ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 18
The effectiveness of computed tomography-guided lumbar epidural steroid injections for spinal pain management: A single center experience with 2-year follow-up
Ali Harman1, Enes Duman2* and Adnan Ozdemir1
1Department of Radiology, Baskent University Medical Faculty, Ankara Research Center, Ankara, Turkey
2Department of Radiology, Baskent University Medical Faculty, Konya Research Center, Konya, Turkey
- *Corresponding Author:
- Enes Duman
Department of Radiology
Baskent University Medical Faculty, Turkey
Accepted date: July 26, 2017
Purpose: To determine the therapeutic value and long-term effects of Computed Tomography (CT)- guided translaminar and transforaminal lumbar epidural steroid injections for spinal pain management.
Materials and Methods: Between December 2011 and June 2013, 428 CT-guided epidural steroid injections of the lumbar spine for 310 patients were assessed retrospectively. There were 325 Translaminar (TL) (in 225 patients) and 103 Transforaminal (TF) (in 85 patients) injections performed. The clinical effectiveness of the injection after the therapy was assessed using Visual Analog Scale (VAS). The patients were classified into three groups (A-C) after injections according to the reduction in the VAS’s.
Results: Technical success rate of 100% without any major complication related to needle placement or drug administration. There were 27 (6.3%) reported minor complications (n: 3 orthostatic hypotension (0.7%) and n: 24 transient motor weaknesses of lower extremities (5.6%). The mean visual analog scores before and after the injections were recorded as 8.9 ± 1.1 and 4.8 ± 2.5 retrospectively (p<0.001). In 23 of 310 patients epidural injections were repeated in different times during study and 73 epidural injections (n: 61 TL and n: 12 TF) were performed.
Conclusion: CT guided epidural injection in the lumbar spine is safe, repeatable and efficacious pain management technique. Both translaminar and transforaminal epidural steroid injections can provide reliable pain relief for up to average 5.5 and 5.6 months respectively.
Keywords
Spinal pain, Epidural steroid injection, Translaminar, Transforaminal
Introduction
Spinal pain may be the most common type of chronic pain suffered and has a reported lifetime prevalence of 54-80% [1]. It is estimated that 20% of the general population may suffer from chronic pain of any type at a given point in time [2]. Inter-vertebral disc herniation, spinal stenos, inter-vertebral disc degeneration without disc herniation, degenerative spondylolisthesis with stenos, and post lumbar surgery syndrome are the most common diagnoses of low back pain with or without leg symptoms [3,4]. There are no interventions which provide definite and long-term improvement in chronic low back pain, neither conservative nor surgical [5].
Epidural steroid injection is one of the most frequently performed interventional pain management procedures. Steroid injections usually with a local anesthetic can be performed by translaminar, transforaminal or caudal approaches. TL epidural steroid injections are more suitable for patients with spinal pain or stenos while TF epidural steroid injections are more suitable for isolated spinal nerve stimulation [6,7].
The most widely used methods to epidural steroid injections are fluoroscopy and CT. The needle position, anatomic structures, distribution of the contrast agent can be seen more clearly on CT than fluoroscopy. So the complication rate decreases with CT [8].
In the lumbar spine, both TL and TF epidural steroid injections usually helpful to pain relief for 6 months of pain relief, though long-term benefits are less reliable [9].
In our study we retrospectively observed the degree and duration of pain relief for CT guided TL and TF epidural steroid injections in 2 y follow up.
Methods and Results
All of the procedures in our study were made out-patiently by four experienced interventional radiologists. The patients suffering from chronic low back pain with or without leg symptoms were directed to our interventional radiology unit from orthopedics, neurosurgery and physical rehabilitation clinics. The routes and levels of the injections were determined regarding to the physical examination findings of the clinicians which were supported by imaging modalities included CT and MR prior to the procedure.
TL epidural steroid injections were performed for patients with lower back pain associated with especially spinal stenos. In the case of multilevel spinal stenos two most effected levels were targeted for injection. TF epidural steroid injections were performed for patients with isolated or multilevel spinal nerve root irritation.
The patients were questioned regarding previous steroid using not to causing iatrogenic Cushing syndrome. If patients used steroid the operation was performed two or three months later. If patients have hemorrhagic diathesis, entry point infection, or allergic disorders, the operation must be postponed.
We informed the patients about the process, results, and complications before the treatment and they signed the patient consent form. If conscious sedation was administered patient, they were monitored.
All of the injections were performed by using conventional CT (Siemens, Somatom Volume Zoom, Dec 2000, Germany) technique because we had no CT fluoroscopy. We can get short section images which were applied technician to provide access via conventional CT. While the images were achieving, only patient was in the room; so operators and technician were not exposed the radiation.
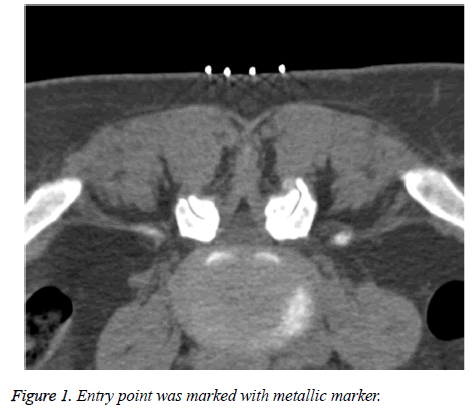
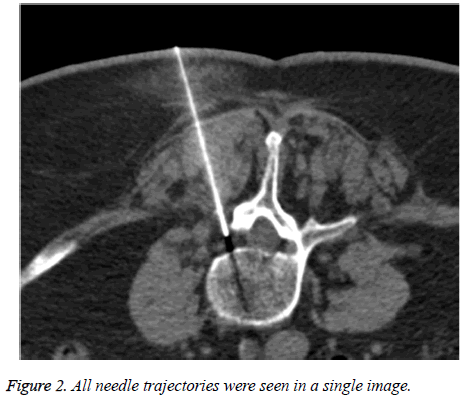
The patients were positioned prone on the CT table. A pillow under the abdomen was used in some patients to open the lumbar interspinous spaces. Then we marked the entry point with metallic marker (Figure 1). After getting a radiographic scout image, the operator delineated the necessary field of view for planning CT scan. Metalic marker was used to plan the needle trajectory. Ideally, we should see the all needle trajectory in a single image (Figure 2). Before sterile preparation of the entry site the skin was marked and metalic marker was removed. After administration of the local anesthetic agent (prilokain HCl 20 mg/ml-Citanest 2%) at the entry point, we left the local anesthesia needle in situ, because it was helpful to make the planned trajectory with images when it was a normal trajectory.
All of the injections were performed using 22 G Chiba needles to minimalize the risk of vascular injury and reduce CT artifact. The needle trajectory and tip position was viewed in the process by using recurrent conventional CT.
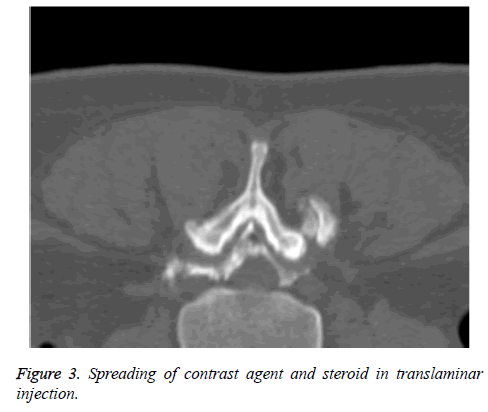
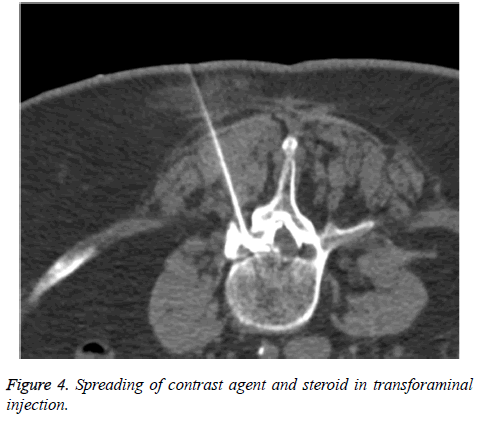
Posterior epidural space, which can be seen as a triangular shaped hypodense area in conventional CT images was targeted in TL injections. In TF injections the needle was advanced to the exiting nerve root. Patients said that they had often pain along the nerve tracing. Once the needle was positioned correctly 0.5-1 ml diluted contrast agent (Ioversol- Optiray 350) with a concentration of 20% was injected and spreading pattern of the contrast agent in epidural space was controlled with CT scans. In TF injections periradicular with or without anterior-posterior epidural spreading, in TL injections posterior epidural with or without anterior epidural-bilateral transforaminal spreading was accepted as a successfully injection (Figures 3 and 4). Consequently, a combination of 4 ml bupivakain HCl (0.5% Marcaine (5 mg/ml)) and 40 mg triamsinolon asetonid (1-2 ml Sinakort-A or Kenakort-A) was injected. In patients which were undergone two injections in the same session 40 mg triamsinolon asetonid was added to the combination. In some cases, control CT of the target area was performed to evaluate the technical results and to determine possible complications. Patients were followed-up for 1 h.
The clinical effectiveness of the injections and the pain relief time after the therapy were assessed using Visual Analog Scale (VAS). VAS is a pain scoring scale between 0 and 10 degrees. Before and after the injections VAS’s were recorded. The patients were questioned after injections about the reduction of the VAS’s. The patients were classified into three groups (A-C) after injections according to the reduction in the VAS’s. The reduction of the VAS equal or more than 50% after injection was accepted as sufficient response (group A) and less than 50% as insufficient response (group B) to the injection. If there was not any change in the VAS, it was accepted as a negative response (group C) to the therapy. In group A and B the pain relief time after the injections were determined. In 23 of 310 patients epidural injections were repeated different times and 73 injections (61 TL and 12 TF) performed. The clinical outcomes of these patients were recorded.
Between November 2011 and June 2013, a total of 310 patients (228 women and 82 men) who were performed 428 CT-guided epidural steroid injections (325 TL and 103 TF injections) of the lumbar spine were assessed retrospectively. The mean age was 65 ± 14.8 y (18-90 y).
All of 428 injections were achieved with a technical success rate of 100% without any major complication related to needle placement or drug administration. During the study time dural puncture occurred in four patients and injections were repeated in any other time. These patients were not included to the study group. There were 27 (6.3%) reported minor complications (n: 3 orthostatic hypotension (0.7%), 24 transient motor weakness of lower extremities (5.6%) in transforaminal (n: 19) and translaminar (n: 5) injections).
The injections were performed between first lumbar and first sacral vertebras in the spine. The injection numbers for different levels of the lumbar spine were 226 in L4-L5 (173 TL and 53 TF), 95 in L3-L4 (83 TL and 12 TF), 81 in L5-S1 (47 TL and 34 TF), 17 in L2-L3 (15 TL and 2 TF) and 9 in L1-L2 (7 TL and 2 TF) intervertebral disk spaces.
The highest visual analog score before the injection and the lowest visual analog score after the injection for both TL and TF injections were 10 and 6; the mean VAS’s before and after the injections were 8.9 ± 1.1 and 4.8 ± 2.5 respectively (p<0.001).
There were 276 (216 TL and 60 TF) of 428 injections in group A (64.5%), 66 injections (52 TL and 14 TF) in group B (15.5%) and 86 injections (57 TL and 29 TF) in group C (21%) according to the reduction of VAS’s before and after injections.
In 325 TL injections 216 (66.5%) were in group A, 52 (16.0%) were in group B and 57 (17.5%) were in group C. In 103 TF injections 60 (58.2%) were in group A, 14 (13.6%) were in group B and 29 (28.2%) were in group C.
The mean follow-up time for all injections was 12 months. The longest pain relief time was 16 months for group A TL injections and 18 months for group A TF injections. The shortest pain relief time was 2 weeks for group A TL injections and 1 month for group A TF injections. 216 TL injections provided up to average 5.5 months and 60 TF injections up to average 5.6 months of pain relief.
In 23 of 310 patients epidural injections were repeated in different times during study and 73 epidural injections (n: 61 translaminar and n: 12 transforaminal) were performed. There were 63 of 73 injections in group A (86%), 3 in group B (4%) and 7 in group C (7%).
Discussion
After the first introduction of ESIs for the treatment of lumbosacral radicular pain in 1950, recently the use of these injections for treating spinal or radicular pain are increasing [10]. Many investigators have investigated the effectiveness of procedure for the treatment of lumbosacral or cervical radiculopathy, and lumbar spinal stenosis [11-17]. The current literature reports success rates up to 100% for ESIs, depending on methodology, outcome measures, patient selection, and technique [18]. The technical success was 100% in our study. Definitely the main proportion to reach this success belongs to imaging modalities such as CT and CT fluoroscopy. The major concern about the use of CT instead of conventional fluoroscopy is radiation exposure. Recently Chang et al. published a retrospective study, including 345 patients, that report average exposure radiation dose during ESI were 1.34 ± 0.05 mSv while using an intermittent scanning mode (dose CT). This study partially eliminates the concerns about CT and supports the use of it when we take into considers the benefits of CT.
The current literature represents that ESIs can offer short-term pain reduction. In addition, it is a safe procedure with low complication rates. Although the articles, which report the effectiveness of procedure, include small number of patients, there have been reviewed articles states ESI is an effective method in short term pain reduction. To our knowledge, our study is one of the largest series including 310 patients, and indicates the midterm result of procedure. The highest visual analog score before the injection and the lowest visual analog score after the injection for both translaminar and transforaminal injections were 10 and 6; the mean VAS’s before and after the injections were 8.9 ± 1.1 and 4.8 ± 2.5 respectively (p<0.001). The reduction of VAS’s was higher than 50% in 276 (216 TL and 60 TF) of 428 injections (64.5%). Limited reduction (lower than 50%) was achieved in 66 injections (52 TL and 14 TF) (15.5%), and no response to treatment was in 86 injections (57 TL and 29 TF) (21%). There was no major complication related to needle placement or drug administration. There were 27 (6.3%) minor complications (n: 3 orthostatic hypotension (0.7%), 24 transient motor weaknesses of lower extremities (5.6%). Transient motor weakness is a side effect because of the using local anesthetic and all of the resolved in 4-5 h. If patients had low blood pressure or were blackout, hypertonic mai was injected. The mean follow-up time for all injections was 12 months. The pain relief times ranges between 2 w and 18 months.
The mean pain relief times were 5.5 months and 5.6 months for TL and TF injections, respectively. These results are compatible with the literature, and confirm the knowledge about EPI that it can provide short-term pain relief, and has significant clinical and social benefits to the patients who suffer from lumbosacral radicular pain. Although mean pain relief period seems to be short, repeatability and safety of procedure can overcome this relative limitation. Another important point is the cost-effectiveness of this repeatable procedure. To date, there have been no cost-effectiveness studies of ESIs in the literature.
In conclusion; our study, which includes the most large patients groups in the literature, confirms that ESIs is an effective, safe and repeatable procedure for treatment of spinal pain. Also our study supports the widespread acceptance of procedure.
References
- Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician 2003; 6: 3-80.
- Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systemic review of the literature. Spine 1999; 24: 1813-1819.
- Helliovaara M, Knekt P, Aroma A. Incidence and risk factors of herniated lumbar intervertebral disc or sciatica leading hospitalization. J Chronic Dis 1987; 40: 251-258.
- Chou R, Huffman L. Guideline for the Evaluation and Management of Low Back Pain: Evidence Review. Am Pain Soc Glenview IL 2009.
- Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: A ten-year perspective. Pain Physician 2010; 13: 401-435.
- Manchikanti L. The growth of interventional pain management in the new millennium: A critical analysis of utilization in the Medicare population. Pain Physician 2004; 7: 465-482.
- Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL. Epidural steroids in the management of chronic spinal pain: A systematic review. Pain Physician 2007; 10: 185-212.
- Andrew L Wagner. CT fluoroscopy-guided epidural injections: technique and results. AJNR Am J Neuroradiol 2004; 25: 1821-1823,
- Manchikanti L, Singh V, Derby R, Schultz DM, Benyamin RM, Prager JP. Reassessment of evidence synthesis of occupational medicine practice guidelines for interventional pain management. Pain Physician 2008; 11: 393-482.
- Lievre JA, Block-Michel H. Linjection transsacree. Bull Soc Med Paris 1957; 73: 1110-1118.
- Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil 2002; 81: 898-905.
- Rydevik BL, Cohen DB, Kostuik JP. Spine epidural steroids for patients with lumbar spinal stenosis. Spine 1997; 22: 2313-2317.
- Banaszkiwicz PA, Kader D, Wardlaw D. The role of caudal epidural injections in the management of low back pain. Bull Hosp Jt Dis 2003; 61: 127-131.
- Carrette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierra A. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med 1997; 336: 1634-1640.
- Nelemans PJ, de Bie RA, de Vet HC, Sturmans F. Injection therapy for subacute and chronic benign low back pain. Spine 2001; 26: 501-515.
- Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain 1998; 14: 148-151.
- Butterman GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am 2004; 86: 670-679.
- Cluff R, Mehio AK, Cohen SP, Chang Y, Sang CN, Stojanovic MP. The technical aspects of epidural steroid injections: a national survey. Anesth Analg 2003; 95: 403-408.