ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 2
Selection of surgical approach for the treatment of bilateral thyroid carcinoma
Department of Thyroid Surgery, China-Japan Union Hospital of Jilin University, Changchun 130033, China
- *Corresponding Author:
- Hui Sun
Department of Thyroid Surgery
China-Japan Union Hospital
Jilin University, Changchun 130033, China
Accepted date: July 25, 2016
This study aims to summarize the clinical features of bilateral thyroid carcinoma as well as to discuss the surgical approaches for its treatment. We analyzed 1999 cases of primary differentiated thyroid carcinoma surgery, of which 556 cases were of bilateral thyroid carcinoma. The age, tumor size, lymph node metastasis of bilateral thyroid cancer was analyzed. Primary bilateral thyroid carcinoma accounted for 27.8% of the cases with a male to female ratio of 1:4.7. Mean age of patients was 42.58 ± 9.07 years. Total or near-total thyroidectomy and routine central lymph node dissection were performed for the treatment of bilateral thyroid carcinoma. Bilateral microcarcinoma accounted for 66.3% of the cases, while the proportion of T1 patients accounted for 88.8%, with a maximum tumor diameter larger than that in unilateral thyroid carcinoma (bilateral 1.01 ± 0.73 cm; unilateral 0.89 ± 0.73 cm; P=0.002). Metastasis rate of central lymph node was significantly higher than that in unilateral thyroid carcinoma (bilateral 214/499, 42.9%; unilateral 370/1195, 31.0%; P<0.01). The metastasis rate in men was higher than that in women, and the central lymph node metastasis rate gradually decreased with increasing age. Observed cases of increased mass volume were accompanied by a significant increase in central and lateral cervical lymph node metastasis rate. Bilateral thyroid carcinoma has been commonly observed mainly in T1 stage tumors, exhibiting higher invasiveness and aggressiveness than unilateral thyroid carcinoma. In these cases, total or near total thyroidectomy is recommended. Surgeons should aim to avoid inducing hypoparathyroidism owing to surgical loss of parathyroid tissue, while protecting the recurrent laryngeal nerve. Prophylactic cervical dissection indications should be broadened for female patients with tumor diameter >1 cm or age <50 years.
Keywords
Thyroid carcinoma, Total thyroidectomy, Parathyroid, Surgical treatment.
Introduction
In recent years, the incidence of thyroid cancer significantly increased. According to the 2012 Chinese Cancer Registry Annual Report, thyroid cancer ranks fourth among the top 10 cancers with an annual growth rate of 14.51% from 2003 to 2007 [1]. It has therefore been the focus of clinicians [2]. In Italy, thyroid cancer has become the second most common cancer in women younger than 45 years of age [3]. In Korea thyroid cancer increased rapidly, by 22.3% per year in both sexes, and has been the most common cancer since 2009 [4]. Thyroid cancer has become one of the major diseases threatening the health of the female population. According to statistics, bilateral thyroid cancer accounted for 12~43% cases [5-7], and our data showed that double thyroid cancer accounted for 27.8%. It is further reported that if the resected thyroid specimens are subjected to continuous biopsy for pathological examination, the incidence of bilateral thyroid cancer could be up to 61%-87.5% [8,9]. Surgery is the first choice of treatment for thyroid cancer with thyroid lobectomy, and total or near total thyroidectomy as the mainstream treatment. Total or near total thyroidectomy is the main treatment option for bilateral thyroid cancer. Bilateral thyroid cancer is a multifocal thyroid cancer, and multifocality is one of the important factors influencing prognosis [10]. Analysis of the clinical data for bilateral thyroid carcinoma, and the identification of its clinical features, will help choose the most suitable surgical approach, which can lead to a standardized treatment with lower recurrence rates. For this purpose, data from 1999 patients diagnosed with differentiated thyroid carcinoma who underwent primary thyroid surgery between June 2008 and December 2011 was analyzed, including 556 cases of bilateral thyroid carcinoma among the 1999 patients.
Materials and Methods
Subjects
We analyzed 1999 patients diagnosed with differentiated thyroid carcinoma who underwent primary thyroid surgery between June 2008 and December 2011, and among that cases, there were 556 cases diagnosed with bilateral thyroid carcinoma, including 97 males, and 459 females, with a male to female ratio of 1:4.7 and an occurrence between 18-70 years of age (mean: 42.58 ± 9.07). This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of China- Japan Union Hospital of Jilin University. Written informed consent was obtained from all participants.
Selection standard
All cases were 1) differentiated thyroid carcinoma; 2) primary surgery treatment; 3) thyroid carcinoma diagnosed by intraoperative frozen slice pathology; 4) without a history of other malignant disease of the neck; 5) without neck radiation treatment; 6) bilateral thyroid carcinoma defined as bilateral tube carcinoma or with the presence of unilateral and isthmic carcinoma.
Surgical treatment
Unilateral thyroid carcinoma cases were treated with gland and isthmus resection, or with contralateral lobe subtotal resection. A small number of cases with failed rapid pathological intraoperative diagnosis underwent subtotal thyroidectomy. Cases with clear diagnosis of bilateral thyroid carcinoma were treated with total or near total thyroidectomy, and few cases with failed intraoperative rapid pathological diagnosis were treated in accordance with unilateral thyroid cancer treatment or benign thyroid disease. We dissected the recurrent laryngeal nerve during the whole resection, and intraoperative recurrent laryngeal nerve monitoring (IONM) was selectively performed. A sophisticated technology was used for the protection of parathyroid outer coating; upper parathyroid was preserved in situ and to protect the surrounding blood supply, a small amount of fat tissue around the gland was left. Inferior parathyroid glands were preserved in situ without affecting central lymph node dissection and its blood supply. If the blood supply was identified to be poor, parathyroid transplantation within the sternocleidomastoid was performed. Routine intraoperative PTH rapid detection of bilateral thyroid cancer is imperative. Upon detection of a significant decrease in the PTH, blood supply should be checked and tissue resected again, and transplantation should be performed within the sternocleidomastoid if necessary.
For cervical lymph node dissection, central lymph node dissection was commonly performed except in few early cases where knowledge was limited. Patients with masses larger than 1 cm or those with obvious lateral neck lymph node swellings underwent elective lymph node dissection (VI, IIA, III, IV). If cervical lymph node metastasis was found, whole neck dissection was performed (VI, II, III, IV, V). All cases showed no lymph node metastasis in I area.
Postoperative treatment and follow-up
All cases were treated with L-thyroxine after surgery. In low risk cases, TSH level was maintained at 0.2~0.5; whereas in high risk cases it was maintained at lower than 0.1. I131 treatment was administered if cervical lymph node metastasis was found and total or near total resection was performed. Patients were followed up at the clinic or over the telephone every 3-6 months.
Statistical method
Continuous variables were presented as mean + standard deviation (SD) and compared by t-test or one-way ANOVA among groups. While the frequency distributions of categorical variables among groups were presented with number (proportion) and compared by Pearson χ2 test. The Hardy– Weinberg equilibrium for each variant was assessed by Pearson χ2 test. A two-tailed P value of <0.05 was considered statistically significant. SAS for Windows version 9.1 (SAS Institute Inc., Cary, NC) was used for all statistical analyses.
Results
Surgical approach
Unilateral thyroid carcinoma cases were treated with unilateral lobectomy and isthmus resection, or with contralateral lobe subtotal resection or total thyroidectomy. Two of the bilateral thyroid carcinoma cases underwent bilateral subtotal resection due to a suspected malignancy during intraoperative rapid pathological assessment. When the results of the intraoperative rapid pathological assessment were unclear, 41 bilateral unilateral thyroid cancer cases including 11 cases of suspicious thyroid cancer, 9 cases of atypical hyperplasia, and 21 cases of malignant pathologies discovered accidentally on the other side of the lobe, were accepted as unilateral carcinomas, and treated with unilateral lobectomy plus contralateral lobe subtotal resection. The remaining 513 cases underwent thyroid neartotal or total thyroidectomy. Central lymph node dissection rate was 84.7% (1694/1999). The central group lymph node dissection rate of bilateral thyroid cancer was 89.8% (499/556). Lateral neck dissection was performed for 1416 cases (70.8%) and bilateral thyroid cancer neck dissection for 446 cases (80.2%, 446/556), 199 of which underwent bilateral neck dissection (35.8%).
Clinical pathology statistics
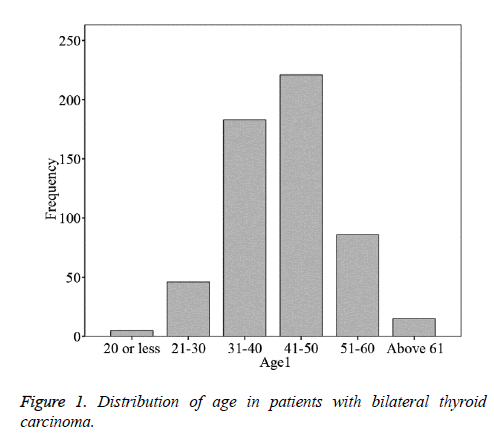
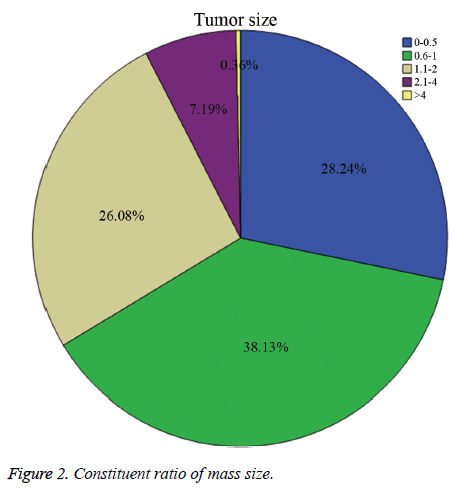
Bilateral differentiated thyroid carcinoma cases were mostly diagnosed as papillary carcinomas with only two patients diagnosed as unilateral follicular carcinoma. Bilateral thyroid cancer accounts for 27.8% of primary thyroid cancer cases, with significantly less occurrence in males in comparison to females. No significant difference was observed among males and females diagnosed with unilateral thyroid cancer (P=0.166). Bilateral thyroid carcinoma had a higher incidence in the 30-50 years age group (Figure 1), with an average age of 42.58 ± 9.07 years, and no difference was found when compared with unilateral thyroid carcinoma (42.90 ± 9.51, P=0.494) (Table 1). The maximum tumor diameter of bilateral thyroid cancer was greater than that of unilateral thyroid cancer (bilateral 1.01 ± 0.73 cm; unilateral 0.89 ± 0.73 cm; P=0.002). Bilateral thyroid microcarcinoma accounted for 66.3% of the cases, and T1 stage accounted for 88.8% (Figure 2). The central cervical lymph node metastasis rate for bilateral thyroid cancer (214/499, 42.9%) was significantly higher than unilateral thyroid cancer (370/1195, 31.0%, P<0.01). Central lymph node metastasis rate of males was significantly higher than that of females (Table 2), and this rate was significantly reduced (Table 3) with increasing age. A significant increase in both central and lateral lymph node metastasis rates were observed with increasing mass (Tables 4 and 5).
| Unilateral | Bilateral | P value | ||
| Cases (n) | 1443 | 556 | ||
| Age (year old) | 42.90 ± 9.51 | 42.58 ± 9.07 | 0.494 | |
| Sex | Male | 292 | 97 | 0.166 |
| Female | 1151 | 495 | ||
| Diameter (cm) | 0.89 ± 0.73 | 1.01 ± 0.73 | 0.002 | |
| Lesion number | Unifocus | 1303 (90.3%) | 0 | |
| Multifocus | 140 (9.7%) | 556 (100%) | ||
| Central lateral lymph node metastasis | Metastasis | 370 (31.0%) | 214 (42.9%) | 0 |
| (unilateral=1195, bilateral=499) | No metastasis | 825 (69.0%) | 285 (57.1%) | |
Table 1: Clinical data of bilateral or unilateral thyroid carcinoma.
| Central lateral Lymph node Metastasis | Sex | Total | |
| Male | Female | ||
| No metastasis | 35 | 250 | 285 |
| 0.389 | 0.611 | 0.571 | |
| Metastasis | 55 | 159 | 214 |
| 0.611 | 0.389 | 0.429 | |
| Total | 90 | 409 | 499 |
Table 2: Sex in relation with central lateral lymph node metastasis in cases of bilateral thyroid carcinoma.
| Central Lateral Lymph Node Metastasis | Age (year old) | Total | |||||
| <20 | 21-30 | 31-40 | 41-50 | 51-60 | >61 | ||
| No metastasis | 7 | 43 | 352 | 464 | 213 | 31 | 1110 |
| 0.368 | 0.309 | 0.612 | 0.716 | 0.78 | 0.775 | 0.655 | |
| Metastasis | 12 | 96 | 223 | 184 | 60 | 9 | 584 |
| 0.632 | 0.691 | 0.388 | 0.284 | 0.22 | 0.225 | 0.345 | |
| Total | 19 | 139 | 575 | 648 | 273 | 40 | 1694 |
Table 3: Age in relation with central lateral lymph node metastasis in cases of bilateral thyroid carcinoma.
| Central lateral Lymph node Metastasis | Mass diameter (cm) | Total | ||||
| 0-0.5 | 0.6-1 | 1.1-2 | 2.1-4 | >4 | ||
| No Metastasis | 104 | 113 | 58 | 10 | 0 | 285 |
| 0.754 | 0.592 | 0.439 | 0.278 | 0 | 0.571 | |
| Metastasis | 34 | 78 | 74 | 26 | 2 | 214 |
| 0.246 | 0.408 | 0.561 | 0.722 | 1 | 0.429 | |
| Total | 138 | 191 | 132 | 36 | 2 | 499 |
Table 4: Bilateral masses size in relation with central lateral lymph node metastasis in cases of bilateral thyroid carcinoma.
| Right side Lateral Lymph Node Metastasis | Mass diameter (cm) | Total | ||||
| 0-0.5 | 0.6-1 | 1.1-2 | 2.1-4 | >4 | ||
| No metastasis | 64 | 71 | 61 | 13 | 0 | 209 |
| 0.81 | 0.657 | 0.56 | 0.433 | 0 | 0.637 | |
| Metastasis | 15 | 37 | 48 | 17 | 2 | 119 |
| 0.19 | 0.343 | 0.44 | 0.567 | 1 | 0.363 | |
| Total | 79 | 108 | 109 | 30 | 2 | 328 |
Table 5: Mass size in relation with right side lateral lymph node metastasis.
Postoperative complications
In the cases of unilateral thyroid carcinoma, temporary (laryngoscopy) vocal cord paralysis occurred in 7 cases, with no permanent vocal cord paralysis except in case of tumor invasion or recurrent laryngeal nerve resection. In the cases of bilateral thyroid carcinoma, vocal cord paralysis occurred in 6 cases with no permanent vocal cord paralysis. Transient hypocalcemia was observed in 14 cases of unilateral thyroid carcinoma and temporary hypocalcemia in 18 cases of bilateral thyroid cancer. In cases of permanent hypocalcemia, 1 cases were unilateral and 4 case were bilateral thyroid carcinoma with no significant statistical difference. Hypocalcemia patients were treated with oral vitamin D and calcium (900-1800 mg/d), and no significant numbness or convulsions were recorded.
Follow-up results
Follow-up time ranged from 3-5 years, and follow-up rate was 92%. Thyroid function control was established 1-4 months following surgery via treatment with oral Euthyrox. Central lymph node recurrence was observed in 3 cases without early central group lymph node dissection. Recurrence occurred in 1 case of leftover lobe after unilateral lobectomy and contralateral subtotal lobectomy, which necessitated secondary surgical treatment.
Discussion
Thyroid cancer is the most common clinical endocrine tumor. Most bilateral thyroid cancers reported in the literature were rare, but our data show that bilateral thyroid cancer patients accounted for 27.8%. High incidence of bilateral thyroid cancer occurrence was observed between 30 and 50 years of age. Our data showed an average age of 42.58 ± 9.07 years, with no significant difference in comparison to unilateral thyroid cancer. Most bilateral thyroid cancers were papillary microcarcinomas accounting for 66.3%, and T1 stage accounted for 88.8%, slightly less than the 70.1% in unilateral thyroid cancer cases. The average tumor diameter was 1.01 ± 0.73 cm, and larger than unilateral thyroid cancer, probably due to multifocality. Multifocal invasive thyroid cancer grows rapidly [11-13]. Mainly, two multifocal forms of thyroid cancer, one originating from the lesion within the gland metastasis, and the other independently originating multifocal tumor, have evolved. Various studies showed that both forms exist at the same time, which explains the inconsistencies in clinical data obtained using different methods and from different regions. Other literature associates multifocal thyroid cancer growth and faster invasion with high expression of Ki-67 and Cyclin D1, which promote cell proliferation [14-17].
Surgical treatment should aim at avoiding re-operation and reducing complications (recurrent laryngeal nerve and parathyroid injury). A unified view on the treatment of bilateral thyroid cancer is total thyroidectomy or near total thyroidectomy. For bilateral lobes foci, total thyroidectomy is appropriate. For unilateral foci plus isthmus foci, thyroid near total resection is suitable. Bilateral thyroid cancer occurred rapid proliferation, metastasis and invasion within the gland, prone to cervical lymph node metastasis, for which bilateral central lymph node metastasis accounts for 42.9%, significantly higher than the unilateral thyroid cancer. Therefore, resection of all possible foci to reduce recurrence rate is necessary. Recurrence was observed only in 1 patient following subtotal lobectomy. Furthermore, total thyroidectomy would benefit Tg and 131I monitoring for recurrence, and would be beneficial for patients with metastases that occur after 131I therapy. For cases of unilateral foci and isthmus, lobectomy and isthmusectomy were performed, and if feasible, total or near total thyroidectomy was performed. The drawback of near-total resection is the limitation of early I131 monitoring for recurrence. Some scholars have suggested that lateral lobe resection or subtotal resection is feasible for small unilateral lesions as well as bilateral thyroid cancer, mainly to reduce the recurrent laryngeal nerve and parathyroid damage. Thyroid surgery is also performed as recurrent laryngeal nerve and parathyroid surgery. Extent of surgery should be based on tumor staging and prognostic factors. Quality and complications of surgery depend on the surgeon's skill and experience. Scholars consider that after total or near total resection, the recurrent laryngeal nerve and parathyroid temporary injury rates are greater than those observed in subtotal thyroidectomy, with no significant increase in permanent damage [18]. Our data confirmed this point.
Neck dissection is accepted as the surgical choice for CN+ patients. On the other hand, prophylactic dissection in central area gradually became routine procedure, especially for bilateral thyroid cancer in CN0 patients. Bilateral thyroid cancers display invasiveness and metastases significantly higher than unilateral thyroid cancers, and multiple reports of higher expression of TGF-β1 and MMP-2 in multifocal PTC also confirmed this point [19-21]. Clinical data show that in bilateral thyroid cancer cases, lymph node metastasis rate was 42.9%, which is significantly higher than unilateral thyroid cancer (31.0%). Also, a higher number of males, and a tumor diameter greater than 1 cm with increased lateral neck lymph node metastases were observed. Lymph node metastasis rate was gradually reduced with increasing age. For CN0 patients, tumor masses greater than 1 cm or male patients younger than 50 years of age should be treated actively with prophylactic neck dissection to reduce reoperation rate.
Bilateral thyroid carcinoma is not clinically uncommon. Increased mass volume was accompanied by a significant increase in central and lateral cervical lymph node metastasis rate. Bilateral thyroid carcinoma exhibits higher invasiveness and aggressiveness than unilateral thyroid carcinoma. Total thyroidectomy or near total resection should be performed. Surgeons should aim to avoid inducing hypoparathyroidism owing to surgical loss of parathyroid tissue, while protecting the recurrent laryngeal nerve. Prophylactic cervical lymph node resection indications should be appropriately widened. TSH suppression therapy should be administered postoperatively and a close follow-up schedule should be in place.
References
- Liu YQ, Zhang SQ, Chen WQ, Chen LL, Zhang SW, Zhang XD, Zheng RS. Trend of incidence and mortality on thyroid cancer in China during 2003-2007. Zhonghua Liu Xing Bing Xue Za Zhi 2012; 33: 1044-1048.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012; 62: 10-29.
- Dal Maso L, Lise M, Zambon P, Falcini F, Crocetti E, Serraino D, Cirilli C, Zanetti R, Vercelli M, Ferretti S, Stracci F, De Lisi V, Busco S, Tagliabue G, Budroni M, Tumino R, Giacomin A, Franceschi S. Incidence of thyroid cancer in Italy, 1991-2005: time trends and age-period-cohort effects. Ann Oncol 2011; 22: 957-963.
- Jung KW, Won YJ, Kong HJ, Oh CM, Cho H. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat 2015; 47: 127-141.
- Hwang E, Pakdaman MN, Tamilia M, Hier MP, Black MJ, Rochon L, Payne RJ. Bilateral papillary thyroid cancer and associated histopathologic findings. J Otolaryngol Head Neck Surg 2010; 39: 284-287.
- Connor MP, Wells D, Schmalbach CE. Variables predictive of bilateral occult papillary microcarcinoma following total thyroidectomy. Otolaryngol Head Neck Surg 2011; 144: 210-215.
- Pasieka JL, Thompson NW, McLeod MK, Burney RE, Macha M. The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg 1992; 16: 711-716.
- Katoh R, Sasaki J, Kurihara H, Suzuki K, Iida Y. Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma. A clinicopathologic study of 105 consecutive patients. Cancer 1992; 70: 1585-1590.
- Clark RL, White CE, Russel WO, Ibanez ML. Clinicopathologic studies in 218 total thyroidectomies for thyroid cancer. Arq Patol 1966; 38: 25-29.
- Prescott JD, Parangi S. Bilaterality in papillary thyroid carcinoma: does it influence prognosis? Ann Surg Oncol 2012; 19: 1-2.
- Kim JY, Jung EJ, Jeong SH, Jeong CY, Ju YT, Lee YJ, Hong SC, Choi SK, Ha WS, Park ST. Clinical Characteristics and Prognosis of Multifocal Papillary Thyroid Carcinoma. J Korean Surg Soc 2010; 79: 442-446.
- Ricci JA, Alfonso AE. Multifocal micropapillary thyroid cancer: a new indication for total thyroidectomy? Am Surg 2012; 78: 1211-1214.
- Machens A, Hauptmann S, Dralle H. Increased risk of lymph node metastasis in multifocal hereditary and sporadic medullary thyroid cancer. World J Surg 2007; 31: 1960-1965.
- Saiz AD, Olvera M, Rezk S, Florentine BA, McCourty A, Brynes RK. Immunohistochemical expression of cyclin D1, E2F-1, and Ki-67 in benign and malignant thyroid lesions. J Pathol 2002; 198: 157-162.
- Timler D, Tazbir J, Matejkowska M, Gosek A, Czyz W. Expression of proteins: D1 cyclin and Ki-67 in papillary thyroid carcinomas. Folia Histochem Cytobiol 2001; 39 Suppl 2: 201-202.
- Wang S, Lloyd RV, Hutzler MJ, Safran MS, Patwardhan NA, Khan A. The role of cell cycle regulatory protein, cyclin D1, in the progression of thyroid cancer. Mod Pathol 2000; 13: 882-887.
- Ranjbari N, Rahim F. The Ki-67/MIB-1 index level and recurrence of papillary thyroid carcinoma. Med Hypotheses 2013; 80: 311-314.
- Džodic RR, Markovic IZ, Momcilo I, Milovanovic Z, Jovanovic N. Principles of surgery for thyroid carcinoma. Arch Oncol 2003; 11: 175-177.
- Cavalheiro BG, Junqueira CR, Brandão LG. Expression of matrix metalloproteinase 2 (MMP-2) and tissue inhibitor of metalloproteinase 2 (TIMP-2) in medullary thyroid carcinoma: prognostic implications. Thyroid 2008; 18: 865-871.
- Vesely D, Astl J, Lastuvka P, Matucha P, Sterzl I. Serum levels of IGF-I, HGF, TGFbeta1, bFGF and VEGF in thyroid gland tumors. Physiol Res 2004; 53: 83-89.
- Maiorano E, Ciampolillo A, Gesualdo L, Ranieri E, Fanelli M, Viale G. Expression of transforming growth factor-ß1 in thyroid tumors. App Immunohistochem Mol Morphol 1999; 7: 135-141.