactatemia may be caused by an inadequate tissue perfusioninduced oxygen debt on exposure to endotoxin, inhibition of pyruvate dehydrogenase activity and increased anaerobic glycolysis, which would lead to pyruvate and lactate accumulation in the cell, deranged oxidative phosphorylation with consequent spillage of excess lactate into the circulation causing increase in blood lactate level [11]. In the present study, the patients demonstrated hyperlactatemia which is increasing with the progression of septic shock with ARDS. Although ABG measurement serves as prognostic marker as well as to guide resuscitation or therapy in patients of septic shock with ARDS [15], its measurement requires an arterial puncture or placement of an indwelling arterial catheter which has been associated with significant pain and complications such as infection, pseudoaneurysm, distal embolization [16]. Thus, the early serial measurement of lactate as a biomarker may serve as an independent noninvasive prognosticator of the disease outcome in septic shock with ARDS providing equivalent information to the arterial blood gas analysis and may be used as an alternative predictive marker or guide to resuscitation. . Out of the 50 patients, 28 patients recovered after receiving mechanical ventilation. Remaining 22 patients developed multiple organ failure.
References
- Andres E, Antonia A, Fernando F. Outcome of older patients receiving mechanical ventilation. Intensive Care Medicine 2004; 30(4): 639- 646.
- Leverve XM, Mustafa I. Lactate. A key metabolite in the intercellular metabolic interplay. Crit Care 2002; 6(4): 284-285,
- David B Sacks. Carbohydrates. In: Burtis AC, Ashwood RE, editors. Tietz text book of clinical chemistry 4th edn: Philadelphia: Saunders; 2006: 837-901.
- Mitchell GS, James SK. Electrolytes and blood gases. In; Burtis AC, Ashwood RE, editors. Tietz textbook of clinical chemistry 4th edn: Philadelphia: Saunders; 2006: 983-1018.
- Caples SM, Hubmayr RD. Respiratory monitoring tools in the intensive care unit. Curr Opinion in Crit Care 2003; 9(3): 230-235.
- Siggaard-Andersen O, Wimberly PD, Fogh-Andersen N, Gothgen IH. Measured and derived quantities with modern pH and blood gas equipment: calculation algorithms with 54 equations. Scand J Clin Lab Invest 1988; 48 (189): 7-15.
- Figge J, Jabor A, Kazda A, Fencl V. Anion gap and hypoproteinemia. Crit Care Med 1998; 26(11): 1807-1810.
- Gutierrez G, Wulf-Gutierrez ME, Reines HD. Monitoring oxygen transport and tissue oxygenation. Curr Opinion in Anaesthesiol 2004; 17(2): 107-117.
- Routsi CS, Zakynthinos H, Bardouniotou D, Alepopou-lou E, Zakynthinos D, Kazi B, Ioanidou, Roussos C. Arteriovenous differences in lactate and lactate pyruvate ratio correlate with hypoxemic lung disease. Am J Respir Crit Care Med 1996; 153 (5): A385.
- Backer D, Creteur J, Zhang H, Norrenberg M, Vincent JL. Lactate Production by the Lungs in Acute Lung Injury. Am J Respir Crit Care Med 1997; 156 (4): 1099-1104.
- Kilpatrick-Smith L, Erecinska M. Cellular effects of endotoxin in vitro: I. Effect of endotoxin on mitochondrial substrate metabolism and intracellular calcium. Circ Shock 1983; 11 (2): 85-99.
- Rhodes A, Cusack RJ. Arterial blood gas analysis and lactate. Curr Opinion in Crit Care 2000; 6 (3): 227-231.
- Rocktaeschel J, Morimatsu H, Uchino S, Bellomo R. Unmeasured anions in critically ill patients: can they predict mortality? Crit Care Med 2003; 31(8): 2131-2136.
- Smith I, Kumar P, Molloy S, Rhodes A, Newman PJ, Grounds RM, Bennett ED. Base excess and lactate as prognostic indicators for patients admitted to intensive care. Inten Care Med 2001; 27 (1): 74-83.
- Eachempati SR, Reed RL, Barie PS. Serum bicarbonate concentration correlates with arterial base deficit in critically ill patients. Surg Infect (Larchmt) 2003; 4 (2): 193-197.
- Crawford A. An audit of the patient?s experience of arterial blood gas testing. Br J Nurs 2004; 13(9): 529-532.