ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2016) Volume 27, Issue 3
Short-term observation of clinical and radiographic results of periapical microsurgery: a prospective study.
1International Clinic Center, Stomatological Hospital of Nankai University, Stomatological Hospital of Tianjin, Tianjin, 300041, PR China
2Second Department of Endodontics, Stomatological Hospital of Nankai University, Stomatological Hospital of Tianjin, Tianjin, 300041, PR China
- *Corresponding Author:
- Jing Shen
International Clinic Center
Stomatological Hospital of Nankai University
China
Accepted date: March 07, 2016
The purpose of the present study was to clinically and radiographically evaluate the periapical healing responses of patients with persistent apical periodontitis who were treated with microsurgical techniques and root-end fillings with mineral trioxide aggregate (MTA). Ninety-seven consecutive patients with 128 teeth demonstrating persistent periapical lesions were included in the study. A modern endodontic surgical protocol, which included mucoperiosteal flap elevation, an ostectomy, root-end resection, ultrasonic root-end preparation, and root-end filling with MTA, was performed. One year later, all of the patients were examined clinically and radiographically. Chi-square tests were used to analyze the results. The radiological and clinical evaluations indicated success in 57.7% of the patients, improvement in 35.1%, and failure in 7.2%. No statistically significant differences were found in the treatment results according to sex, age, or tooth type. A statistically significant relationship (P<0.05) was noted between the size and type of lesion and prognosis. The larger lesions and cysts had the worst prognoses. The use of state-of-the-art microscopes, microinstruments, and ultrasonic tips and more biologically acceptable root-end filling materials in strict microsurgical approaches produces better outcomes in patients with persistent apical periodontitis.
Keywords
Mineral trioxide aggregate, Dental operating microscope, Ultrasonics, Endodontic microsurgery, Persistent apical periodontitis.
Introduction
Apical periodontitis, which is a chronic inflammatory disorder of periapical tissues and which is caused by etiological agents of endodontic origin, can be treated with surgical and nonsurgical root canal treatments [1]. The major goals of root canal treatments are to clean and shape the root canal system and seal it in all three dimensions in order to prevent reinfection of the tooth [2]. Due to the complexity of the root canal system, inadequate aseptic control and instrumentation, poor access cavity design, debridement, leaky temporary or permanent restorations, and microorganisms in the root canals or periradicular lesions play a major role in the persistence of apical periodontitis lesions after root canal treatments [1]. Nonsurgical endodontic treatments are predictable and reliable and have high success rates that vary from 86% to 98% [3,4]. However, the success rate of retreatment cases with periapical lesions is lower. Endodontic failures can be attributed to intraor extra-radicular causes. The following six biological factors result in the persistence of asymptomatic radiolucencies after root canal treatments: persistent intraradicular infection in the complex apical root canal system, extraradicular infection, extruded root canal filling or other exogenous materials that cause a foreign body reaction, accumulation of endogenous cholesterol crystals, true cystic lesions, and healing of the scar tissue of the lesion [5].
When nonsurgical retreatments do not result in successful outcomes or are impossible due to previous prosthodontic treatments, such as crowns or posts in the root canals, periapical surgery is the treatment of choice [6]. The goal of periradicular surgery is to create optimum healing conditions through the regeneration of tissues, including the formation of a new attachment apparatus [7]. A technique that involves the use of a dental operating microscope (DOM), microinstruments, ultrasonic tips, and more biologically acceptable root-end filling materials has recently been introduced [8-10]. Schilder concluded in a recent systematic review and meta-analysis that the prognoses of patients undergoing endodontic microsurgery were significantly better than the patients who were treated with traditional root-end surgery, and endodontic surgery cured 94% of the cases of apical periodontitis [11]. Von Arx et al. reported that the probability of success for endodontic microsurgery is 1.58 times that of surgery [12].
The purpose of the present study was to clinically and radiographically evaluate the postsurgical periapical healing responses of 128 teeth in 97 patients with persistent apical periodontitis that had been previously managed by either endodontic or surgical interventions. All of the teeth were subjected to strict microsurgical procedures under a DOM, and mineral trioxide aggregate (MTA) was used as the root-end filling material.
Methods
Inclusion criteria and case selection
A total of 134 patients with periapical lesions were referred to the International Clinic Center of Stomatological Hospital of Nankai University from May 2007 to October 2010. Of these, 121 of the teeth that were observed to be poorly filled were first subjected to conventional endodontic retreatment, except for crown restorations, which are difficult to retreat. The periapical radiotransparencies of the teeth improved or disappeared in 37 cases. These cases were therefore excluded. In addition, patients with systemic diseases, especially cardiovascular disease, were excluded. The remaining 97 patients with 128 teeth were included in the study, and their sex, age, tooth type, biopsy results, and lesion size were recorded. Written informed consents were obtained preoperatively from all of the patients who agreed to participate in accordance with the Declaration of Helsinki, and exempt status was approved by the Institutional Review Board Office of Human Research Ethics at Stomatological Hospital of Nankai University.
The criteria for patient selection for endodontic surgery were stringent. The indications for periapical microsurgery were as follows [13]:
1. Periapical lesion that affected the permanent teeth and produced pain or inflammation and that had been subjected to endodontic treatment, resulting in repeated failure of the root canal treatment;
2. Periapical lesion that caused pain or swelling and that involved permanent teeth with bridge abutments that were subjected to endodontic treatment or teeth with posts that presented extraction difficulties; or
3. Symptomatic gutta-percha overfilling or foreign bodies, such as broken instruments, that were lodged in the apical third of the root canal with a concomitant infection and orthograde extraction difficulties.
The marginal bone level around the tooth in question was reduced by no more than 50% [14,15]. The periapical surgery was not performed in the acute phase of the chronic periapical abscess exacerbation or root fracture.
Criteria of healing assessment
At 3, 6, and 12 months after the microsurgery, the clinical and radiographic appearances were evaluated according to the following criteria by von Arx and Kurt [16].
1. The surgery was considered a success when bone regeneration was 90% or more and the pain and clinical ratings were 0.
2. The surgery was considered an improvement when bone regeneration was between 50% and 90% and the pain and clinical ratings were 0.
3. The surgery was considered a failure when bone regeneration was less than 50% and clinical symptoms were present.
The surgeries of the second group of patients, who had shown improvements after the surgeries, were considered successful at the one-year follow-up examination.
Surgical techniques
The microsurgeries were performed by the same endodontist. A 0.2% chlorhexidine solution was used as a rinse the night before the surgery and the morning of the surgery. Mandibular nerve block anesthesia (3-4 mL of 2% lidocaine) and local infiltration anesthesia (1.8 ml injection of 2% mepivacaine/ adrenaline) were administered for mandibular teeth. For maxillary teeth, only local infiltration anesthesia was administered (1.8 ml injection of 2% mepivacaine/adrenaline). The teeth were placed under a DOM (OPMI PROergo; Carl Zeiss Meditec, Inc., Dublin, CA, USA), and a full-thickness mucoperiosteal buccal or palatal flap was elevated with an incision of the gingival margin that was made with a microsurgical blade. A releasing vertical incision was performed to create a triangular flap in the premolar and molar regions and two incisions were made in the anterior region in order to make a rectangular flap. The periapical area was exposed by removing the covering bone with a ISO 014 round bur. The periapical area was enucleated for biopsy. The bony crypt was then examined carefully under magnification, and as much soft tissue as possible was removed so that other anatomic structures, such as the maxillary antrum and mental foramen, were not compromised. After the periodontal tissue, which was probably a granuloma, cyst, or abscess, was removed, the bone crypt was filled with 1% epinephrine pellets and dry sterile cotton pellets and left for 2 to 4 min. All of the cotton pellets, except for the first epinephrine pellets, were then removed. If bleeding continued, the procedure was repeated until hemostasis was achieved. The apical 3 mm of the root that was as perpendicular as possible to the long axis of the tooth was removed. An ultrasonic wash that was prepared after the root canal was used to remove 3 mm of the gutta-percha on all of the walls of the cavity, and a micromirror was used to ensure that the wall of the cavity was clean. All of the preparations in the bone and apicoectomies were performed under constant saline irrigation. Retrograde cavities that were 3 mm deep were prepared with a Satelec P5 ultrasonic unit (Acteon Group, Mérignac, France). A complete isthmus was prepared with appropriate ultrasonic instruments. An incomplete isthmus required a careful approach with thin ultrasonic tips that were used to create a trough along the incomplete isthmus. The MTA (white ProRoot MTA, DENTSPLY, York, PA, USA) was mixed according to the manufacturer’s instructions, spread with a microplugger, and condensed into the prepared canal. The pellet and remaining MTA were removed before the final irrigation with 0.9% sterile saline and closure of the surgical site. The resection surface and bony crypt were inspected again under the DOM, and the flaps were repositioned and sutured with interrupted 5-0 sutures. After the surgery, a periapical radiograph was immediately taken with the standardized paralleling technique.
Amoxicillin (1.5 g/day) or erythromycin (2 g/day) antibiotics were prescribed for the first postoperative week. A 0.2% chlorhexidine mouthwash was used 5–6 times a day. The sutures were usually removed 5–7 days after the surgery.
In 83 (85.6%) of the cases, a sufficient amount of tissue was obtained and submitted for histopathological evaluation. All of the enucleated biopsies were immediately fixed in 4% buffered formalin solution. The samples were embedded in paraffin, sliced into 5 μm thick sections, and stained with hematoxylin and eosin. The results of the routine histopathological evaluations were confirmed by two experienced pathologists. The specimens were classified as granulomas, scar tissues, or radicular cysts.
The patients were postoperatively reviewed at 3, 6, or 12 months. The clinical and radiographic parameters were evaluated separately by two authors according to the evaluation criteria of von Arx and Kurt [16]. The two observers calibrated their criteria before the assessments.
Statistical analysis
Ninety-seven patients (128 teeth) were clinically and radiographically followed for one year. Chi-square tests were performed on the sex, age, tooth type, biopsy results, and lesion size data. P values less than 0.05 in the two-tail test were considered significant.
Results
The age of the patients (51 men, 46 women) ranged from 12 to 66 years, with a mean of 37.
The teeth consisted of anteriors, premolars, and molars in the mandible and maxilla.
The results according to sex, age, tooth type, biopsy result, and lesion size are presented in Tables 1-5, respectively. The Chisquare tests revealed that the treatment results did not differ according to sex, age, or tooth type (P>0.05). The size and type of lesion differed significantly according to prognosis (P>0.05 for both), and the patients with the larger lesions (≥ 10 mm) and cysts were those with the worst prognoses.
| gender | Cases (%) | Success (%) | Failure (%) |
| male | 51(52.6) | 48(94.1) | 3(5.9) |
| female | 46(47.4) | 42(91.3) | 4(8.7) |
| total | 97(100) | 90(92.8) | 7(7.2) |
| * Chi-square test, P=0.705. | |||
Table 1: The treatment results of 97 cases with microsurgery related to gender.
| age | Cases (%) | Success (%) | Failure (%) |
| <45 | 72(74.2) | 67 (93.1) | 5 (6.9) |
| ≥45 | 25(25.8) | 23 (92.0) | 2 (8.0) |
| total | 97 | 90 | 7 |
| * Chi-square test, P=1.000 | |||
Table 2: The treatment results of 97 cases with microsurgery related to age.
| location | tooth type | Cases (%) | Success (%) | Failure (%) |
| anterior | 33 (34.0) | 32 (97.0) | 1 (3.0) | |
| maxilla | premolar | 16 (16.5) | 15 (93.8) | 1 (6.2) |
| molar | 10 (10.3) | 9 (90.0) | 1 (10.0) | |
| anterior | 16 (16.5) | 15 (93.8) | 1 (6.2) | |
| mandible | premolar | 13 (13.4) | 11 (84.6) | 2 (15.4) |
| molar | 9 (9.3) | 8 (88.89) | 1 (11.11) | |
| total | 97 | 90 | 7 | |
| * Chi-square test, P=0.427. | ||||
Table 3: The treatment results of 97 cases with microsurgery related to tooth type.
| biopsies | Cases (%) | Success (%) | Failure (%) |
| granuloma | 71 (85.5) | 68 (95.8) | 3 (4.2) |
| cyst | 12 (14.5) | 8 (66.7) | 4 (33.3) |
| total | 83 | 76 | 7 |
| * Chi-square test, P=0.007. | |||
Table 4: The treatment results of 83 cases with microsurgery related to biopsy.
| size | Cases (%) | Success (%) | Failure (%) |
| <10mm | 70 (72.2) | 68 (97.1) | 2 (2.9) |
| ≥10mm | 27 (27.8) | 22 (81.5) | 5 (18.5) |
| total | 97 | 90 | 7 |
| * Chi-square test, P=0.017. | |||
Table 5: The treatment results of 97 cases with microsurgery related to size.
Fourteen (14.4%) samples could not be analyzed histopathologically because they were destroyed by the apical surgery or were in very small pieces.
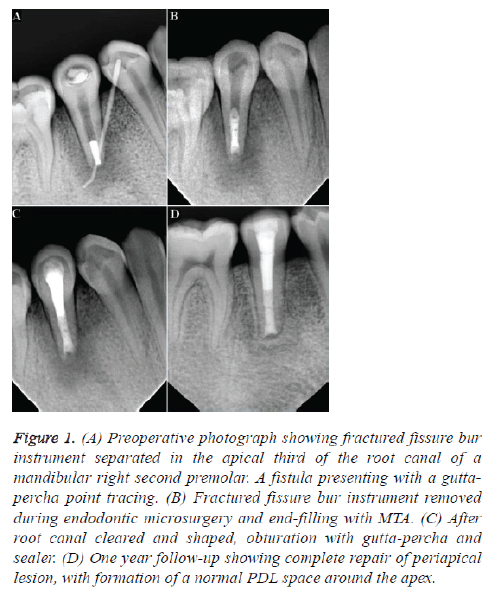
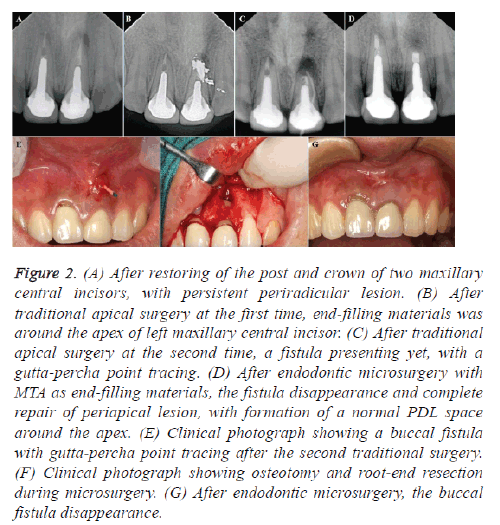
All of the 97 patients were available for the follow-up evaluations. Success was observed in 56 cases (57.7%) (Figures 1 and 2), improvement was observed in 34 cases (35.1%), and failure was observed in seven cases (7.2%). Of the seven cases with failures, two consisted of molars that were extracted due to root fracture after the procedure, and the other five cases refistulated in the anterior teeth (2 cases) and premolars (3 cases) after the microsurgery.
Figure 1: (A) Preoperative photograph showing fractured fissure bur instrument separated in the apical third of the root canal of a mandibular right second premolar. A fistula presenting with a guttapercha point tracing. (B) Fractured fissure bur instrument removed during endodontic microsurgery and end-filling with MTA. (C) After root canal cleared and shaped, obturation with gutta-percha and sealer. (D) One year follow-up showing complete repair of periapical lesion, with formation of a normal PDL space around the apex.
Figure 2: (A) After restoring of the post and crown of two maxillary central incisors, with persistent periradicular lesion. (B) After traditional apical surgery at the first time, end-filling materials was around the apex of left maxillary central incisor. (C) After traditional apical surgery at the second time, a fistula presenting yet, with a gutta-percha point tracing. (D) After endodontic microsurgery with MTA as end-filling materials, the fistula disappearance and complete repair of periapical lesion, with formation of a normal PDL space around the apex. (E) Clinical photograph showing a buccal fistula with gutta-percha point tracing after the second traditional surgery. (F) Clinical photograph showing osteotomy and root-end resection during microsurgery. (G) After endodontic microsurgery, the buccal fistula disappearance.
Discussion
Endodontic microsurgery combines the magnification and illumination of a DOM with the proper use of new microinstruments. The use of a DOM during endodontic surgery enhances the visualization of the operating field, which allows for better identification of the root apices, smaller osteotomies, shallower resection angles, better placement and use of the ultrasonic instruments, precise root filling, and better detection of the apical details, such as isthmuses, canal fins, microfractures, and the lateral canal, thus resulting in higher success rates. For cases with failed conventional endodontic treatments, nonsurgical retreatments, which provide more benefits than surgical retreatments, should be attempted first [8]. Endodontic surgery may be the only alternative to tooth extraction in cases in which the orthograde approach is not feasible due to the presence of posts or other permanent restorative materials in the coronal aspect of the root canals. One of the main objectives of endodontic surgery is sealing the root canal system against persistent or recurrent intracanal infection, thereby enabling healing by forming a barrier between the irritants within the confines of the affected root and the tissues surrounding the root.
The results showed a high incidence of periapical granulomas among the periapical lesions that were obtained during the apical surgeries, and the results supported previous reports of patients with larger lesions and cysts [13] and larger periapical lesions having worse prognoses [14-18]. Von Arx et al. reviewed the prognostic factors in apical surgeries with rootend fillings. For tooth-related factors, higher healing rates were significantly associated with the following categories: no preoperative pain or signs, root canal fillings with good densities, periapical lesions that are absent or 5 mm or less, and the use of endoscopes [19]. There were no significant healing difference in older and young patient (Table 1), and the result of our study is consistent with Tawil's research [20].
A suitable root-end filling material permits the periapical tissues to heal in an ideal manner through the regeneration of cementum, periodontal ligaments, and alveolar bone. Some of the main specifications that endodontists look for in a retrofilling material are sealing ability, handling properties, working time, radiopacity, antibacterial activity, biocompatibility, and the induction of the periodontal ligament [21]. MTA materials demonstrate acceptable biocompatible behavior and performance when they are used for root-ending fillings, perforation repairs, pulp-capping, pulpotomies, and apexification treatments. Chong et al. compared the use of intermediate restorative material (IRM) and MTA in the same technique in periapical surgery [21]. The success rate for MTA was higher (84% after 12 months, 92% after 24 months) than that of IRM (76% after 12 months, 87% after 24 months). Bernabé et al. compared a number of root end-filling materials, including MTA, IRM, zinc oxide-eugenol, and reinforced zinc oxide cement with a mixture of eugenol and ethoxy-benzoic acid (Super EBA), in dogs and found that MTA was the only material that simulated hard tissue when it was in direct contact with retrofilling material [21]. Baek et al. compared the use of super EBA, an amalgam, and MTA as root-end filling materials in dogs' teeth [22]. MTA showed the most favorable results for polymorphonuclear infiltration, bone maturation, and cementum formation.
Because the prognosis of endodontic surgery is highly dependent on good obturation and sealing of the root canal, optimal cavity preparation is an essential prerequisite for adequate root-end filling after an apicoectomy. A better centered root-end preparation lessens the risk of lateral perforation. The cleaning effects and cutting abilities of ultrasonic retrotips have been described as satisfactory [23]. In the present study of 97 treated cases, a strict microsurgical protocol using MTA as the root-end filling material was performed, and 90 cases were classified as successes and 7 cases were classified as failures. These results were consistent with those of previous reports [21,24,25].
This prospective periapical microsurgery study showed significant better clinical outcomes in patients with persistent apical periodontitis the using strict microsurgical with microinstruments, ultrasonic tips and more biologically acceptable root-end filling materials.
References
- Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J 2006; 39: 249-281.
- Tanalp J, Güngör T. Apical extrusion of debris: a literature review of an inherent occurrence during root canal treatment. Int Endod J 2014; 47: 211-221.
- de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study-Phase 4: initial treatment. J Endod 2008; 34: 258-263.
- Fernández R, Cadavid D, Zapata SM, Alvarez LG, Restrepo FA. Impact of three radiographic methods in the outcome of nonsurgical endodontic treatment: a five-year follow-up. J Endod 2013; 39: 1097-1103.
- Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod 2009; 35: 930-937.
- Abramovitz I, Better H, Shacham A, Shlomi B, Metzger Z. Case selection for apical surgery: A retrospective evaluation of associated factors and rational. J Endod 2002; 28: 527-530.
- von Arx T, Gerber C, Hardt N. Periradicular surgery of molars: a prospective clinical study with a one-year follow-up. Int Endod J 2001; 34: 520-525.
- Song M, Kim E. A prospective randomized controlled study of mineral trioxide aggregate and super ethoxy–benzoic acid as root-end filling materials in endodontic microsurgery. J Endod 2012; 38: 875-879.
- Song M, Jung IY, Lee SJ, Lee CY, Kim E. Prognostic Factors for Clinical Outcomes in Endodontic Microsurgery: A Retrospective Study. J Endod 2011; 37: 927-933.
- Song M, Chung W, Lee SJ, Kim E. Long-term Outcome of the Cases Classified as Successes Based on Short-term Follow-up in Endodontic Microsurgery. J Endod 2012; 38: 1192-1196.
- Setzer FC, Kim S. Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res 2014; 93: 19-26.
- von Arx T, Jensen SS, Hänni S, Friedman S. Five-Year longitudinal assessment of the prognosis of apical microsurgery. J Endod 2012; 38: 570-579.
- Carrillo C, Peñarrocha M, Bagán JV, Vera F. Relationship between histological diagnosis and evolution of 70 periapical lesions at 12 months, treated by periapical surgery. J Oral Maxillofac Surg 2008; 66: 1606-1609.
- Christiansen R, Kirkevang LL, Hørsted-Bindslev P, Wenzel A. Patient discomfort following periapical surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105: 245-250.
- Dietrich T, Zunker P, Dietrich D, Bernimoulin JP. Apicomarginal defects in periradicular surgery: classification and diagnostic aspects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94: 233-239.
- von Arx T, Kurt B. Root-end cavity preparation after apicoectomy using a new type of sonic and diamond surfaced retrotip: a 1-year follow-up study. J Oral MaxillofacSurg 1999; 57: 656-661.
- Molven O, Halse A, Grung B. Incomplete healing (scar tissue) after periapical surgery-radiographic findings 8 to 12 years after treatment. J Endod 1996; 22: 264-268.
- Wang Q, Cheung GS, Ng RP. Survival of surgical endodontic treatment performed in a dental teaching hospital: a cohort study. IntEndod J 2004; 37: 764-775.
- von Arx T, Penãrrocha M, Jensen S. Prognostic factors in apical surgery with root-end filling: a Meta-analysis. J Endod 2010; 36: 957-973.
- Tawil PZ, Saraiya VM, Galicia JC, Duggan DJ. Periapical microsurgery: the effect of root dentinal defects on short- and long-term outcome. J Endod 2015; 41: 22-27.
- Bernabé PF, Holland R, Morandi R, de Souza V, Nery MJ, Otoboni Filho JA, Dezan Junior E, Gomes-Filho JE. Comparative study of MTA and other materials in retrofilling of pulpless dogs’ teeth. Braz Dent J 2005; 16: 149-155.
- Baek SH, Plenk H Jr, Kim S. Periapical tissue responses and cementum regeneration with amalgam, Super EBA, and MTA as root-end filling materials. J Endod 2005; 31: 444-449.
- Stock CJ. Current status of the use of ultrasound in endodontics. Int Dental J 1991; 41: 175-182.
- Rubinstein RA, Kim S. Short-term observation of the results of endodontic surgery with the use of a surgical operation microscope and Super-EBA as root-end filling material. J Endod 1999; 25: 43-48.
- Rubinstein RA, Kim S. Long-term follow-up of cases considered healed 1 year after apical microsurgery. J Endod 2002; 28: 378-383.