ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2005) Volume 16, Issue 2
Seroprevalence of Hepatitis C Virus (HCV) infection among blood donors in a South-Eastern State of Nigeria
1Department of Heamtology\Immunology, Collaeg of Health Sceinces, Ebonyi State University, P. M. B. 053 Aba-kalik, Nigeria
2Department of Medical Laboratory Sciences, Collage of Health Sciences, Ebonyi State University, P. M. B. 053 Abakaliki, Nigeria
- *Corresponding Author:
- Dr. Chukwurah E. F.
Department of Haematology/Immunology,
College of Health Sciences,
Ebonyi State University Abakaliki,
Nigeria
Email: osylver1 ( at ) yahoo.com
Accepted date: December 1 2004
Hepatitis C Virus (HCV) is now recognized as the most common viral infection causing chronic liver disease in human. So far, the chronic hepatitis C virus infection in many individuals is asymptomatic and the prevalence of the antibodies to this virus among blood donors in this part of the world is not well established. This study addressed the prevalence of the antibodies to Hepatitis C Virus (anti-HCV) in 1280 blood donors at University of Nigeria Teaching Hospital in Enugu – a southeastern state of Nigeria. The screening of the anti-HCV was by immunochromatographic method. Our results showed that 97 (7.6%) of the blood donors were positive for the anti-HCV. This shows a high prevalence of HCV infection among blood donors in this region when compared with those established for Western countries. There is need therefore for public interventions through mandatory screening of blood and blood products, destruction of disposable nee-dles, adequate sterilization of reusable materials and promotion of health education on HCV in-fection and its prevention.
Keywords
Hepatitis C Virus, Prevalence, Blood donors
Introduction
Epidemiological data indicated that the introduction of routine screening for Hepatitis B-surface antigen (HbsAg) in the serum of blood donors has reduced the frequency of post transfusion Hepatitis B infection but certain cases still abound [1,2,3]. Besides Hepatitis B, also Hepatitis non A, non B may be seen as cause of complications of blood transfusion [4,5,6,7]. Hepatitis C Virus which is a flavivirus with long incubation period of 2 to 26 weeks has been implicated as a principal agent of non A, non B hepatitis. The virus is plasma borne and has the same routes of transmission in common with Hepatitis B virus – sexual contact, exposure to contaminated blood and blood prod-ucts, or vertical transmission, i.e, from mother to her fetus/child during the perinatal period [8].
Acute infection is usually mild but as many as 80% of infected individuals can become chronically infected and risk serious long-term sequalae including cirrhosis, liver failure and hepatocellular carcinoma [9].
Current treatment for HCV infection is not highly effective and at least 90% of the patients who need treatment are unable to afford it [10]. Immunization for passive prophylaxis of the hepatitis infection is not readily available. Public health interventions therefore continue to be the only effective method of preventing HCV infection. These include screening blood and blood products before transfusion, effective use of universal precautions and contraceptive barrier methods, use of disposable sharps and promotion of health education on HCV infection and its prevention. However, any strategy to prevent HCV infection must be based on accurate data. Recently, prevalence estimates by WHO suggested that 3% of the world population (about 170 million people) are currently infected with HCV and therefore at risk of developing cirrhosis and liver cancer [11,9]. In developed countries, particularly USA and UK, there is mandatory screening tests for HbsAg and antibodies to HCV, HIV 1 and 2 and Treponema pallidum – syphilis [12,13]. Most developing countries and indeed some centres in Nigeria do not screen donors for Hepatitis C, hence there is dearth of information on the prevalence of this clinically important virus. This study therefore was undertaken to investigate the seroprevalence of HCV antibodies among blood donors in Enugu – a south-eastern state of Nigeria and to awaken interest therein. Ethical clearance was obtained from the Ethical Committee of University of Nigeria Teaching Hospital Enugu, Nigeria while additional consent was sought from the blood donors.
Materials and Methods
Source of samples
A total of 1280 subjects who were volunteer donors and whose consents were sought were recruited for the study. They included 1270 males and 10 females who came to donate blood for friends and relations. Care was taken to make sure that no donor was used more than once and those who have history of recent ill-health or who had donated within one year prior to the study were excluded. The study lasted from May 2002 to July 2003. 2.0 ml of whole blood were collected from each donor into a clean test tube and allowed to clot and retract. Serum samples were then separated and stored frozen until needed for the analysis.
Analysis
All serum samples were tested for anti-HCV using Anti-HCV One Step Immunochromatographic method as previously described [14]. The method employs a unique combination of purified recombinant antigens and polyclonal solid phase antibodies to selectively identify antibodies to Hepatitis C Virus with high degree of sensitivity. All the tests were carried out strictly according to the manufacturer’s instructions. Doubtful results were repeated and inconclusive ones excluded.
Results
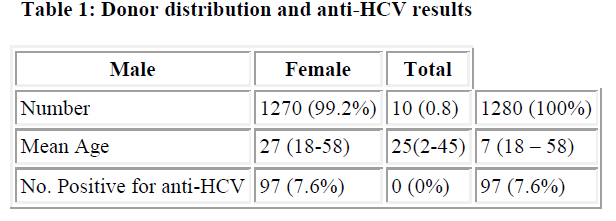
Out of the 1280 blood donors tested for anti-HCV,1270 (99.2%) were males while 10 (0.8%) were females. 97(7.6%) of the total number were positive for antibodies to HCV (Table 1). None of the female donors were positive.
Discussion
The number of infection that are potentially transmitted by blood transfusion seems daunting. Though there is dearth of information on the prevalence of this virus in Nigeria, our result of 7.6% seroprevalence is quite high. This is in variance with the figures in UK where the incidence of most of these infections in the general population is low [9,12]. In these areas, most potential donors who are at high risk of transmitting infectious agents have voluntarily stopped giving blood, and blood that is given is carefully screened so that absolute numbers of infection complications resulting from blood transfusion are minimal. Though many agents can be transmitted by transfusion including malaria parasites and other viruses, only four screening tests are currently mandatory for donors in UK. These include HbsAg for Hepatitis B Virus and antibodies to HIV 1 and 2, HCV and Tre-ponema pallidum – syphilis [12]. Presently, screening for HCV antibodies are routinely done before blood donations in all advanced countries [4,11,15]. However, in Nigeria and indeed most third world countries, only screening for HbsAg and HIV antibodies are done, where they are done at all. This definitely account for the increased risk of post-transfusion hepatitis due to non A, non B Hepatitis of which HCV is the principal agent. In most cases, greater proportion of the recipients develop chronic liver disease. Before screening for HCV antibodies was introduced in USA, about 10% of blood transfusions caused in-crease in transaminase activity in the recipients with occasional cases of symptomatic hepatitis. This figure has been drastically reduced to 0.15% [16].
To reduce the incidence of HCV-associated transfusion hepatitis in Nigeria, there is need therefore for large prospective studies on the prevalence and chronicity of non- A, non- B Hepatitis in potential blood donors within the country. This will help to institute national public health intervention programmes that will involve mandatory screening of blood and blood products before transfusion and promotion of health education on HCV infection and prevention.
Acknowledgement
We express our sincere thanks to the staff of Blood Bank section of University of Nigeria Teaching Hospital, Enugu – Nigeria for their assistance and understanding during the study.
References
- Okafor GO, Obi GO. The incidence of Hepatitis B surface antigen in Nigeria. Trans. Roy Soc Trop Med Hyg 1979; 73: 648.
- Abiodun PO, Umoike IU. HBs antigenaemia in Benin city, Nigeria. J. Pediatr. 1990; 17: 27-31.
- Schreiberer GB, Busch MP, Kleinman SH, Kerolitz JJ. The risk of transfusion transmitted viral infections. New Eng. J. Med. 1996; 316: 1685-1689.
- Iwarson S; Lindholm A, Norkrans G. Hepatitis B and non A, non B in a Swedish blood center during 10 years of HbsAg screening. Vox sang 1980; 39: 79-82.
- Richards G, Holland P, Kuramoto K, Donville D, Randell R. Prevalence of antibody to Hepatitis Virus in a blood donor population. Transfusion 1991; 31: 169-173.
- Nelson K, Ahmed F, Ness PM; Munoz A, Yawnk D, McAllister H, Stambolis V, Donaline J. Efficacy of donor screening methods on reducing the risk of transfusion transmission of HCV. Transfusion 1993; 40: 248-251.
- Tamim H; Aoun JP, Irani-Hakime N, Samaha H; Khoury S, Almawi WY. Seroprevalence of HCV infection among blood donors; a hospital-based study. Transfusion and Aspheresis Sci 2001; 24: 29-35.
- Wejstal R, Hermodsson S, Iwarson S, Wokrans G.. Mother to infant transmission of Hepatitis C virus infection. J. Med. Vi-rol. 1990; 3: 178-182.
- Touzet S, Kraemer L, Colin C, Pradet P. Epidemiology of Hepatitis C virus infection in seven European Union Countries: a critical analysis of literature. Euro J Gastroenterol Hepatol 2000; 12: 667-678.
- Brillianti S; Garson JA, Tuke PW, Ring C, Briggi M, Macici C, Miglioli M, Barbara L, Teckler RS. Effect of a-interferon therapy on Hepatitis C Viraemia in community acquired chronic non-A, non-B hepatitis. J Med Virol 1991: 136-141.
- Ouzan B, Pesle B, Baldini E, Rimbourg H; Darphin F, Brichetti A, Follana R. Epidemiological information obtained from anti-hepatitis virus screening in blood donors and candi-dates for autologous transfusion from 1992 to 1996 in the Alpes-maritime region. Gastroenterol. Clinique et Biol. 2000; 2413: 337-341.
- Garson JA, Clewly JP, Simmonds P, Zhang LQ, Mori L, Ring C, Follet EAC, Martin S. Hepatitis C Viraemia in UK blood donors. Vox sang 1992; 218-223.
- Aubuchon J. P; Birkmeyer J. D and Bush M. P. Safety of blood supply in the United States: opportunities and controversies. Ann Int Med 1997; 127: 904-909.
- Souto FJ, Riberio LC, Perazolo GF, Pforter HM, Saldanha AA. Immunoblot as a supplemental test to detect antibodies to Hepatitis C virus in donors blood. Revista-Sociedade Bras De Med Trop 2000; 35: 69-71.
- Roggendorf M; Deinhardt F; Rasshofer R; Eberle J, Hopfu Moller B; Zachoval R; Page G; Schramm W and Rommel F. Antibodies to Hepatitis C Virus. Lancet 1989; 6: 324-325.
- Barbara YAJ, Contreras M. Infection complications of blood transfusion. In: ABC of blood transfusion. B. M. J Books 1998; pg 53-64.