ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2013) Volume 24, Issue 3
The benefit of combining standard automated perimetry and multifocal visual evoked potential hemifield intersector analysis in suspecious glaucomatous visual field defects.
1Department of Ophthalmology, Hamad Medical Corporation, Qatar
2School of life and health sciences, Aston University, UK
3Department of Medical Statistics & Epidemiology, Hamad Medical Corporation, Dept. of Public Health, Weill Cornell Medical College, Qatar
4Department Evidence for Population Health Unit, School of Epidemiology and Health Sciences, The University of Manchester, Manchester, UK
- *Corresponding Author:
- Abdulbari Bener
Department of Medical Statistics & Epidemiology
Hamad Medical Corporation and Dept. of Public Health
Weill Cornell Medical College
PO Box 3050
Doha- State of Qatar
Accepted date: March 12 2013
Citation: Mousa MF, Cubbidge RP, Al-Mansouri F, Bener A. The benefit of combining standard automated perimetry and multifocal visual evoked potential hemifield intersector analysis in suspecious glaucomatous visual field defects. Biomedical Research 2013; 24 (3): 277-288.
Several analysis protocols have been tested to identify early visual field losses in glaucoma patients using the mfVEP technique, some were successful in detection of field defects, which were comparable to the standard SAP visual field assessment, and others were not very informative and needed more adjustment and research work. In this study we implemented a novel analysis approach and evaluated its validity and whether it could be used effectively for early detection of visual field defects in glaucoma. The purpose of this study is to examine the benefit of adding mfVEP hemifield Intersector analysis protocol to the standard HFA test when there is suspicious glaucomatous visual field loss. 3 groups were tested in this study; normal controls (38 eyes), glaucoma patients (36 eyes) and glaucoma suspect patients (38 eyes). All subjects had a two standard Humphrey visual field HFA test 24-2, optical coherence tomography of the optic nerve head, and a single mfVEP test undertaken in one session. Analysis of the mfVEP results was done using the new analysis protocol; the Hemifield Sector Analysis HSA protocol. The retinal nerve fibre (RNFL) thickness was recorded to identify subjects with suspicious RNFL loss. The hemifield Intersector analysis of mfVEP results showed that signal to noise ratio (SNR) difference between superior and inferior hemifields was statistically significant between the 3 groups (ANOVA p<0.001 with a 95% CI). The difference between superior and inferior hemispheres in all subjects were all statistically significant in the glaucoma patient group 11/11 sectors (t-test p<0.001), partially significant 5/11 in glaucoma suspect group (t-test p<0.01) and no statistical difference between most sectors in normal group (only 1/11 was significant) (t-test p<0.9). Sensitivity and specificity of the HSA protocol in detecting glaucoma was 97% and 86% respectively, while for glaucoma suspect were 89% and 79%. The use of SAP and mfVEP results in subjects with suspicious glaucomatous visual field defects, identified by low RNFL thickness, is beneficial in confirming early visual field defects. The new HSA protocol used in the mfVEP testing can be used to detect glaucomatous visual field defects in both glaucoma and glaucoma suspect patient. Using this protocol in addition to SAP analysis can provide information about focal visual field differences across the horizontal midline, and confirm suspicious field defects. Sensitivity and specificity of the mfVEP test showed very promising results and correlated with other anatomical changes in glaucoma field loss. The Intersector analysis protocol can detect early field changes not detected by standard HFA test.
Keywords
Objective perimetry, multifocal VEP, visual field testing, glaucomatous field loss, glaucoma suspect, SAP, HFA
Introduction
It has been well established that conventional visual field testing using SAP protocols are almost always influenced by intra and inter-test variability [1].. Inter and intra-test variability, reliability, reproducibility and learning effect, are major problems that constitute the final outcome of subjectivity in current visual field testing protocols. Despite its disadvantages, which could be clearly seen in the long test duration and variability, the HFA is considered the gold standard method for visual field assessment in clinical practice and glaucoma related clinical trials [2]. The Swedish Interactive Threshold Algorithm (SITA) standard offers much shorter test times, but its variability is almost similar to that of the full-threshold strategy [3]. There has been always a need for more objectivity in the methods used for visual field assessment as opposed to conventional subjective tests, which can reduce variability and improve reliability of these tests when used in monitoring and diagnosis of glaucoma [4]. mfVEP is considered an objective method of visual field assessment as it does not require any interactive response from the patient to produce a topographic assessment of the visual field. mfVEP can provide objective visual field assessment at a good level of sensitivity and specificity [3,4]. Decisions related to management are mainly depending on the good sensitivity and specificity figure of the test, and its ability to show consistent results over time. One reported problem that affects the ability of SAP tests to determine progression of glaucomatous visual field defects is that the measurements become less repeatable as the disease advances and defects increase in depth or size [3,5]. However, despite the improvements over the past two decades, the debate still presents about the reliability of SAP in general, and with the introduction of mfVEP, the question extended to include whether mfVEP as an objective test could offer more reliability figures, and thus improve the repeatability of visual field assessment. mfVEP has shown in many studies [6-9] a good level of repeatability among normal subjects, and glaucoma patients, in short and long reassessment intervals.
The use of functional visual field assessment has been the gold standard method for detection of field scotomas and defects for decades. Clinically, it would be extremely helpful to have an agreement between two functional assessment of the visual field, such as HFA or mfVEP. The combination between these tests can overcome the shortcoming of each individual test such as poor reliability or the SAP learning curve. It was reported in many studies that HFA correlates well with mfVEP test and add more information about the visual field [10]. It was found that the combined use of these two tools enhanced the ability to detect the glaucomatous visual field defects, and they suggested that it is useful to diagnose and monitor glaucoma using this combination.
Subjects and Methods
This study was conducted at the ophthalmology outpatient clinic, Hamad Medical Corporation, Doha, Qatar. Study subjects were selected from patients attending the ophthalmology outpatient clinics during the recruitment period. All study subjects were screened by a full eye examination before enrolment by a glaucoma specialist; including intraocular pressure, Gonioscopy, visual acuity using Snellen chart, slit lamb assessment of the anterior segment, and retinal examination including the optic nerve head (optic disc). Subjects were categorized into three groups; glaucoma, glaucoma suspect, and normal controls.
Selection criteria
Selection criteria for glaucoma and glaucoma suspect patients followed the guidelines of the American Academy of Ophthalmology Preferred Practice Pattern (AAO-PPP) in the precise definition of glaucoma and glaucomasuspect patients [11]. Normal subjects were recruited after excluding any existing ocular pathology. Both genders were equally invited to participate in this study. Subjects suffering from visual field losses due to any pathology other than glaucoma, significant retinal disease with or without macular involvement, established neurological deficits that affect visual cortex or visual pathways, or subjects with amblyopia were excluded from joining this study. Subjects under the age of 16 were not recruited for this study; due to the high level of variability and poor reliability exist in SAP test for patients under age of 16 [12].
THE MFVEP TEST
The Stimulus
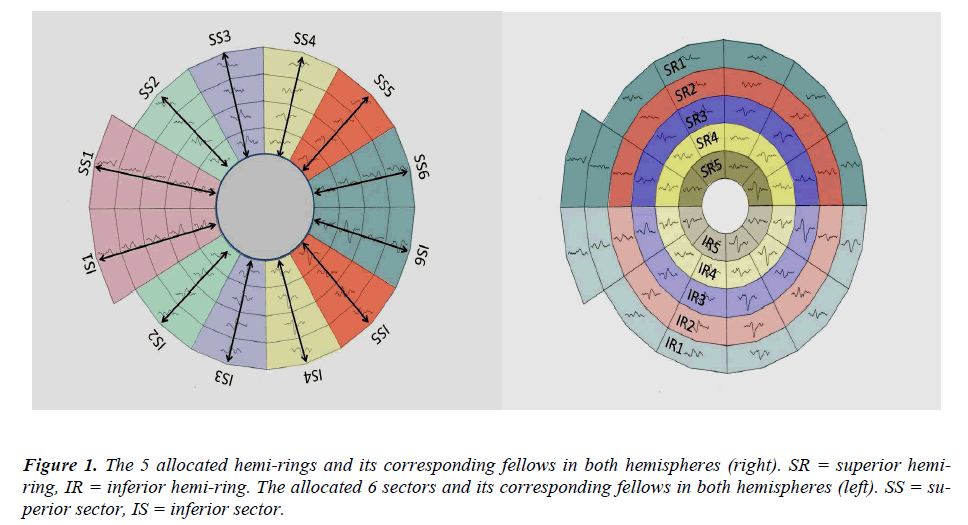
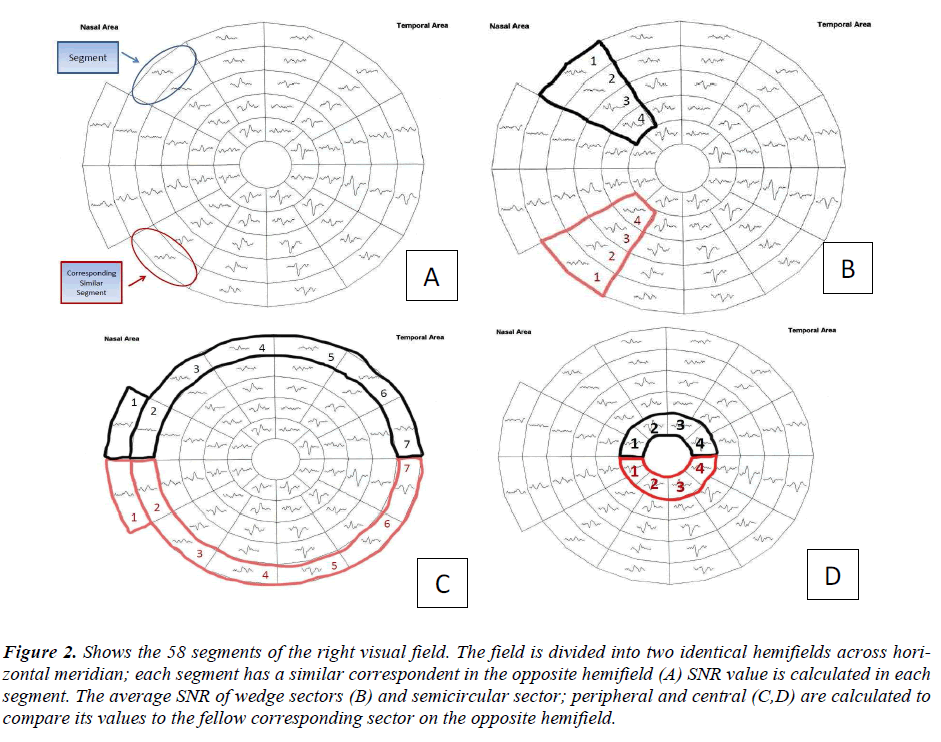
According to the guidelines of the International Society of Clinical Electrophysiology of Vision (ISCEV) (26) there is a standard requirement for the multifocal stimulus. We fulfilled the required standards; using a CRT frame frequency of 75 Hz, which has been used widely. For CRT displays, the luminance of the stimulus elements in the light state was least 100 cd/m2. The luminance of the display in the dark state was low enough to achieve a contrast (Michelson) of ≥ 90% using an m-sequence) and was used to control the temporal sequence of change between the light and dark stages of each stimulus hexagon. Recordings have been obtained with a dartboard pattern which is a standard option (Dart Board 58 with Pattern segments) of the Roland Consult GmbH software, RETIscan (Brandenburg, Germany). A modified version of this pattern has recently been introduced as part of the Hemifield Sector Analysis protocol (HSA). The modification was based upon the new idea of this research work to record the signal to noise ratio (SNR) values of each segment (figure 2-A), then calculating the average of individual sectors that contains fixed number of segments as shown in (figure 2-B). Each sector SNR value in one hemisphere is compared to its corresponding sector in the other hemisphere to calculate the difference between the two fellow sectors. Similar averaging and calculations were done in a hemi-ring group of segments arranged circumferentially around the central part as shown in (figure 2-C&D). SNR values from each two fellow hemirings are compared to see if there is any statistical difference between each couple of sectors / hemi-rings in the 3 subject groups. The dartboard pattern was presented on a monitor viewed at a distance of 30 cm; the diameter of the display subtended 44.51 cm. There are 58 sectors in this display and each sector contains 16 checks, 8 black and 8 white. The dartboard pattern covers a central 25O on each side of fixation point with nasal extension wing up to 42O. Each participant has undertaken single mfVEP test and two HFA 24-2 SITA standard tests with one hour apart during their enrolment period. The concept of the analysis protocol as described earlier is to compare and divide the mfVEP field into similar (equal) sectors and hemi-rings across the horizontal meridian, where a sector at the superior hemisphere compared to its corresponding fellow sector in the inferior hemisphere. The allocated sectors and hemi-rings, shown in (figure 1), comprise a fixed number of segments. SNR value from each segment is recorded; and an average is taken from all the segments allocated to any given sector, to give a sector average SNR value. This sector SNR value is the one compared to its corresponding sector across the horizontal meridian, and not the individual segments. Certain measurable parameters were recorded and calculated in this HSA protocol in order to compare the 3 groups. The SNR value in each sector / hemi-ring was compared to the corresponding fellow in the opposite hemisphere and the difference was calculated to check for any significant change between corresponding sectors / hemi- rings. The same SNR values and difference between sectors / hemi-rings were also compared to their similar identical ones in the 3 groups to check for any significant change between groups.
Figure 2: Shows the 58 segments of the right visual field. The field is divided into two identical hemifields across horizontal meridian; each segment has a similar correspondent in the opposite hemifield (A) SNR value is calculated in each segment. The average SNR of wedge sectors (B) and semicircular sector; peripheral and central (C,D) are calculated to compare its values to the fellow corresponding sector on the opposite hemifield.
All data obtained from the 3 study groups were analyzed using the new Hemifield Sector Analysis protocol (HSA). Paired t-test was performed to check for statistical significance for all sectors and hemi-rings. One way ANOVA test was performed to check for statistical significance between groups. Agreement between HFA and SNR was perfomed using Kappa statistics. ROC cutoff values for glaucoma and normal groups were used to perform Kappa statistical agreement tests. SNR value of 1.99 at a sensitivity level of 97% and specificity 0f 86% as detected by the ROC curve, was used as a cutoff value; where any response above this value was considered as a normal response. Kappa statistical analysis showed a good agreement between HFA and SNR.
Results
A total of 60 subjects (112 eyes) were recruited and enrolled in this study; 20 subjects (38 eyes) normal groups, 20 subjects (38 eyes) glaucoma suspects, and 20 subjects (36 eyes) glaucoma patients. All subjects had two HFA - SITA standard 24-2 visual tests and a single mfVEP test. There was no signficant age or gender distribution difference detected among the 3 study groups (P = 0.673). The mean age for all study subjects were 40.65 years.
The hemifield sector analysis
The Normal group inter-sector/hemi-ring differences between corresponding hemifields were tested for significance. Mean SNR value was 2.85 ± 0.503. 6 sectors and 5 hemi-rings on each hemifield were compared to their corresponding fellows on the opposite hemifield. There was only one pair of sectors (1/6) found signifcant, and no hemi-rings (0/5) were found to be signifcant. The glaucoma suspect group of 20 glaucoma suspect patients (38 eyes) were tested. The majority of patients (9/20) were diagnosed as glaucoma suspect based on high intraocular pressure recorded in multiple occasions, (5/20) had suspecious visual field results, (3/20) had suspicious optic disc appearance without established damage. The inter-sector/hemi-ring differences between corresponding hemifields were tested for significance. Mean SNR value was 2.27 ± 0.276. There were 4/6 sectors found to have statistically signifcant SNR difference when compared to their corresponding fellows, while 1/5 hemi-rings was statistically significant. The glaucoma group of 20 glaucoma patients (36 eyes) were tested. The majority of patients (14/20) had simple open angle glacuaoma (OAG), (3/20) had narrow angle glaucoma (NAG), and (1/20) had pseudoexfoliation glaucoma. Most of the patients (13/20) had asymmetrical glaucomatous field changes between eyes, the rest (7/20) had symmterical mild to moderate field changes. only 3/36 eyes showed advnaced glaucomatous changes with symmterical severe field loss across diline in both hemifield, all the rest (33/36) showed clear differences between the two corresponding hemifields. The inter-sector/hemi-ring differences between corresponding hemifields were tested for significance and showed that all sectors and hemi-rings were statistically signifcant when compared to its coresponding fellows in the oposite hemifield. The results show that the majority of patients had asymmetrical glaucomatous visual field defects between the two eyes. The mean SNR value for glaucoma group was 1.70 ± 0.412, which is low average response close to noisy poor signal (SNR = 1.0)
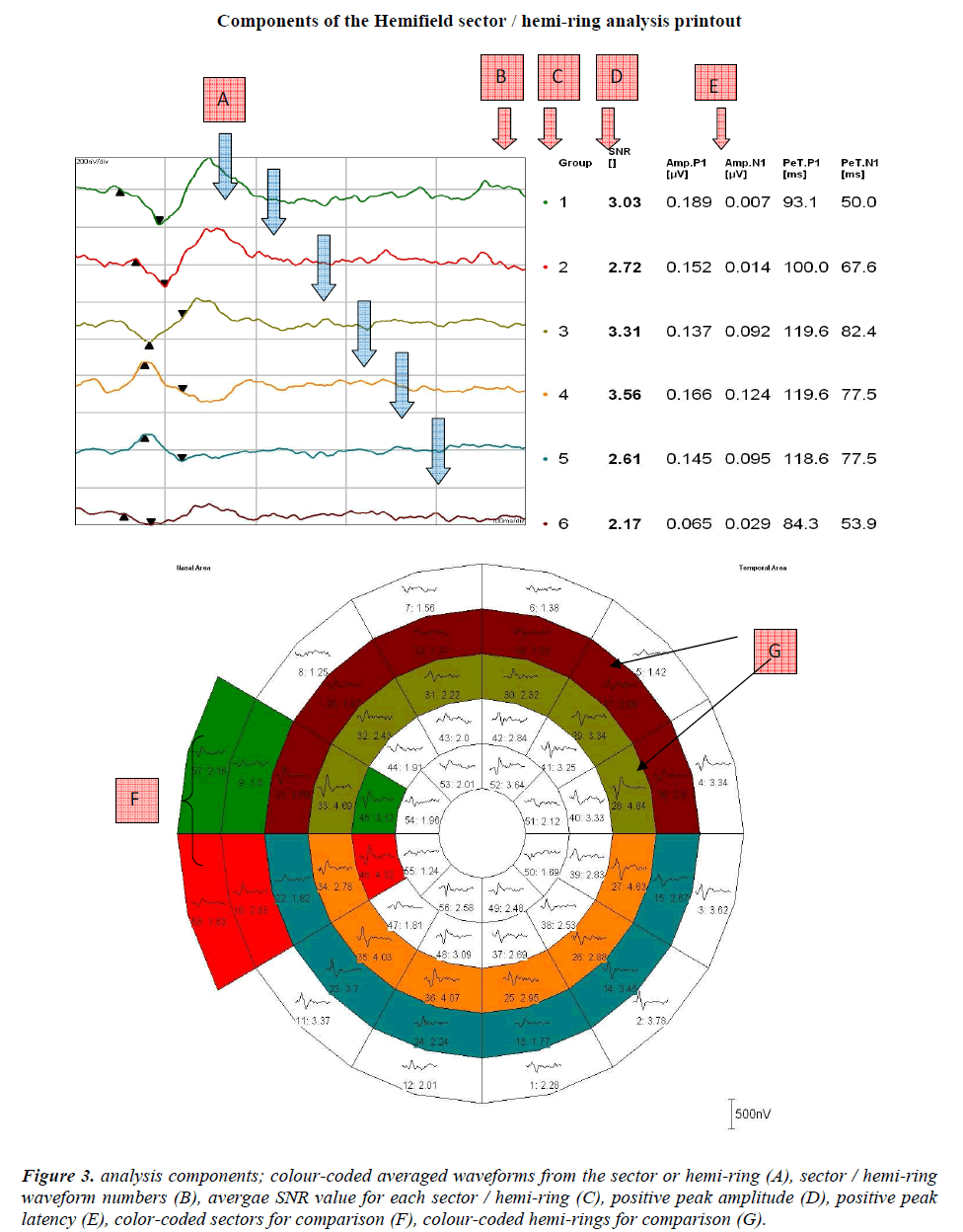
Figure 3: analysis components; colour-coded averaged waveforms from the sector or hemi-ring (A), sector / hemi-ring waveform numbers (B), avergae SNR value for each sector / hemi-ring (C), positive peak amplitude (D), positive peak latency (E), color-coded sectors for comparison (F), colour-coded hemi-rings for comparison (G).
Discussion
The sensitivity and specificity of the hemifield sector analysis protocol of mfVEP test in detecting glaucoma suspects were in this study 89% and 79% respectively. These figures are consistent with many previous study suggested a role of mfVEP objective test in the early detection of glaucoma. The majority of studies identifying the role of the mfVEP in the detection of glaucomatous visual field defects confirmed its ability to detect defects that are not detected by SAP with good sensitivity and specificity levels (76%-92%), which is a very good detection rate compared to the SAP results and its limitations in the early stages of glaucoma. The sensitivity and specificity of the hemifield sector analysis protocol in detecting glaucomatous defects were 97% and 86% respectively. These figures are supported by previous studies where the majority of studies identifying the role of mfVEP in detection of glaucomatous visual field defects confirmed its ability to detect already existent damage with high sensitivities ranging between (86%-97.5%) which is a very good detection rate when compared to SAP and its limitations in the early stages of glaucoma [13-16].
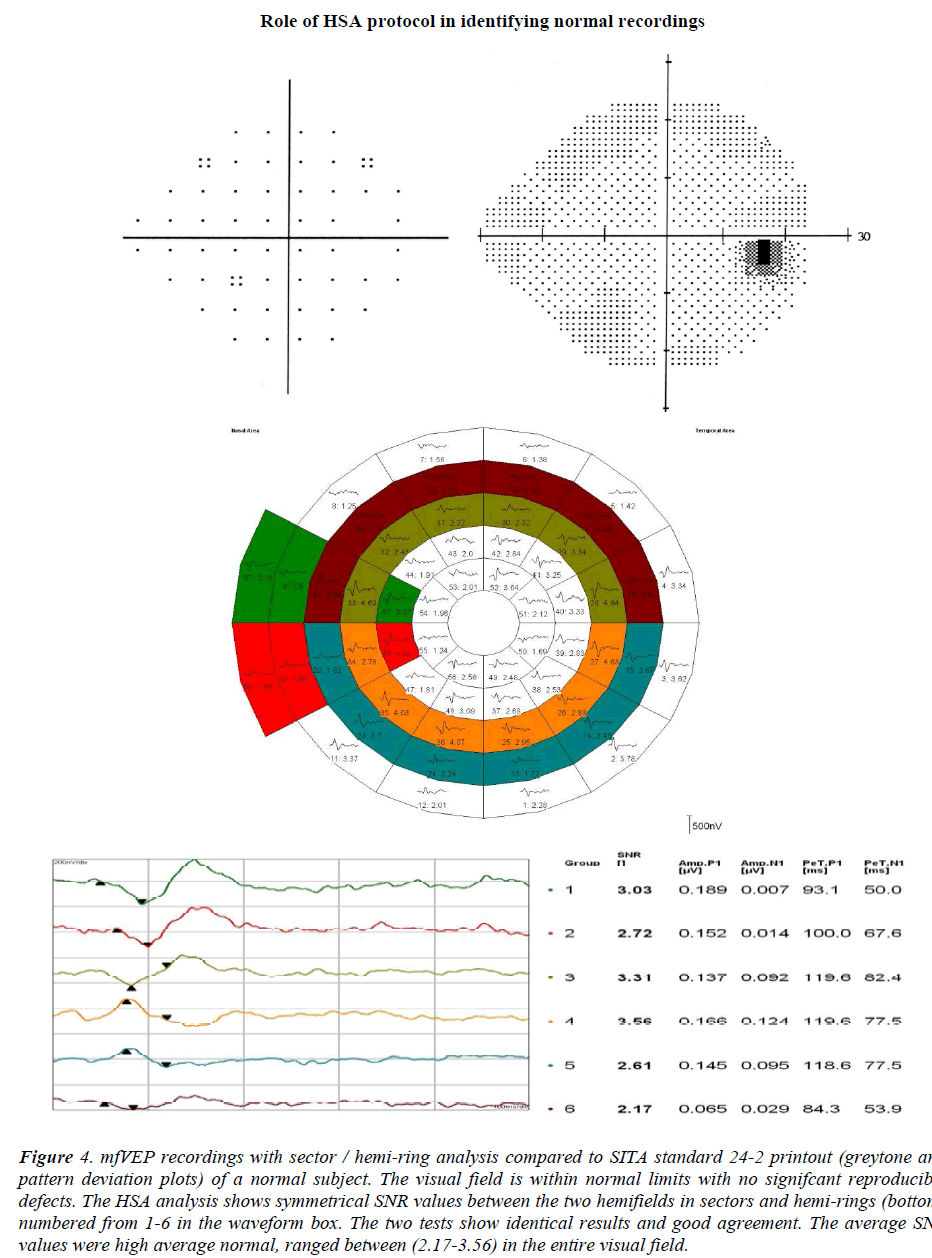
The role of mfVEP in the early detection of glaucomatous visual field defects, and in confirming an unreliable visual field test is considered the main area of recent research. Recent evidence suggests that the mfVEP can have clear role in monitoring and detecting progression of glaucoma based on good repeatability figures [15-17]. When SAP results are unreliable or inconclusive it reflects on the management plan and the follow up visits. In this study, the hemifield sector analysis protocol was able to provide interesting results in some patients with glaucoma suspect diagnosis or patients with unreliable SAP results. Figures 4 & 5 are clear examples of how this protocol was able to identify normal visual field and glaucomatous visual field accurately. All normal subjects were identified as normal visual field using the HSA protocol. Figures (6-8) show that focal depression detection in unreliable HFA test can reflect glaucomatous visual field defect. When the test is combined with mfVEP, the SNR value represents the response of each sector or hemi-ring can confirm the depression and the focal defect. Theoretically if the response in consistently low or depressed this should be a good indicator that there is a focal defect in this location. Modest visual field losses lead to very small mfVEP responses. Thus, the presence of a good SNR indicates that the visual field should be relatively good. This observation has an important clinical implication. Monocular field analysis measures focal defects precisely, the interpretation of these defects and how reliable it is could be answered by comparing the results of the two tests. The SNR of monocular responses can be used in situations where the clinician suspects that a large visual field defect is not ‘‘real’’. In their results, Hood et al [18] have shown that the presence of good SNR value almost always indicates that the visual field in this specific region is good as well. But conversely, a small mfVEP response does not necessarily mean that there will be a visual field defect or that there is a confirmed glaucomatous damage in this location, despite a large response means that the visual field sensitivity should be reasonably good, and If it is not, the SAP visual field should be questioned because a repeatable and confirmed mfVEP response is more sensitive than SAP test results. Monocular field analysis measures focal defects precisely, the interpretation of these defects and how reliable it is could be answered by comparing the results of the two tests. These measures are comparable in that it assesses the same region (the sectors of the mfVEP display versus the SAP retinal sensitivity map) of the visual field. However, the two measures do not have a comparable ratio scales; there is no direct relationship between decibels and SNR values. In addition, they do not possess the same spatial resolution. In this study the results of the two tests were evaluated indirectly by comparing the two grading systems; the HFA visual field grading system and a simple grading system which was created in this study categorizing SNR values into 5 levels, G1-G5 running between normal G1 and pure noise (SNR < 1.0). In this study kappa analysis was used for agreement between the two tests using the grading system of both tests. The agreement was 88.9% in identifying normal subjects and 77.8% in identifying glaucoma patients. These findings are in agreement with previous studies, where SAP and mfVEP results were comparable and showed similar repeatability figures [6-9,19]. The combined use of both tests; SAP and mfVEP in the category of suspicious and unreliable patients can add weight to the clinical status of the patient, especially when both agree on outcome. Figures 6-8 show examples of suspicious visual field tests that do not match with the clinical picture of the patient and still not strong enough to establish a diagnosis. The hemifield sector analysis was performed for these patients and it showed significant depression of multiple sectors corresponding with the SAP visual field test. These results when used in combination can support each other and point to a possibly true underlying glaucomatous visual field defect that need attention and modification of management plan. Clinically, it would be extremely helpful to have an agreement between a functional assessment of the visual field, such as HFA or mfVEP. The mfVEP was tested in combination with a different structural test; the optical coherence tomography measurements of the retinal nerve fibre layer thickness in a study done by Moschos et al [20], they tested two groups; normal controls and glaucoma patients who underwent the two tests. They found that the combined use of these two tools enhanced the ability to detect the glaucomatous visual field defects, and they suggested that it is useful to diagnose and monitor glaucoma using this combination. In the early stages of glaucoma, where selective types of ganglion cells are more affected and first to be lost, SAP assessment is insensitive to this selective loss since the response of other types of ganglion cells mask a defect [7]. This is probably the time when a mfVEP would be very helpful to confirm suspicious visual fields and add more credibility to the assessment of SAP. It has also been shown and proven that structural losses usually precede functional defects in glaucomatous damage (2). This means that if a structural test shows some significant losses in an unconfirmed or unreliable SAP test it is worth to take this seriously and closely monitor these patients until sufficient evidence is available. The high sensitivity of the mfVEP test can assist in these suspicious cases and alert clinicians to modify their management plan and make monitoring more often, and to add more functional and structural tests in the routine visits.
Figure 4: mfVEP recordings with sector / hemi-ring analysis compared to SITA standard 24-2 printout (greytone and pattern deviation plots) of a normal subject. The visual field is within normal limits with no signifcant reproducible defects. The HSA analysis shows symmetrical SNR values between the two hemifields in sectors and hemi-rings (bottom) numbered from 1-6 in the waveform box. The two tests show identical results and good agreement. The average SNR values were high average normal, ranged between (2.17-3.56) in the entire visual field.
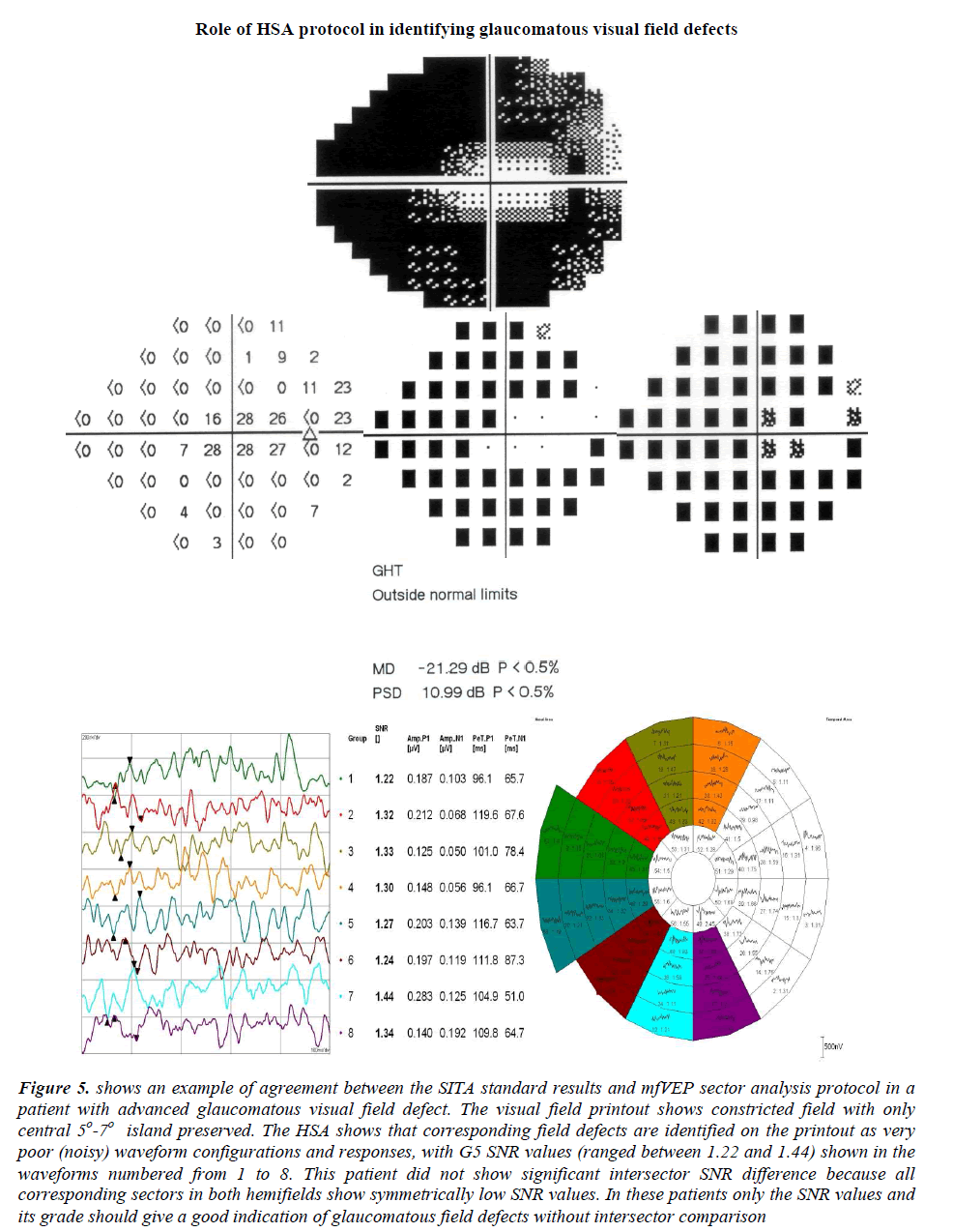
Figure 5: shows an example of agreement between the SITA standard results and mfVEP sector analysis protocol in a patient with advanced glaucomatous visual field defect. The visual field printout shows constricted field with only central 5o-7o island preserved. The HSA shows that corresponding field defects are identified on the printout as very poor (noisy) waveform configurations and responses, with G5 SNR values (ranged between 1.22 and 1.44) shown in the waveforms numbered from 1 to 8. This patient did not show significant intersector SNR difference because all corresponding sectors in both hemifields show symmetrically low SNR values. In these patients only the SNR values and its grade should give a good indication of glaucomatous field defects without intersector comparison
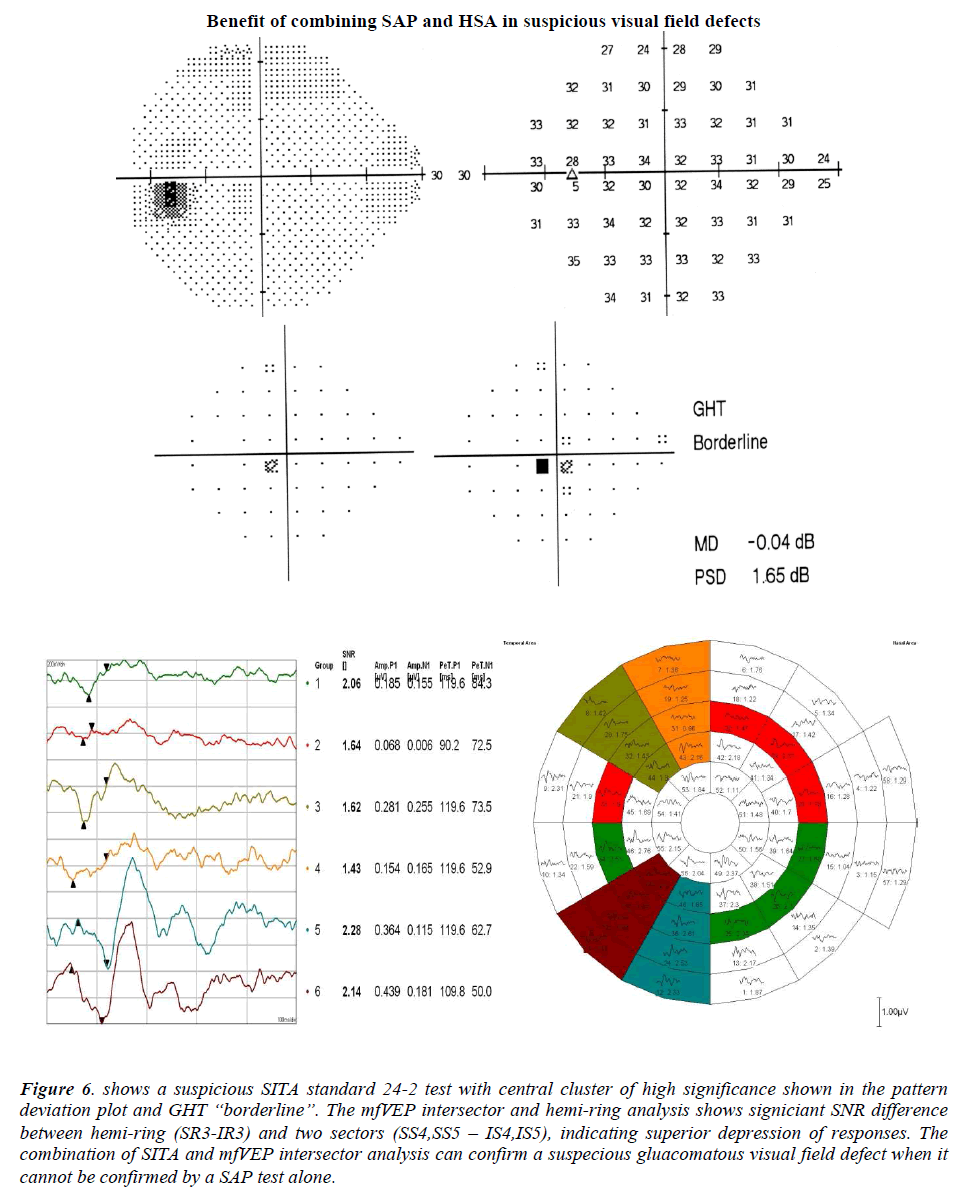
Figure 6: shows a suspicious SITA standard 24-2 test with central cluster of high significance shown in the pattern deviation plot and GHT “borderline”. The mfVEP intersector and hemi-ring analysis shows signiciant SNR difference between hemi-ring (SR3-IR3) and two sectors (SS4,SS5 – IS4,IS5), indicating superior depression of responses. The combination of SITA and mfVEP intersector analysis can confirm a suspecious gluacomatous visual field defect when it cannot be confirmed by a SAP test alone.
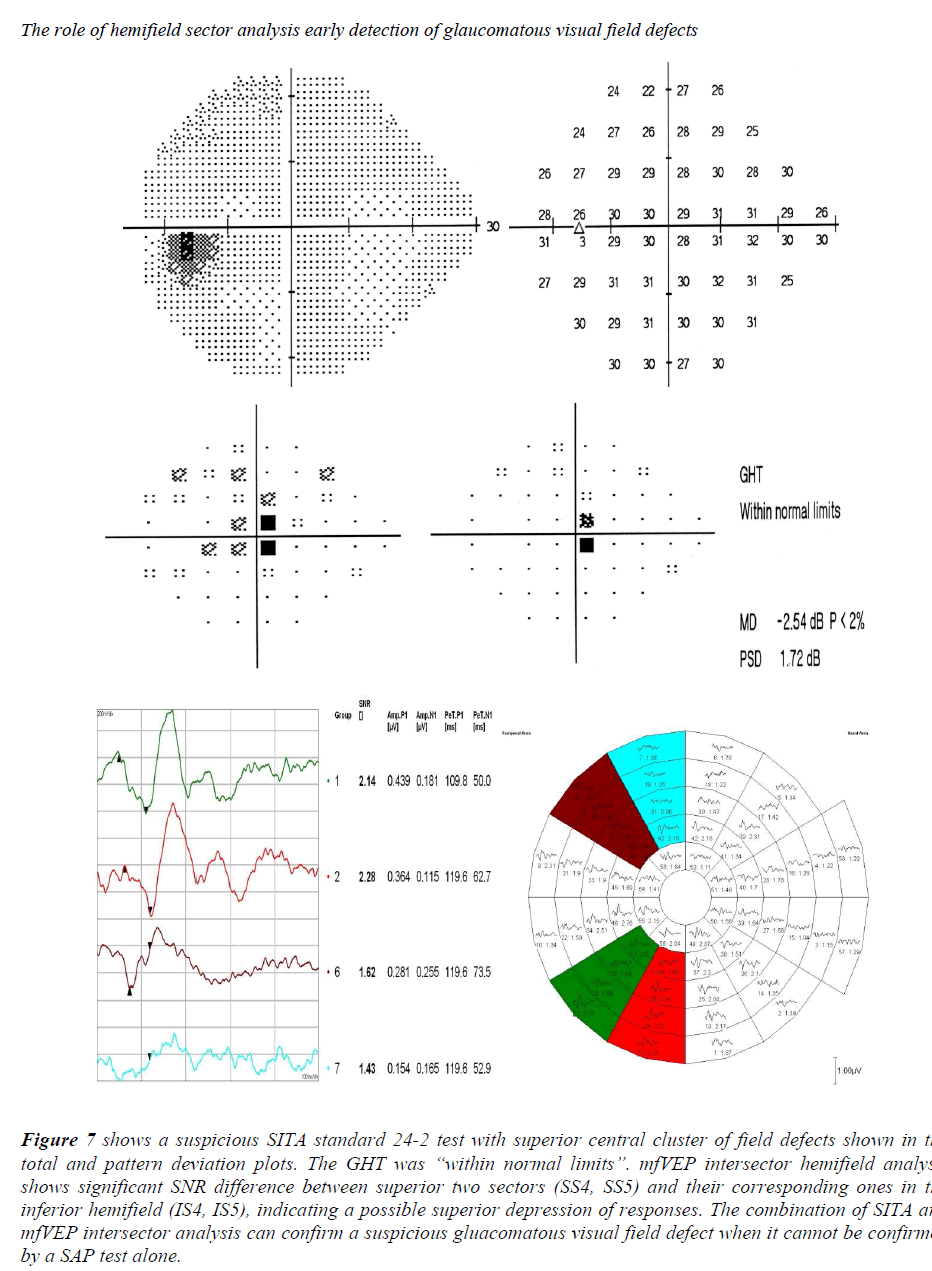
Figure 7: shows a suspicious SITA standard 24-2 test with superior central cluster of field defects shown in the total and pattern deviation plots. The GHT was “within normal limits”. mfVEP intersector hemifield analysis shows significant SNR difference between superior two sectors (SS4, SS5) and their corresponding ones in the inferior hemifield (IS4, IS5), indicating a possible superior depression of responses. The combination of SITA and mfVEP intersector analysis can confirm a suspicious gluacomatous visual field defect when it cannot be confirmed by a SAP test alone.
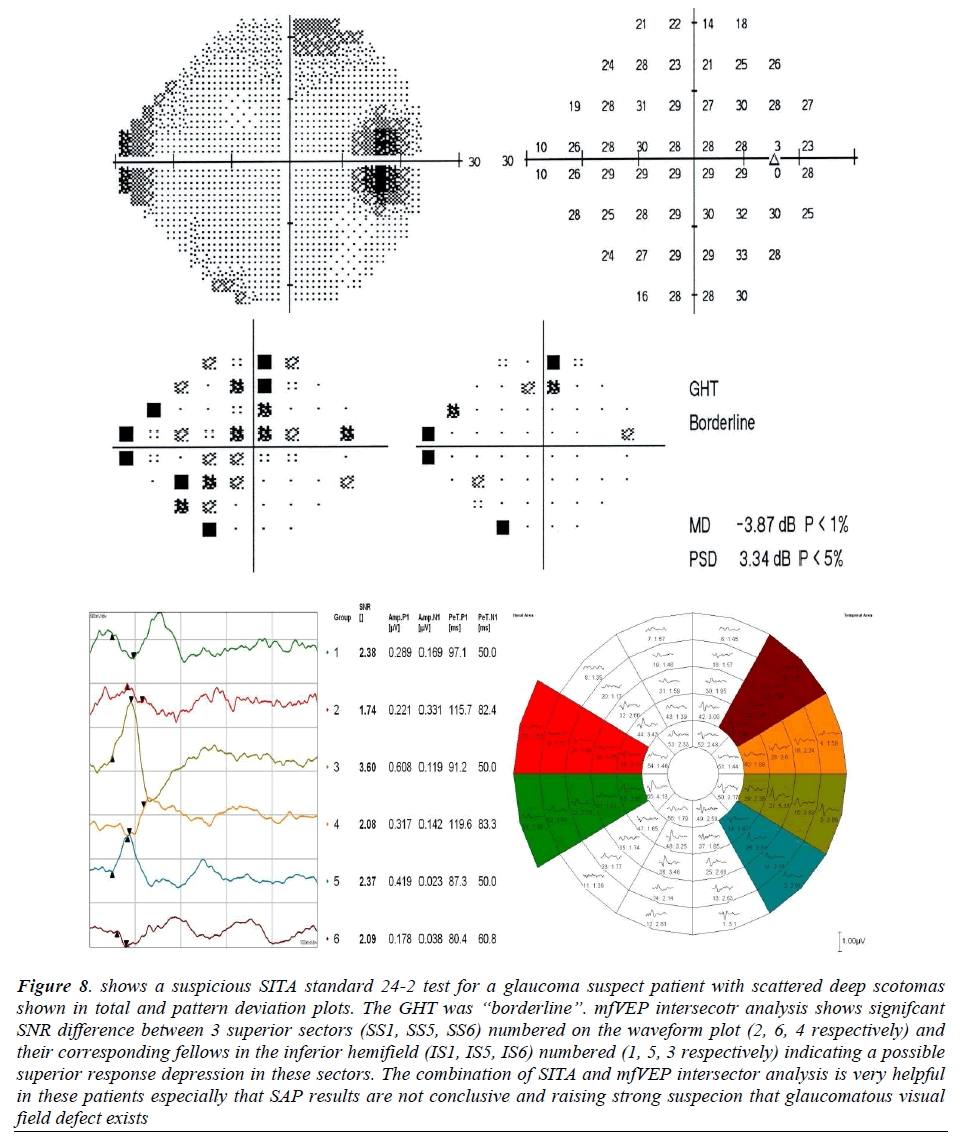
Figure 8: shows a suspicious SITA standard 24-2 test for a glaucoma suspect patient with scattered deep scotomas shown in total and pattern deviation plots. The GHT was “borderline”. mfVEP intersecotr analysis shows signifcant SNR difference between 3 superior sectors (SS1, SS5, SS6) numbered on the waveform plot (2, 6, 4 respectively) and their corresponding fellows in the inferior hemifield (IS1, IS5, IS6) numbered (1, 5, 3 respectively) indicating a possible superior response depression in these sectors. The combination of SITA and mfVEP intersector analysis is very helpful in these patients especially that SAP results are not conclusive and raising strong suspecion that glaucomatous visual field defect exists
Conclusion
The combined use of HFA and mfVEP hemifield sector analysis protocol has shown good results in confirming suspicious visual field defects. The use of both tests can add more information to the clinician, enabling a better management plan and close monitoring of suspected visual field losses. Longitudinal studies still needed to assess these patients over time to see if early prediction of visual field defects detected by the combined use of HFA and mfVEP tests was accurate or not.
Acknowledgement
We would like to thank Hamad Medical Corporation for their support and approval of this study (HMC Research Protocol # 11351 / 2012)
References
- Heijl A, Lingren A, Lindgren G. Test-retest variability in glaucomatous visual fields. Am J Ophthalmol. 1989; 108:130-135.
- Kerrigan-Baumrind LA, Quigley HA, Pearse ME, Kerrigan DF, Mitchell RS. Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci. 2000; 41: 741-748.
- Artes PH, Hutchison DM, Nicolela MT, et al. Threshold and variability properties of matrix frequencydoubling technology and standard automated perimetry in glaucoma. Invest Ophthalmol Vis Sci. 2005; 46: 2451-2457.
- Bengtsson B, Heijl A. Evaluation of a new perimetric threshold strategy, SITA, in patients with manifest and suspect glaucoma. Acta Ophthalmol Scand. 1998; 76:268-272.
- Artes PH, Iwase A, Ohno Y, Kitazawa Y, Chauhan BC.Properties of perimetric threshold estimates from full threshold, SITA standard, and SITA fast strategies. Invest Ophthalmol Vis Sci 2002; 43: 2654-2659.
- Goldberg I, Graham SL, Klistorner AI. Multifocal objective perimetry in the detection of glaucomatous field loss. Am. J. Ophthalmol. 2002; 133: 29-39.
- Klistorner AI, Graham SL, Grigg JR, Billson FA. Multifocal topographic visual evoked potential: improving objective detection of local visual field defects. Invest.Ophthal Vis Sci 1998; 39: 937-950.
- Klistorner AI, Graham SL. Objective perimetry in glaucoma. Ophthalmology 2000; 107: 2283-2299.
- Bjerre A, Grigg JR, Parry NR, et al. Test-retest variability of multifocal visual evoked potential and SITA standard perimetry in glaucoma. Invest Ophthalmol Vis Sci 2004; 45: 4035-4040.
- Graham SL, Klistorner AI, Grigg JR, Billson FA. Objective VEP perimetry in glaucoma: asymmetry analysis to identify early deficits. J Glaucoma 2000; 9: 10-19.
- American Academy of Ophthalmology Preferred Practice Pattern (AAO-PPP) Definition and Guidelines for: Primary Open-Angle Glaucoma; Primary Angle-Closure Glaucoma; Primary Open-Angle Glaucoma Suspect. AAO publications 2010.
- Bengtsson B, Olsson J, Heijl A, et al. A new generation of algorithms for computerized threshold perimetry, SITA. Acta Ophthalmol Scand 1997; 75: 368-375.
- Chen C, Hood DC, Zhang X, Emely Karam Z, Jeffrey LM, Ritch R, Thienprasiddhi P, Greenstein VC. Repeat Reliability of the Multifocal Visual Evoked Potential in Normal and Glaucomatous Eyes. Journal of Glaucoma 2003; 12: 399-408.
- Graham SL, Klistorner AI, Goldberg I. Clinical application of objective perimetry using multifocal visual evoked potentials in glaucoma practice. Arch Ophthalmol 2005; 123: 729-739.
- Hood DC, Zhang X. Multifocal ERG and VEP responses and visual fields: comparing disease-related changes. Doc Ophthal 2000; 100: 115-137.
- Thienprasiddhi P, Greenstein VC, Chen CS, et al. Multifocal visual evoked potential responses in glaucoma patients with unilateral hemifield defects. Am J Ophthalmol. 2003; 136: 34-40.
- Thienprasiddhi P, Greenstein V, Chu D, Xu L, Liebmann MJ, Ritch R, Hood DC. Detecting early functional damage in glaucoma suspect and ocular hypertensive patients with the multifocal VEP technique. J Glaucoma 2006; 15: 321-327.
- Hood DC, Greenstein VC. Multifocal VEP and ganglion cell damage: applications and limitations for the study of glaucoma. Progress in Retinal and Eye Research 2003; 22: 201-251.
- Watanabe K, Shinoda K, Kimura I, Mashima Y, Oguchi Y, Ohde H. Discordance between subjective Perimetric visual fields and objective multifocal visual evoked potential-determined visual fields in patients with hemianopsia. Am J Ophthalmol 2007; 143: 295-304.
- Moschos M, Georgopoulos G, Chatziralli I, Koutsandrea C. Multifocal VEP and OCT findings in patients with primary open angle glaucoma: A cross sectional study. BMC Ophthalmology. 2012; 12: 34-42.