ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 4
T wave peak to T wave end interval is prolonged in patients with atrioventricular nodal reentry.
Bursa Postdoctorate Training and Research Hospital, Department of Cardiology, Bursa, Turkey
- *Corresponding Author:
- Osman Can Yontar
Bursa Yüksek İhtisas Hastanesi
152 evler mah, Prof. Tezok Cad
Bursa/Turkey
Accepted June 01 2014
Atrioventricular nodal reentry tachycardia (AVNRT) is known to be associated with increased risk of susceptibility for ventricular arrhythmias and sudden death. Studies indicate that prolongation of the interval between the peak and end of the T wave (Tpeak to Tend, Tp-e) on the 12-lead ECG is a marker of ventricular arrhythmogenesis. The aim of this study was to assess ventricular repolarization in patients with AVNRT by using Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio. Patient records of Bursa Postdoctorate Training and Research Hospital were retrospectively analyzed. Electrocardiogram of 62 patients, who were diagnosed with AVNRT by electrophysiological study, were obtained and scanned. T wave peak to end interval, QT and corrected QT intervals and some other ECG intervals were measured. Electrocardiograms by age and sex were matched with 34 healthy individuals who were compared as controls. Patients with critical coronary stenosis, moderate or severe valvular disease, left and/or right heart failure, left and/or right ventricle hypertrophy, atrial fibrillation, right or left bundle block or patients who got pacemaker or ICD implanted were excluded from this study. Both groups did not differ in patient demography. Mean values for AVNRT patients and control group were: QT (362.7±43.7 vs 364.1± 34.1), QTc (417.8±43.2 vs 438.3±44.2) and Tp-e interval (83.5±16.6 vs 77.0±9.7). Tpe/ QT and Tp-e/QTc ratio were also higher in the AVNRT group. T wave peak to end interval is a measure of transmural dispersion of repolarization in the left ventricle and accepted as a surrogate for increased risk of ventricular arrhythmogenesis. Tp-e/QT and Tp-e/QTc are relatively new markers; which also indicate repolarization defects. Our results show that Tpe (p=0.018), Tp-e/QT (0.23 vs 0.21; p=0,008) and Tp-e/QTc (0.20 vs 0.17; p=0.000) were significantly higher in AVNRT group; which correspond to previous studies about strong relationship between AVNRT and ventricular arrhythmia.
Keywords
electrocardiogram (ECG), nodal reentry, tachycardia
Introduction
Atrioventricular nodal reentry tachycardia (AVNRT) is the most common form of regular supraventricular tachycardia (SVT) [1]. AVNRT is known to be associated with higher susceptibility for ventricular arrhythmias than healthy individuals [2,3]. Sudden cardiac death due to ventricular fibrillation is a rare, but serious complication of nodal reentry. Underlying mechanisms of sudden cardiac death due to these arrhythmias are unclear yet. Recent studies indicate that prolongation of the interval between the peak and end of the T wave (T peak to end, Tp-e) on the 12-lead ECG is a marker of ventricular arrhythmogenesis [4,5,6]. Prolongation of this interval represents a period of potential vulnerability to re-entrant ventricular arrhythmias. Prolonged Tp-e has been associated with increased risk of mortality in the congenital and acquired long QT syndromes [7], hypertrophic cardiomyopathy [8] and also in patients undergoing primary PCI for myocardial infarction [9]. However, there is no information available assessing the Tp-e in patients with AVNRT. The aim of this study was to assess ventricular repolarization in patients with AVNRT by using Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio.
Methods
Subjects of study
Patient records of Bursa Postdoctorate Training and Research Hospital were retrospectively analyzed. ECG of 62 patients, who were later diagnosed as AVNRT by electrophysiological study, were obtained and scanned. ECGs by age and sex were matched with 34 healthy individuals, who did not have AVNRT or any supraventricular tachycardia. They were used as controls. Patients with critical coronary stenosis, moderate or severe valvular disease, left and/or right heart failure, hypertension of any stage, left and/or right ventricle hypertrophy, atrial fibrillation, right or left bundle block or patients who got pacemaker or cardioverter/defibrillator implanted were excluded from the study.
Measurement of Tp-e, QT and QRS Intervals from the 12-Lead ECG
All ECGs were scanned. The Tp-e interval was defined as the interval from the peak of T wave to the end of T wave. Measurements of Tp-e intervals were performed from precordial leads [10]. T wave peak to end interval, QT and corrected QT intervals were measured by an engineer with a computer program involving the MATLAB (MathWorks, Natick U.S.A.) since using a ruler, vernier caliper or any other manual measuring tool to get measurements from ECG papers could be either inaccurate or slow. These codes are based on image manipulation principles.
Image manipulation method could be divided into three subdivisions: image processing, image analysis and image understanding. Image analysis is the technique that should be used to gather measurement data from ECG. Running the written code imports the image file first and then, by choice, allows the user to pick points that need to be picked to get measurements or generates a matrix that consists of a dedicated numeric value of each pixel’s color. Creating a matrix gives user the flexibility of using functions that is predefined by program. In spite of this, hand picking is easier and has a simple interface especially for beginner level users. Algorithms are developed and used to get excellent measurements in order to tolerate differences: such are tilting during scanning process, different scanning resolutions and using different ECG.
The QT interval was defined as extending from the beginning of the QRS complex to where T waves descend onto the isoelectric baseline. When a U wave interrupted the T wave before returning to baseline, the QT interval was measured to the nadir of the curve between the T and U waves. The QTc interval was calculated using the Bazett formula: QTc (miliseconds)=QT measured/√RR (seconds).
Statistical Analysis
SPSS 13.0 statistical software was utilized. Independentsamples T test and Pearson's chi-square tests were used for univariate case-control comparisons of continuous and categorical variables for all cases vs. controls, respectively.
Results
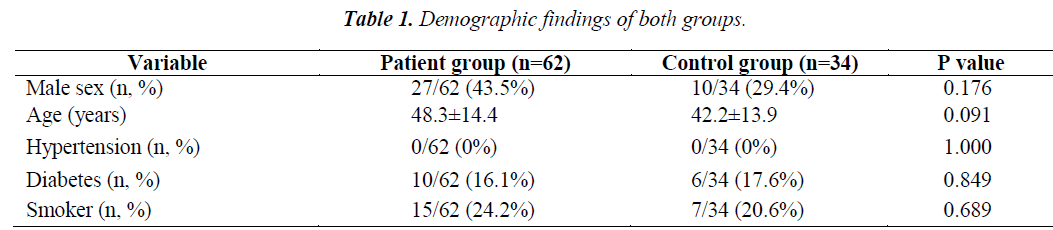
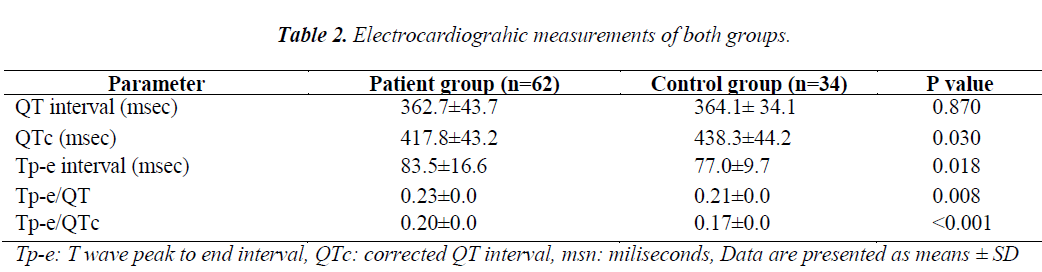
Both groups did not differ in patient demography (Table 1). Mean values for AVNRT patients and control group were: QT (362.7±43.7 vs 364.1± 34.1), QTc (417.8±43.2 vs 438.3±44.2) and Tp-e interval (83.5±16.6 vs 77.0±9.7). Tpe/ QT and Tp-e/QTc ratio were also higher in AVNRT group. All of the measurements are listed in table 2.
Discussion
The present study showed that Tp-e interval, Tp-e/QT andTp-e/QTc ratio were prolonged in patients with AVNRT. T wave peak to end interval is a measure of transmural dispersion of repolarization in the left ventricle and accepted as a surrogate for increased risk of ventricular arrhythmogenesis. Tp-e/QT and Tp-e/QTc are relatively new markers; which also indicate repolarization defects. Published studies clearly suggest the applicability of Tp-e/QT ratio as a potentially important index of arrhythmogenesis, both under the conditions of short, normal and long QT interval, as well as in congenital and acquired channelopathies. In various high-risk population, such as, patients with hypertrophic cardiomyopathy [11,12,13], post-myocardial infarction [9,11], long QT syndrome [14,15,16] inducible ventricular tachycardia [17,18,19], end-stage renal disease [20], repaired tetralogy of Fallot [21] or Brugada syndrome [10,22] Tpe interval had been found to be more prolonged than control patients.
Underlying mechanism of Tp-e prolongation in ventricular repolarization abnormality was proposed by Antzelevitch and coworkers [6]. The authors describe in their numerous articles that there are three types of identifiable cells in the ventricular myocardium. One type of these cells is the subendocardial M cell (Midmyocardial); which has larger late sodium and sodium/calcium exchange currents and a weaker slowly activating delayed rectifier current [23]. The interval of Tp-e corresponds with transmural dispersion of repolarization in the ventricular myocardium, a period during which the epicardium has repolarized and is fully excitable, but the M cells are still in the process of repolarization and vulnerable to the occurrence of early after-depolarizations [19,24,25]. In suitable conditions, a critical early after-depolarization starts a reentry circuit and maintains it long enough to evolve into polymorphic VT or VF.
As we have mentioned above, Tp-e interval and Tp-e/QT and Tp-e/QTc ratios were validated in various cardiac conditions that may lead to sudden cardiac death. Atrioventricular nodal reentry has been known for its benign course. However, some cases of sudden death are available in the literature [2,3]. In addition, idiopathic ventricular arrhythmias may coexist with AVNRT [26]. Mechanism of this susceptibility in patients with AVNRT remains unclear. Nigro et al. showed relationship between autonomic function and AVNRT [27].Thus, alterations in autonomic neural tone may be another reason for the increase of Tp-e interval and Tp-e/QT ratio in patients with AVNRT.
In our study, Tp-e; which is a surrogate for transmyocardial repolarization heterogeneity and an accepted marker for sudden death caused by ventricular arrhythmia, was found to be longer (p=0.018), in patients with AVNRT than healthy controls. What is more, results show that Tp-e/QT (0.23 vs 0.21; p=0,008) and Tp-e/QTc (0.20 vs 0.17; p=0.000) were significantly higher in AVNRT group.
Conclusion
Our findings put forward that Tp-e, Tp-e/QT and Tpe/ QTc measurements; which were obtained from surface ECG, are significantly high in patients who suffer from AVNRT rather than healthy controls. Keeping the coexistence of AVNRT and ventricular arrhythmias in mind, results raise the question whether there is myocardial repolarization heterogeneity in these patients or not. Since Tp-e prolongation is an accepted marker for sudden death caused by ventricular arrhythmia in some conditions, it is worth investigating for its utility in risk assessment for this group of patients.
Limitations
This is the first study; which aims to relate AVNRT with Tp-e measurements. However, our subject number is quite small in establishing a definite conclusion. A prospective study with long-term follow-up for ventricular arrhythmias would shed more light on this subject. Furthermore, utilization of electro-anatomic mapping systems would contribute to the evaluation of disturbances in ventricular conduction and/or electrical disarrangement. This limitation is also a result of the retrospective nature of our study.
Conflict of interest
Authors do not declare any conflict of interest.
References
- Akhtar M, Jazayeri MR, Sra J, Blanck Z, Deshpande S, Dhala A. Atrioventricular nodal reentry. Clinical, electrophysiological and therapeutic considerations. Circulation 1993; 88: 282-295.
- Wang YS, Scheinman MM, Chien WW, Cohen TJ, Lesh MD, Griffin JC. Patients with supraventricular tachycardia presenting with aborted sudden death: incidence, mechanism and long-term follow-up. J Am Coll Cardiol 1991; 181: 711-719.
- Anderson JL. Supraventricular tachyarrhythmias: not always so benign. J Am Coll Cardiol. 1991;1 81: 720-721.
- Taggart P, Sutton PM, Opthof T, Coronel R, Trimlett R, Pugsley W, Kallis P. Transmural repolarisation in the left ventricle in humans during normoxia and ischaemia. Cardiovasc Res 2001; 50: 454-462.
- Opthof T, Coronel R, Janse MJ. Is there a significant transmural gradient in repolarization time in the intact heart?: Repolarization Gradients in the Intact Heart. Circ Arrhythm Electrophysiol. 2009; 2: 89-96.
- Antzelevitch C, Sicouri S, Litovsky SH, Lukas A, Krishnan SC, Di Diego JM, Gintant GA, Liu DW. Heterogeneity within the ventricular wall. Electrophysio-logy and pharmacology of epicardial, endocardial, and M cells. Circ Res 1991; 69: 1427-1449.
- Topilski I, Rogowski O, Rosso R, Justo D, Copperman Y, Glikson M, Belhassen B, Hochenberg M, Viskin S. The morphology of the QT interval predicts torsade de pointes during acquired bradyarrhythmias. J Am Coll Cardiol 2007; 49: 320-328.
- Shimizu M, Ino H, Okeie K, Yamaguchi M, Nagata M, Hayashi K, Itoh H, Iwaki T, Oe K, Konno T, Mabuchi H. T-peak to T-end interval may be a better predictor of high- risk patients with hypertrophic cardiomyopathy associated with a cardiac troponin I mutation than QT dispersion. Clin Cardiol 2002; 25: 335-339.
- Haarmark C, Hansen PR, Vedel-Larsen E, Pedersen SH, Graff C, Andersen MP, Toft E, Wang F, Struijk JJ, Kanters JK. The prognostic value of the Tpeak-Tend interval in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. J Electrocardiol 2009; 42: 555-560.
- Castro Hevia J, Antzelevitch C, Tornés Bárzaga F, Dorantes Sánchez M, Dorticós Balea F, Zayas Molina R, Quiñones Pérez MA, Fayad Rodríguez Y. Tpeak-Tend and Tpeak-Tend dispersion as risk factors for ventricular tachycardia/ventricular fibrillation in patients with the Brugada syndrome. J Am Coll Cardiol 2006; 47(9): 1828-1834
- Savelieva I, Yap YG, Yi G, Guo X, Camm AJ, Malik M. Comparative reproducibility of QT, QT peak, and T peak– T end intervals and dispersion in normal subjects, patients with myocardial infarction, and patients with hypertrophic cardiomyopathy. Pacing Clin Electrophysiol 1998; 21:2376-2381.
- Saba MM, Arain SA, Lavie CJ, Abi-Samra FM, Ibrahim SS, Ventura HO, Milani RV. Relation between left ventricular geometry and transmural dispersion of repola- rization. Am J Cardiol 2005; 96: 952-955.
- Haarmark C, Hansen PR, Vedel-Larsen E, Pedersen SH, Graff C, Andersen MP, Toft E, Wang F, Struijk JJ, Kanters JK. The prognostic value of the Tpeak-Tend interval in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocar- dial infarction. J Electrocardiol 2009; 42: 555-560.
- Lubinski A, Lewicka-Nowak E, Kempa M, Baczynska AM, Romanowska I, Swiatecka G. New insight into repolarization abnormalities in patients with congenital long QT syndrome: the increased transmural dispersion of repolarization. Pacing Clin Electrophysiol 1998; 21: 172-175.
- Viitasalo M, Oikarinen L, Swan H, Väänänen H, Glatter K, Laitinen PJ, Kontula K, Barron HV, Toivonen L, Scheinman MM. Ambulatory electrocardiographic evide- nce of transmural dispersion of repolarization in patients with long-QT syndrome types 1 and 2. Circulation 2002;106: 2473-2478.
- Yamaguchi M, Shimizu M, Ino H, Terai H, Uchiyama K, Oe K, Mabuchi T, Konno T, Kaneda T, Mabuchi H. T wave peak-to-end interval and QT dispersion in acquired long QT syndrome: a new index for arrhythmogenicity. Clin Sci (Lond) 2003; 105: 671-676.
- Lubinski A, Kornacewicz-Jach Z, Wnuk-Wojnar AM, Adamus J, Kempa M, Królak T, Lewicka-Nowak E, Radomski M, Swiatecka G. The terminal portion of the T wave: a new electrocardiographic marker of risk of ventri- cular arrhythmias. Pacing Clin Electrophysiol 2000; 23: 1957-1959.
- Wolk R, Stec S, Kulakowski P. Extrasystolic beats affect transmural electrical dispersion during programmed electrical stimulation. Eur J Clin Invest 2001; 31: 293-301.
- Watanabe N, Kobayashi Y, Tanno K, Miyoshi F, Asano T, Kawamura M, Mikami Y, Adachi T, Ryu S, Miyata A, Katagiri T. Transmural dispersion of repolarization and ventricular tachyarrhythmias. J Electrocardiol 2004; 37:191-200.
- Tun A, Khan IA, Wattanasauwan N, Win MT, Hussain A, Hla TA, Cherukuri VL, Vasavada BC, Sacchi TJ. Increased regional and transmyocardial dispersion of ventricular repolarization in end-stage renal disease. Can J Cardiol 1999; 15: 53-56.
- Sarubbi B, Pacileo G, Ducceschi V, Russo MG, Iacono C, Pisacane C, Iacono A, Calabrò R. Arrhythmogenic substrate in young patients with repaired tetralogy of Fallot: role of an abnormal ventricular repolarization. Int J Cardiol 1999; 72: 73-82.
- Letsas KP, Weber R, Astheimer K, Kalusche D, Arentz T. Tpeak-Tend interval and Tpeak-Tend/QT ratio as markers of ventricular tachycardia inducibility in subjects with Brugada ECG phenotype. Europace 2010; 12: 271-274.
- Sicouri S, Antzelevitch C. A subpopulation of cells with unique electrophysiological properties in the deep subepicardium of the canine ventricle. The M cell. Circ Res 1991; 68: 1729-1741.
- Antzelevitch C, Shimizu W, Yan GX, Sicouri S, Weissen- burger J, Nesterenko VV, Burashnikov A, Di Diego J,Saffitz J, Thomas GP. The M cell: its contribution to the ECG and to normal and abnormal electrical function of the heart. J Cardiovasc Electrophysiol 1999; 10: 1124-1152.
- Emori T, Antzelevitch C. Cellular basis for complex T waves and arrhythmic activity following combined I(Kr) and I(Ks) block. J Cardiovasc Electrophysiol 2001; 12: 1369-1378.
- Hasdemir C, Alp A, Simsek E, Kose N, Aydin M, Payzin S. Spontaneous atrioventricular nodal reentrant tachycar- dia in patients with idiopathic ventricular arrhythmias: the incidence, clinical, and electrophysiologic characteristics. J Cardiovasc Electrophysiol 2013; 24: 1370-1374.
- Nigro G, Russo V, de Chiara A, Rago A, Cioppa ND, Chianese R, Manfredi D, Calabrò R. Autonomic nervous system modulation before the onset of sustained atrioventricular nodal reentry tachycardia. Ann Noninva- sive Electrocardiol 2010; 15: 49-55.