ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 7
The "improved bi-ring" method for the correction of mammary ptosis post augmentation mammoplasty
Ruomiao Chen, Xiuying Shan, Meishui Wang, Houbing Zheng and Biao Wang*
Department of Plastic Surgery, the First Affiliated Hospital of Fujian Medical University, Fuzhou, China
- *Corresponding Author:
- Biao Wang
Department of Plastic Surgery
The First Affiliated Hospital of Fujian Medical University, China
Accepted date: December 3, 2016
The aim of this study was to investigate the outcomes of “Improved Bi-Ring” method (IBI) of correction of post-Augmentation Mammoplasty Mastoptosis (pAMM). IBI was utilized to remove the foreign material or prosthesis after augmentation mammoplasty, thereby correcting mastoptosis. The subcutaneous tissues of the inferior pole of the breast were dissected at the 4-8 o’clock position via a bicircular incision until the submammary fold, with no wide separation in the other quadrants. The glands were incised vertically along the lower breast quadrant, the foreign material was removed, and the exterior and interior sides of the lower breast quadrant were properly folded and sutured to correct mastoptosis. In patients with intact pectoralis major, silicone prostheses were positioned behind this muscle. Between June 2008 and March 2015, IBI was performed to correct pAMM in 15 cases, including 9 cases of foreign material removal and mastoptosis correction and 6 cases of simultaneous silicone prosthesis implantation to correct mastoptosis. The follow-up lasted from 2 months to 2.5 years. The postoperative shapes of the breasts were satisfactory, and no complications occurred. IBI for correcting pAMM is a simple technique that allows concealing the scar and leads to good postoperative results.
Keywords
Augmentation mammoplasty, Mastoptosis, Bi-ring method, Complication.
Introduction
Along with their primary function of producing milk, breasts are an important symbol of female body aesthetics. In light of the rising standards of attractiveness adopted by the modern society along with an easier access to cosmetic surgery, Augmentation Mammoplasty (AM) has been widely used not only to correct physical defects but to enhance self-confidence and perceived social status [1,2]. The application of certain surgical methods, types of prostheses, and technologies may lead to the development of post-AM mastoptosis and mastatrophy in some women [3]. Mastoptosis, one of the post- AM complications, can lead to the loss of the shape and proportions of the breasts, and such complications as residue, displacement of the foreign material, and oppression, as well as capsular contracture, displacement, or even rupture of the silicone prosthesis can cause physical and psychological burden. The traditional “bi-ring” method, which was first proposed by Lexer in 1912 and improved by Benelli [4], has mainly been used, with reliable results, to correct mild to moderate mastoptosis, redundant breast deformity, and bilateral breast asymmetry.
Simple mastoptosis correction is insufficient in the treatment of post-Augmentation Mammoplasty Mastoptosis (pAMM) because two problems, prosthesis/foreign material presence and deformed breast shape, need to be addressed simultaneously and, owing to the disruption of blood supply and damage to the breast tissues during AM, removal of the prosthesis/foreign material can significantly change breast volume, leading to bilateral asymmetry [5]. The problem of simultaneous safe handling of the prosthesis/foreign material and efficient correction of mastoptosis has not been properly addressed. From June 2008 to March 2015, we employed the “Improved Bi-Ring” method (IBI) to correct 15 cases of pAMM of various types. This study retrospectively analysed these 15 cases, aiming to explore the applicability of IBI in treating pAMM.
Materials and Methods
Clinical data
All 15 women with pAMM had bilateral deformity. The mean age was 42.5 years (range: 35-50). In 7 cases, pAMM was caused by prior injection of “Orimeten”, in 6 cases by silicone prosthesis implantation, and in 2 cases by injection of artificial silicone oil. According to Regnault’s classification [6], five cases of pAMM were severe, 4 cases were moderate, and 6 cases were mild. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Fujian Medical University. Written informed consent was obtained from all participants.
Preoperative design
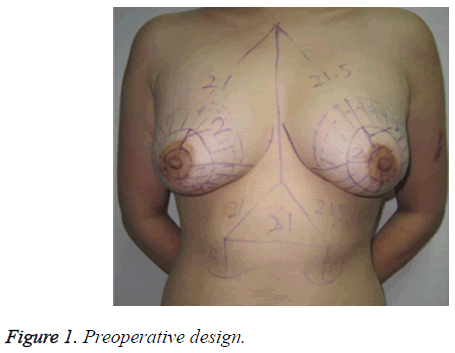
The patient was placed in a standing position with both arms hanging naturally. Both submammary folds were kept as close to the original state as possible. New positions of the nipples were chosen 18-22 cm apart from the midpoint of the sternal notch using the clavicular midline as a reference and adjusted based on the patient’s height using the following formula: height (cm) × (12-12.5%) ± 1 cm. The inner rings of the nipples were designed according to the size of the original areola and set as centers of the new areola with a diameter of 3.5-4.0 cm. The size of the outer ring mainly depended on the degree of mastoptosis and skin laxity. First, the superior pole of the outer ring, which usually forms the inner-outer ring spacing, was positioned based on the following calculation: (distance between the sternal notch midpoint and the original nipple)-(distance between the sternal notch midpoint and the new nipple). Second, the inferior pole of the outer ring was positioned to place the outer ring 5-7 cm away from the submammary fold. Next, the left and right diameters of the outer ring were selected according to the vertical diameter of the outer ring and considering the spacing between normal nipples. Finally, the dissection region was marked between the breast surface and the subcutaneous tissues, and the submammary fold was fully separated at the 4-8 o’clock region of the inferior pole of the breast, with the separation regions of the remaining quadrants kept mostly outside of the outer ring, which was equivalent to the spacing between the inner and outer rings (Figure 1).
Surgical procedures
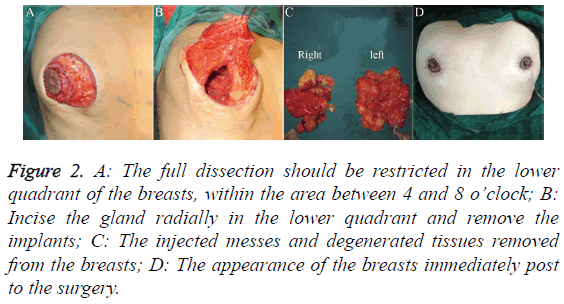
The epidermis between the inner and outer rings was removed while paying attention to preserve a complete sub-dermal vascular network. The skin flap of the mammary gland was dissected within the 4-8 o’clock regions along the exterior side of the outer ring, breast tissue surface, and subcutaneous tissues until the submammary fold, and the region was expanded as appropriate in every case. The nipple was set as the center of the lower quadrant of the breast. The gland was cut vertically and radially. The silicone implant was then examined for integrity, and the surrounding tissues were examined for damage caused by the injected prosthesis from the posterior side of the mammary gland and/or pectoralis major. The silicone implant/injected agent was removed along with surrounding degenerated tissues.
If intraoperative implantation of a silicone prosthesis was requested or the intraoperative exploration revealed no obvious damage to the pectoralis major and there was no visible foreign material within the posterior gap of the pectoralis major, the posterior gap was then bluntly and sharply separated under direct vision, with the range roughly the same as that used in AM, and a silicone prosthesis of an appropriate size was implanted.
To avoid disrupting the blood supply of the nipple-areola complex, the skin flaps in the remaining quadrants were appropriately separated, i.e. without wide separation to the edge of the breast gland, such that the dermal cap could be sutured and fixed without tension.
The interior and exterior sides of the incision edge of the lower quadrant of the breast were folded, curled, and sutured horizontally, with both glands at the incision edge curled inward to fill the posterior gland gap. Meanwhile, the mammary gland was moved up from under the fold to correct the mastoptosis. In cases with simultaneous implantation of silicone prosthesis into the posterior gap of the pectoralis major, proper folding and suturing were performed according to the extent of mastoptosis.
Drainage tubes were placed at the posterior side of the breast gland and/or pectoralis major and passed through another opening at the lateroinferior side of the breast. The dermal cap was sutured using interrupted sutures to fix the mammary gland, and the positions of both nipples were adjusted to place them at the same level and achieve bilateral symmetry. A continuous string suture with a single-strand nylon line was placed along the dermis of the outer ring to tighten the outer ring and make it approximately equal in size to the inner ring. The subcutaneous tissues and skin was sutured using interrupted suture. The surgical area was pressure dressed, and the drainage tube was connected to a high-vacuum bottle and removed 48-72 hours later. The sutures were removed after 7-9 days (Figure 2).
Figure 2: A: The full dissection should be restricted in the lower quadrant of the breasts, within the area between 4 and 8 o’clock; B: Incise the gland radially in the lower quadrant and remove the implants; C: The injected messes and degenerated tissues removed from the breasts; D: The appearance of the breasts immediately post to the surgery.
Results
No complications such as hematoma, seroma, infection, wound dehiscence, or nipple and areola necrosis occurred in our 15 patients, of which 9 underwent IBI to remove the prosthesis/injected agent and correct the mastoptosis and 6 underwent IBI to remove the prosthesis/injected agent and simultaneously implant a silicone prosthesis to correct the mastoptosis. The skin wrinkles at the outer incision edge all healed naturally within 2-3 months. The follow-up lasted between 2 months and 2.5 years. Mastoptosis improved in all the patients and a good cosmetic effect was achieved, while no significant scar hyperplasia, nipple and areola sensory dysfunction, and prosthetic capsular contracture or other adverse events occurred. None of the patients required revision surgery because of unsatisfactory breast appearance.
Representative cases
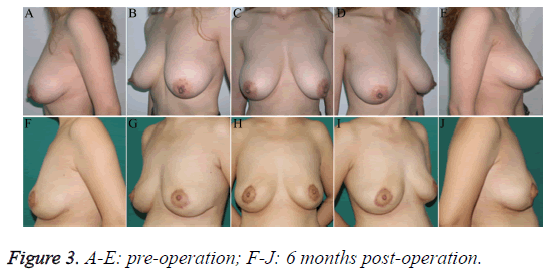
Case 1: a 50-year-old woman. This study was conducted in accordance with the declaration of Helsinki and received approval from the Ethics Committee of Fujian Medical University. Written informed consent was obtained from the participant. “Orimeten” was injected into both breasts for AM 8 years earlier. Clinical symptoms included bilateral breast asymmetry and moderate mastoptosis with palpable induration. Intraoperative exploration revealed extensive infiltration of the yellow semi-solid, water-soluble injected agent into subcutaneous tissues of both breasts, a posterior gap of the mammary gland, pectoralis major and its posterior gap, fibrosis of local tissues, and formation of foreign body granuloma. The patient underwent IBI to remove the injected material and correct the mastoptosis. Primary incision healing was achieved, with good blood supply in both nipple-areola complexes, normal sensation, and no complications such as hematoma, seroma, infection, etc. The patient was followed up for 18 months. Both breasts had a smooth appearance and were bilaterally symmetric; the sensation in the nipple-areola region was normal (Figure 3).
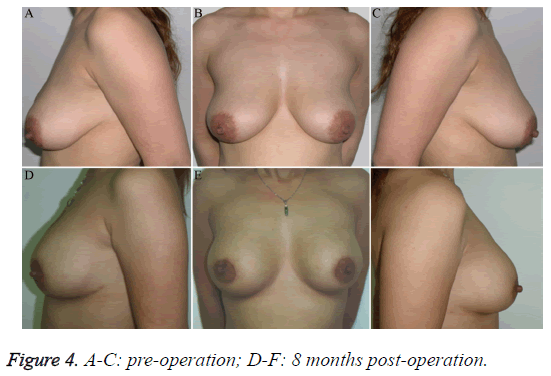
Case 2: a 35-year-old woman. This study was conducted in accordance with the declaration of Helsinki and received approval from the Ethics Committee of Fujian Medical University. Written informed consent was obtained from the participant. "Orimeten" was injected into both breasts for AM 8 years earlier. Moderate bilateral mastoptosis was present, but the breasts were soft on palpation and no induration was present in the subcutaneous tissues and glands. The patient’s request was to improve the appearance of the breasts. Accordingly, simultaneous implantation of silicon prostheses was performed after the removal of the injected agent. Intraoperative exploration revealed that the structure of the pectoralis major was still intact (with the thickness of 1.5 cm), and the elasticity was acceptable. Therefore, two 260 ml Nagor silicone prostheses were implanted during the surgery. Primary incision healing was achieved. The patient was followed up for 8 months. Both breasts appeared round and straight, with soft texture and appropriate sensation in the nipples (Figure 4).
Discussion
In recent years, AM has become one of the most common cosmetic surgical procedures. According to treatment approach, it can be divided into silicone prosthesis AM, AM by injection, autologous fat grafting AM, etc. AM may cause damage to the structures supporting the breast. Moreover, gravity and surface tension of the prosthesis after AM may inflict further damage to the surrounding tissues, causing chronic persistent injury of the structures supporting the breast [7]. This may lead to a gradual decrease in the fullness of the superior pole of the breast and opposite changes in the inferior pole [8]. Therefore, mastoptosis is one of the chronic complications after AM of various types.
According to surgical method, pAMM can be divided into following types:
Post-silicone prosthesis AM mastoptosis
Inferior gaps of the gland, pectoralis major, and biplane are currently the most widely used implantation levels, each of which has unique characteristics and limitations [9]. According to purpose of the initial AM, post-silicone prosthesis AM mastoptosis could be roughly divided into two categories. First, AM is widely applied to correct mild mastoptosis [10] if the original breast volume was large and the breasts were sagging. Clinical research revealed that breast implants are more often located in the superficial regions such as behind the mammary gland and pectoral fascia or at the inferior interface of the gland and pectoralis major [11]. The correction of the original mastoptosis is dependent more on the shrunk glands. Breast ligament reconstruction is not performed simultaneously, and pAMM emerges gradually [12]. Second, if the breasts were originally small, irrespectively of the presence of mastoptosis, breast implants can be located at any level. Given the good supporting and fixing properties of the pectoralis major, the pathogenesis of pAMM after the implantation of prosthesis into the posterior gap of the pectoralis major is considered to be the same as that of primary mastoptosis. pAMM is rare in cases with breast implants located at the posterior region of the breast glands and pectoral fascia.
Post-injection AMM
Because injection AM is carried out without direct vision while the injection volume is normally large and the injected agent is hydrophilic, this agent can easily spread and redistribute as a result of massage, squeezing, other activities, postural changes, gravity, etc. This may affect the pectoralis major, inferior gap of the glands, and even multiple levels of the mammary gland. The injected agent can be ultimately redistributed by diffusion or as a whole and induce foreign body reaction pathologically manifested with tissue infiltration, hyalinization, chronic persistent pain, swelling, bruising, etc. [13]. Refractory infections can occur in some clinical cases [14], resulting in serious damage to the supportive structures of the breast and exacerbating mastoptosis. Another notable feature of this type of AM is the infiltration of foreign material. On the one hand, this infiltration primarily damages the breast pedicle via the above mechanism. On the other hand, cavities with various sizes may form behind the mammary gland during the removal of the foreign material, leading to secondary injuries of the breast pedicle [5].
Because of the impacts of residue, displacement of the foreign material, and oppression, as well as capsular contracture, displacement and even rupture of the silicone prosthesis, and physical and psychological burdens, it may sometimes be necessary to remove the prosthesis/foreign material. As a result, the affected breast might appear imbalanced in terms of superficial tissues and volume, and more serious consequences such as mastoptosis or cosmetic problems might occur. A wide surgical field is required to accurately assess the condition of the tissues surrounding the inferior gap of the gland when removing the prosthesis or foreign material. At the same time, although the degree of secondary injury to the breast central glandular pedicle may vary, adequate blood supply to the nipple-areola complex from the surrounding glandular pedicle is necessary. In summary, irrespectively of the type of pAMM correction, foreign material should be handled properly and the blood supply of the nipple-areola complex should be maintained, making a simple mastoptosis correction unsuitable. Currently, there is no standard treatment that would include deformity correction after breast implant removal, and relevant reports are rare.
The wide surgical field employed in the traditional bi-ring method inevitably affects the blood supply of the mammary gland, and gland suspension often leads to postoperative chest pain. Therefore, we introduced a number of modifications in the traditional bi-ring method. First, we narrowed the intraoperative separation range. The nipple and areola are mostly innervated by the lateral cutaneous branch of the 4th intercostal nerve, with some participation of the 3rd and 5th intercostal nerves. The 4th intercostal nerve penetrates the chest from the axillary midline, crosses the outer edge of the pectoralis major, enters the breast gland from the inferior gap of the gland approximately 1.5-2.0 cm from the gland edge, and finally penetrates the bottom of the breast gland to control the nipple and areola [15,16]. In our method, only sufficient separation of the mammary gland at the 4-8 o’clock region of the breast inferior pole is needed. Thus, excessive separation in the breast lateroinferior quadrants, namely, the outer edge of the right beast at the 8 o’clock and the left breast at the 4 o’clock directions, is avoided, which could protect the 4th intercostal nerve. The separation towards this region of the breast gland allows satisfactory breast retraction and shaping. Second, the breast pedicle was protected: the blood supply to the regions above the nipple and areola was from the internal thoracic artery, while that to the regions beneath the lateral side was from the lateral thoracic artery and lateral perforating branches of the intercostal artery [17]. If blood vessels surrounding the nipple and areola are cut during the surgery, the nipple and areola depend on the blood supply from the deep region of the gland only. Two or three layers of angioarchitecture present in the breast [18] are connected via vertical perforating branches, and a dense network of blood vessels is present on the surface of the pectoral fascia. Therefore, excessive resection or separation of the gland or tissues may increase the risk of postoperative tissue necrosis. In our approach, only the dissection of the inferior quadrant of the breast until the inferior pole is performed, with the rest of the quadrants remaining relatively intact and the skin glandular pedicle kept as wide as possible to ensure adequate blood supply of the nipple-areola complex. Third, breast shaping is simple: glandular folding, curling, and suturing are only performed at both sides of the longitudinal incision of the breast inferior pole, which allows prevention of local pain caused by suspension and fixation of the glands in the traditional method.
IBI is a simple procedure for correcting various types of pAMM. Not only it retains the advantages of the traditional method, such as the small and hidden incision and easy acceptance by patients [4], but also avoids the occurrence of local postoperative chest pain caused by the suspension of the breast gland in the traditional method. Furthermore, the range of intraoperative peeling is narrower, which protects breast blood vessels and nerves and significantly reduces the occurrence of postoperative complications. The main disadvantage of this method is the short-term formation of folds around the surgical incision, accompanied with an uneven appearance. However, the follow-up showed that the local folds fully disappeared within 2-3 months after the surgery.
In recent years, foreign scholars have used single-pedicle dermal breast flap from the inferior pole [19], double-pedicle tissue flap [20], and traditional autologous tissue breast reconstruction surgeries, such as transverse rectus abdominis muscle flap (TRAM flap) and inferior epigastric arterial perforating flap (DIEP flap) [21], to perform autologous tissue AM, remove the prosthesis, repair breast deformity, restore breast volume, and correct mastoptosis. Autologous tissue of sufficient volume effectively filled the emptiness behind the mammary gland or pectoralis major after the prosthesis was removed and made the reformed breasts look full and naturally descending. From the point of view of long-term effects, autologous tissue is much more stable than breast implants, with the impacts of weight fluctuation, gravity, and skin sagging on its appearance much more coordinated with the contralateral breast. Although the postoperative results are nearly ideal [22], the application of an autologous tissue flap for repairing breast deformity after implant removal might cause additional trauma in the donor region, thus affecting the appearance. Furthermore, the breast blood supply may be unstable after the removal of the foreign material, significantly limiting the clinical application of autologous tissues in repairing post-AM breast deformity.
Breast suspension combined with silicone prosthesis implantation has received criticism from foreign scientists in recent years. Studies have found that implantation of a silicone prosthesis performed simultaneously with breast shaping may help to elevate the nipples, correct mastoptosis, erect the breasts, and improve bilateral breast symmetry [23], thereby restoring physical and mental health and avoiding the economical and psychological burdens associated with a second surgery [24]. However, the opinion of each individual patient regarding whether intraoperative silicone prosthesis reimplantation should be performed needs to be taken into account, and preoperative Magnetic Resonance Imaging (MRI) and intraoperative exploration of damaged tissues should be conducted. In cases with structural disorder of the breast and local tissues and significant damage to the pectoralis major caused by foreign material infiltration at multiple levels, complete removal of the foreign material might exacerbate the damage, precluding implantation of new silicone prosthesis. Such patients should be kept fully informed by orthopaedic surgeons, and postoperative psychological counselling should be provided.
Although it is widely recognized that Allosome Decellularized Dermis (ADM) can provide good coverage and support for the prosthesis and reduce prosthesis-related complications [25-27], thereby providing possibilities for implanting the prosthesis at a shallow level and achieving natural, upright breast shape, the complexity of the patient’s condition after AM should be considered. On the one hand, the depth of the location of the pectoralis major and its thickness could provide more stable support and allow encapsulation of the prosthesis. On the other hand, the surgical approach should avoid damaging the connections between the chest wall and the pectoral fascia while preserving the vascular network on the surface of the pectoral fascia to maintain the blood supply of the chest wall skin. Based on these two considerations, the inferior gap of the pectoralis major is the most appropriate level for silicone prosthesis reimplantation.
Routine preoperative breast MRI is necessary to assess the extent of damage to the breast central stem and surrounding tissues in the glandular inferior gap caused by foreign material, which is important for intraoperative judgment. In addition, it can exclude breast cancer, AM-merge local infections, etc. [28]. It is particularly important to protect the breast tissues surrounding the pedicle during the operation by limiting the extent of full separation of mammary glands to the 4-8 o’clock region of the breast inferior quadrant until the submammary fold, retaining the position of the original submammary fold, and choosing the degree at which the breast surface dermal cap can be sutured. When the gland of the breast inferior pole is cut out vertically and radially during the surgery, the mammary gland pedicle should be protected, and the foreign material and degenerated surrounding gland tissues should be removed under direct vision. Folding, curling, and suturing of the gland should be performed at the lateral sides of the gland inferior pole along the vertical incision such that the breast inferior pole curls upwards and inwards, and the void formed after the removal of the foreign material does not need filling or special fixation.
Limitations of this Study
The extent of pAMM deformity varied because of differences in AM methods and variability in tissue damage between the subjects. The small number of cases precluded statistical analysis of outcomes of IBI in pAMM of different types. Although pAMM was successfully treated with IBI in this study, a comparison of long-term effects with those of the conventional breast suspension method was not performed. Furthermore, we did not consider the influence of age, which is an important factor causing mastoptosis. In future studies, more subjects should be recruited and grouped according to age and AM surgical procedure for more in-depth comparative analysis. Finally, long-term effects of IBI in correcting pAMM need to be carefully evaluated to assess the feasibility of its clinical application.
Acknowledgements
This study was supported by the Foundation of National key Clinical Specialty Discipline Construction Program, and scientific Research Foundation of National Health and Family Planning Commission-Joint Research Projects of Fujian Provincial Health and Education (WKJ-FJ-03).
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Penaud A, De Mortillet S. Evaluation of the psychological benefits of breast augmentation for aesthetic purposes. Results of a multicenter prospective study of a series of 181 patients. Ann Chir Plast Esthet 2013; 58: 10-17.
- Kalaaji A, Bjertness CB, Nordahl C, Olafsen K. Survey of breast implant patients: characteristics, depression rate, and quality of life. Aesthet Surg J 2013; 33: 252-257.
- Somogyi RB, Brown MH. Outcomes in primary breast augmentation: a single surgeons review of 1539 consecutive cases. Plast Reconstr Surg 2015; 135: 87-97.
- Benelli L. A new periareolar mammaplasty: the round block technique. Aesthetic Plast Surg 1990; 14: 93-100.
- Wang Z, Li S, Wang L, Zhang S, Jiang Y, Chen J, Luo D. Polyacrylamide hydrogel injection for breast augmentation: another injectable failure. Med Sci Monit 2012; 18: 399-408.
- Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg 1976; 3: 193-203.
- Nicolle FV. Capsular contracture and ripple deformity of breast implants. Aesthetic Plast Surg 1996; 20: 311-314.
- Ji K, Luan J, Liu C, Mu D, Mu L, Xin M, Sun J, Yin S, Chen L. A prospective study of breast dynamic morphological changes after dual-plane augmentation mammaplasty with 3D scanning technique. PLoS One 2014; 9: e93010.
- Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg 2006; 118: 81-98; 9-102.
- Lindsey JT. Importance of the periareolar approach in the augmentation of the ptotic breast. Ann Plast Surg 2002; 48: 460-462.
- Gryskiewicz J. Dual-plane breast augmentation for minimal ptosis pseudoptosis (the in-between patient). Aesthet Surg J 2013; 33: 43-65.
- Deventer PV, Graewe FR, Wuringer E. Improving the longevity and results of mastopexy and breast reduction procedures: reconstructing an internal breast support system with biocompatible mesh to replace the supporting function of the ligamentous suspension. Aesthetic Plast Surg 2012; 36: 578-579.
- Lau PP, Chan AC, Tsui MH. Diagnostic cytological features of polyacrylamide gel injection augmentation mammoplasty. Pathology 2009; 41: 443-447.
- Bree R, Middelweerd MJ, van der Waal I. Severe granulomatous inflammatory response induced by injection of polyacrylamide gel into the facial tissue. Arch Facial Plast Surg 2004; 6: 204-206.
- Sarhadi NS, Shaw Dunn J, Lee FD, Soutar DS. An anatomical study of the nerve supply of the breast, including the nipple and areola. Br J Plast Surg 1996; 49: 156-164.
- Sarhadi NS, Shaw-Dunn J, Soutar DS. Nerve supply of the breast with special reference to the nipple and areola: Sir Astley Cooper revisited. Clin Anat 1997; 10: 283-288.
- Deventer PV. The blood supply to the nipple-areola complex of the human mammary gland. Aesthetic Plast Surg 2004; 28: 393-398.
- Odey D, Prescher A, Pallua N. Vascular reliability of nipple-areola complex-bearing pedicles: an anatomical microdissection study. Plast Reconstr Surg 2007; 119: 1167-1177.
- Honig JF, Frey HP, Hasse FM, Hasselberg J. Inferior pedicle autoaugmentation mastopexy after breast implant removal. Aesthetic Plast Surg 2010; 34: 447-454.
- Gurunluoglu R, Kubek E, Arton J. Dual pedicle mastopexy technique for reorientation of volume and shape after subglandular and submuscular breast implant removal. Eplasty 2013; 13: e48.
- Rabey NG, Lie KH, Kumiponjera D, Erel E, Simcock JW, Malata CM. Salvage of failed prosthetic breast reconstructions by autologous conversion with free tissue transfers. Eplasty 2013; 13: e32.
- Mioton LM, Seth A, Gaido J, Fine NA, Kim JY. Tracking the aesthetic outcomes of prosthetic breast reconstructions that have complications. Plast Surg (Oakv) 2014; 22: 70-74.
- Persoff MM. Mastopexy with expansion-augmentation. Aesthet Surg J 2003; 23: 34-39.
- Swanson E. Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammaplasty, performed individually and in combination. Plast Reconstr Surg 2013; 132: 30-45.
- Jansen LA, Macadam SA. The use of AlloDerm in postmastectomy alloplastic breast reconstruction: part I. A systematic review. Plast Reconstr Surg 2011; 127: 2232-2244.
- Chepla KJ, Dagget JR, Soltanian HT. The partial AlloDerm sling: reducing allograft costs associated with breast reconstruction. J Plast Reconstr Aesthet Surg 2012; 65: 924-930.
- Busse B, Orbay H, Sahar DE. Sterile acellular dermal collagen as a treatment for rippling deformity of breast. Case Rep Surg 2014; 2014: 876254.
- Youk JH, Son EJ, Kim EK, Kim JA, Kim MJ. Diagnosis of breast cancer at dynamic MRI in patients with breast augmentation by paraffin or silicone injection. Clin Radiol 2009; 64: 1175-1180.