ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 2
The effects of a pulmonary rehabilitation program on exercise tolerance, quality of life, sleep quality and emotional status in the patients with Parkinson's disease
1Department of Neurology, Sakarya University, Research and Training Hospital, Sakarya, Turkey
2Department of Pulmonology, Sakarya University, Research and Training Hospital, Sakarya, Turkey
3Department of Physical Medicine and Rehabilitation, Sakarya University, Research and Training Hospital, Sakarya, Turkey
- *Corresponding Author:
- Belma Gungen
Department of Neurology, Sakarya University
Research and Training Hospital, Turkey
Accepted date: June 27, 2016
Introduction: We aimed in the present study to investigate the effects of pulmonary rehabilitation on the respiratory parameters and effort capacity, quality of life (QoL), anxiety, depression, and sleepiness in the patients with Parkinson's disease (PD).
Methods: The study included 34 mobilized patients with PD. Patients underwent a 12-week pulmonary physiotherapy (PPT). Pulmonary function tests (PFT), six-minute walk test (6mWT), Hoehn and Yahr Scale (HYS), Unified Parkinson's Disease Rating Scale (UPDRS), QoL, Parkinson's Disease Questionnaire (PDQ), Beck Anxiety Inventory (BAI), Beck Depression Inventory (BDI), and Epworth Sleepiness Scale (ESS) scores were evaluated before and after PPT.
Results: PPT improved parameters of PFT significantly, and caused an increase of about 35 m in the 6mWT (p<0.001). HYS (p=0.002), UPDRS, QoL, PDQ, BAI, BDI and ESS scores were found to improve significantly after the PPT (p<0.001 for all).
Conclusion: Results of our study indicated that PPT is effective significantly and positively especially on the non-motor complications, by increasing effort capacity and walking distance in the patients with PD.
Keywords
Parkinson's disease, Pulmonary rehabilitation, Anxiety, Depression, Sleepiness, Quality of life.
Introduction
Parkinson’s disease (PD) is a chronic and progressive neurodegenerative condition, affecting approximately 10 million people worldwide [1]. People with PD have more motor and autonomic, cognitive, behavioural and sensorial complications. The motor complications include tremor, rigidity, bradykinesia, decreased pulmonary capacity and deterioration of muscle strength, balance and walking performance, while the non-motor complications include autonomic dysfunction, fatigue, apathy, sensory complaints, sleep disturbances, depression, cognitive dysfunction and ultimately decreased quality of life (QoL) [2,3]. Because of these physical insufficiencies, patients with PD maintain sedentary lives, with less motor activity [4]. This life style causes social isolation, and increased dependency to others, leading to a vicious cycle that worsens the emotional disorder and life quality.
Another important reason of inactivity in PD patients is the respiratory complication that leads to decreased effort capacity. Respiratory involvement with PD could occur through both peripheral and central mechanisms. Motor manifestations such as rigidity, tremor and weakness affect the upper airway and the respiratory pump muscles. Non-motor brain stem involvement has effect at the level of respiratory control [5]. In addition to these ventilatory abnormalities, evidences of a high incidence of obstructive and restrictive pulmonary dysfunction were found [6,7]. Exercise therapy poses the potential to improve many clinical domains of PD [8]. Indeed studies on PD have shown improvements of muscle strength, cardio respiratory fitness, balance, walking performance, and QoL, following exercise therapy [2]. In the previous studies, it has been reported that pulmonary rehabilitation improves the PFT parameters, and increases the scores of six-minute walk test (6mWT) [9,10]; however, as far as we know, a study is not available indicating the effects of pulmonary rehabilitation on the emotional status and sleep quality.
In our study, we aimed to investigate effects of the increased effort capacity and mobilization by pulmonary physiotherapy (PPT), on the general and Parkinson-specific life qualities, emotional status, and sleep quality.
Materials and Methods
From April 2014 to April 2015, 123 consecutive PD outpatients were recruited at regular check-ups at the Department of Neurology Clinic, Sakarya University Medical Faculty (Turkey). The diagnosis was made according to the United Kingdom Parkinson's Disease Society Brain Bank criteria. Participants were evaluated for disease severity using the Unified Parkinson’s Disease Rating Scale (UPDRS) [11] in the “on-state” and Hoehn and Yahr Scale (HYS) [12]. All patients were clinically stable (without fluctuations or dyskinesia). Accompanying malignancy, congestive heart failure, insulin-dependent diabetes mellitus, inflammation, infection, neurological dysfunction, severe depression, dementia and other conditions that could influence the mobility status were excluded from the study. Pulmonary system was evaluated in detail in all patients, by a specialist in chest diseases. All pulmonary function tests (PFT) were carried out by the same technician in accordance with the directives of the American Thoracic Society.
Patients with asthma-COPD and obstructive pulmonary disease were not included in the study. Cases, who have previously participated in an exercise program, and those receiving drugs for anxiety, depression and sleep disturbances, were also excluded. The remaining 45 patients with mental and cognitive status suitable for physiotherapy (mini mental state examination ≥ 24), have undergone 6mWT according to the standard protocol [13]. The level of quality of life was assessed by means of the quality of life scale in Parkinson’s Disease Questionnaire (PDQ-39) [14]; it is a 39-item self-report questionnaire which measures eight dimensions of health, namely mobility, activities of daily living, emotional wellbeing, stigma, social support, cognition, communication, and bodily discomfort. Higher score of PDQ-39 indicates poorer QoL in PD patients. This scale evaluates the effect of Parkinson’s disease on the quality of life, within the last one month.
For evaluation of quality of life (QoL), Short Form-36 (SF-36) was used. The SF-36 Health Survey questionnaire was used to measure health-related QoL [15]. It is composed of 36 items, addressing eight dimensions of QoL: physical functioning, physical role limitations, bodily pain, general health, vitality, social functioning, emotional role limitations and mental health. These scores range from 0 to 100, with higher scores representing better health quality. For evaluation of emotional status, Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) were used [16,17]. The BAI and BDI are widely used, 21-item standardized self-administered questionnaires that measure various symptoms of anxietydepression and describe the somatic and cognitive-affective symptoms on a four-point scale that ranges from 0 to 3. A higher score indicates a more severe depression. The sleep quality was assessed by the Epworth Sleepiness Scale (ESS) [18]. Epworth 0-10 was categorized as mild, and over 10 was categorized as severe.
Patients were administered 12-week exercise program by an experienced pulmonary physiotherapist. During the exercise program, pursed lips pulmonary, and diaphragmatic pulmonary exercises were applied, after training. PFT, 6mWT, QoL, UPDRS, HYS, PDQ-39, SF-36, BAI, BDI, and ESS were evaluated before and after the exercises. Six of the patients were excluded from the study because of the alteration in treatment dose during the follow-up period, three cases were excluded due to the inability in applying physiotherapy program, and two cases were excluded because of not attending to controls. The study was completed with the participating 34 patients. Ethical approval for the study was granted by the Sakarya University Ethics Committee. All patients were informed about the aim of the study, and written consent was obtained.
Statistical analysis
Statistical analyses were carried out using the SPSS/PC software (version 21.0). Descriptive statistics were presented as mean values with a standard deviation for numeric variables. The paired-samples t-test for comparison of parametric data among groups. The limit for statistical significance was accepted as p<0.05.
Results
Of the original sample of 129 PD patients, 45 patients met the inclusion criteria. An additional 11 patients were excluded because of missing data. This resulted in a total sample size of 34 patients. The demographics and clinical features of patients are listed in Table 1.
| Mean ± SD | Min-max | ||
|---|---|---|---|
| Male/Female | 21/13 | ||
| Age | 68.21 ± 12.20 | 48-86 | |
| Disease duration (yr) | 5.8 ± 4.4 | 20-Mar | |
| Age of onset (yr) | 62.94 ± 12.8 | 34-84 | |
| UPDRS | 31.7 ± 10.03 | Oct-46 | |
| HYS | 1.6 ± 0.4 (median: 2) | 1-2.5 | |
| UPDRS: Unified Parkinson’s Disease Rating Scale; HYS: Hoehn and Yahr Stage. | |||
Table 1. Demographic and clinical characteristics of the subjects.
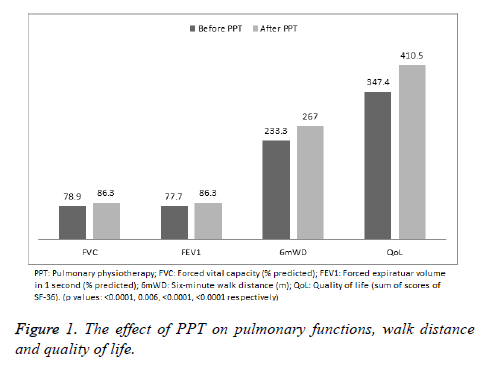
Spirometric parameters of the patients improved significantly following the PPT. The mean value of FEV1 increased from 77.6, to 86.3. Similarly, FVC also increased from 78.85 to 86.97. The walking distance increased significantly in the 6mWT performed after physiotherapy, from the mean value of 233 m, to 269 m as shown in Figure 1.
The overall life quality and the anxiety-depression scores of patients improved significantly following PPT. Results are illustrated in Table 2.
| Before PPT | After PPT | Difference | p value | |
|---|---|---|---|---|
| UPDRS | 31.7 ± 10.03 | 25.6 ± 9.6 | -6.35 | <0.0001 |
| HYS | 1.6 ± 0.4 | 1.6 ± 0.4 | 0 | 0.002 |
| PDQ-39 | 59.3 ± 39.5 | 52.4 ± 37.3 | -6.912 | <0.0001 |
| BAI | 20.09 ± 12.2 | 16.91 ± 11.0 | -3.176 | <0.0001 |
| BDI | 18.74 ± 12.45 | 16.21 ± 12.33 | -2.529 | <0.0001 |
| ESS | 8.82 ± 4.54 | 7.26 ± 4.22 | -1.559 | <0.0001 |
| BAI: Beck Anxiety Inventory; BDI: Beck Depression Inventory; ESS: Epworth Sleepiness Scale; Data are shown as mean ± SD. | ||||
Table 2. The effect of PPT on clinical characteristics, emotional status and sleep quality of subjects.
Discussion
Likely, our study is the first to prospectively demonstrate improved QoL, anxiety, depression, sleepiness, 6mWT, spirometry and UPDRS in individuals with PD after participation in a Pulmonary rehabilitation program. Our results have confirmed the views that respiratory parameters of the patients would improve, their effort capacities would increase resulting in decreases of dependency and social isolation, which might improve quality of life in these cases, and additionally anxiety-depression and sleepiness might decrease, following a PPT program. Anxiety and depression exists more frequently in the patients with PD, compared to the general population [19], and this affects life quality of the patients negatively [20]. In large serial studies, rates of anxiety and depression have been reported to be 45%-51% and 35%-45%, respectively [19,21,22]. We determined signs of anxiety and depression in 64.7%, and 41.1% of the patients in our study, respectively.
The mechanisms of mood disorders in the patients with PD have not been clarified yet [23]. Possessing a chronic and progressive disease may lead to anxiety and depression, and debilitating and unpredictable motor symptoms may also contribute to this [24]. However mood disorders in PD cannot be solely explained by the psychological response to the diagnosis of PD, since anxiety and depression are reported more frequently in PD compared to patients with other similarly chronic and debilitating diseases [23]. The dopaminergic neurotransmitter alterations can be directly related to anxiety symptoms in PD [23]. Furthermore studies suggest possible associations with both serotonergic and noradrenergic systems and white-matter abnormalities. On the upshot it is largely attributed to a combination of neurobiological and psychological causes [23]. Whatever the cause may be, PPT was determined to affect anxiety and depression significantly in our study, and rates of anxiety and depression decreased to 44.1% and 32.3%, respectively following PPT (p<0.001). We could not reach a study in the literature evaluating the effect of PPT on psychological status. However in the previous studies, activities like exercising and dancing were shown to decrease anxiety and depression [25-27]. This fact can be explained by positive effect of the increased capability of activity, on the mood.
Insomnia and excessive daytime sleepiness (EDS) is an increasingly recognized problem in PD, and it causes clinically significant problems and impairs the quality of life of patients [28,29]. EDS affects up to 50% of Parkinson’s disease patients and is 15-fold more frequent in PD patients than in the agematched healthy subjects [30]. Epworth Sleepiness Scale has been reported to be reasonably well to evaluate excessive daytime sleepiness in PD [31]. In our study, ESS score was found to be 8.82 prior to PPT, and 41.1% of the patients were found to exist with EDS. Following PPT, the mean ESS score decreased to 7.26, and rate of EDS decreased to 20.5%; the differences were found to be significant (p<0.0001). In a recent general population-based study, exercise was shown to exert positive effect on EDS [32]. However a study evaluating the effect of PPT is not available yet. Besides physical activity, PPT may help to decrease sleep disturbances also by decreasing anxiety, and by its positive effects on the respiratory parameters. Quality of life has become an increasingly important parameter in the evaluation of the efficacy of interventions in patients suffering from Parkinson's disease. Multiple studies, using a variety of approaches and methods, have shown a reduction of QoL in PD patients [33]. In our study, overall life quality and also Parkinson-specific life quality improved significantly after the PPT (p>0.001 and p<0.0001, respectively).
Systematic reviews have indicated non-motor symptoms [including depression and anxiety] as major factors in determining health-related quality of life, progression of disability, and home nursing in PD patients [34]. A significant relationship between postural instability, gait dysfunction dominant symptoms and anxiety is also observed [24]. Furthermore exercise was indicated to increase PDQ in the randomized studies [35], and thus increased walking distance and decreased anxiety may improve quality of life. UPDRS score decreased significantly following PPT in our study; this decrease may be explained by the decreases in anxiety and depression in these patients. Negative effect of anxiety on the motor symptoms is well-known [24]. In the metaanalyses, exercise has been determined to decrease depression in the patients with neurological disorders [36]. Moreover Klusevky et al. have shown that treatment of depression in PD patients by sertraline exerts positive effects on motor functions, and improves UPDRS score compared to basal level [37]. Recent studies also demonstrated that exercise decreases UPDRS scores [35].
Respiratory function parameters were shown to be impaired in PD, compared to normal population [7,38]. However number of studies investigating the effects of pulmonary rehabilitation programs is considerably limited. Koseoglu et al. have reported that some of the PFT parameters improve with PPT [9]. Significantly different FEV1 and FVC values determined in our study may contribute to the literature in this regard. In PD patients, the reduction in walking capacity is an important factor that negatively affects the perception of QoL [39]. In the study of Cagusi et al., in addition to improvements in the scores of PDRS-III, BDI and PDQ, a significant increase in walking distance was observed with the tailored exercise program [40]. In our study, walking distance increased about 35 m with PPT, and this difference was significant. This increase may be the main cause of all improvements in the patients. There are several limitations to this study. The lack of a non-physiotherapy control group does not allow direct comparison of PPT versus no PPT. Furthermore, we did not have a follow-up period to determine whether the effects of PPT lasted over time.
Evidences from published trials and guidelines have suggested potential benefits of physiotherapy for patients with Parkinson’s disease [41,42]. Referral rates for physiotherapy in Parkinson’s disease are low [41], and the main objective of rehabilitation in PD is usually to recover motor function; however our study has demonstrated that PPT application in PD is also effective in decreasing the non-motor symptoms (including anxiety, depression, and sleepiness), and in increasing the quality of life. As a conclusion, addition of pulmonary exercises to the physical therapy program of the patients with Parkinson’s disease, suggests potential benefits.
Author Roles
Design: BDG, YA; data acquisition: BDG, YGA, ACG; DD, SB; statistical analysis: YA; first draft of the manuscript: YA. All authors reviewed and commented on the final manuscript.
Conflicts of Interest
The authors declare that they have no conflicts of interest in relation to this article.
References
- Foundation PsD Understanding Parkinsons 2014.
- Uhrbrand A, Stenager E, Pedersen MS, Dalgas U. Parkinsons disease and intensive exercise therapy-a systematic review and meta-analysis of randomized controlled trials. J Neurol Sci 2015; 353: 9-19.
- Zhang N, Liu W, Ye M, Cohen AD, Zhang Y. The heterogeneity of non-motor symptoms of Parkinsons disease. Neurol Sci 2015; 36: 577-584.
- Nimwegen M, Speelman AD, Hofman EJ. Physical inactivity in Parkinsons disease. J Neurol 2011; 258: 2214-2221.
- Seccombe LM, Giddings HL, Rogers PG. Abnormal ventilatory control in Parkinsons disease-further evidence for non-motor dysfunction. Respir Physiol Neurobiol 2011; 179: 300-344.
- Sabate M, Gonzalez I, Ruperez F, Rodríguez M. Obstructive and restrictive pulmonary dysfunctions in Parkinsons disease. J Neurol Sci 1996; 138: 114-119.
- Sathyaprabha TN, Kapavarapu PK, Pall PK, Thennarasu K, Raju TR. Pulmonary functions in Parkinsons disease. Indian J Chest Dis Allied Sci 2005; 47: 251-257.
- Pelosin E, Faelli E, Lofrano F, Avanzino L, Marinelli L, Bove M, Ruggeri P, Abbruzzese G. Effects of treadmill training on walking economy in Parkinsons disease: a pilot study. Neurol Sci 2009; 30: 499-504.
- Koseoglu F, Inan L, Ozel S. The effects of a pulmonary rehabilitation program on pulmonary function tests and exercise tolerance in patients with Parkinsons disease. Funct Neurol 1997; 12: 319-325.
- Frazzitta G, Maestri R, Bertotti G. Intensive rehabilitation treatment in early Parkinsons disease: a randomized pilot study with a 2-year follow-up. Neurorehabil Neural Repair 2015; 29: 123-131.
- Fahn S, Elton RL. Recent Developments in Parkinsons Disease. Macmil Health Info 1987; 2: 153-163.
- Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. Neurol 1967; 17: 427-442.
- American Thoracic Society Statement Guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111-117.
- Martinez-Martin P, Jeukens-Visser M, Lyons KE. Health-related quality-of-life scales in Parkinsons disease: critique and recommendations. Mov Disord 2011; 26: 2371-2380.
- Gazibara T, Pekmezovic T, Kisic Tepavcevic D. Health-related quality of life in patients with Parkinsons disease: Implications for falling. Parkinsonism Relat Disord 2015; 21: 573-576.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56: 893-897.
- Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. J Clin Psychol 1984; 40: 1365-1367.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 1991; 14: 540-545.
- Rutten S, Ghielen I, Vriend C. Anxiety in Parkinsons disease: Symptom dimensions and overlap with depression and autonomic failure. Parkinsonism Relat Disord 2015; 21: 189-193.
- Rodriguez-Violante M, Cervantes-Arriaga A, Corona T. Clinical determinants of health-related quality of life in Mexican patients with Parkinsons disease. Arch Med Res 2013; 44: 110-114.
- Negre-Pages L, Grandjean H, Lapeyre-Mestre M. Anxious and Depressive Symptoms in Parkinsons Disease: The French Cross-Sectionnal DoPAMiP Study. Mov Disord 2010; 25: 157-166
- Reijnders JS, Ehrt U, Weber WE. A systematic review of prevalence studies of depression in Parkinsons disease. Mov Disord 2008; 23: 183-189
- Dissanayaka NN, White E, OSullivan JD. The clinical spectrum of anxiety in Parkinsons disease. Mov Disord 2014; 29: 967-975
- Burn DJ, Landau S, Hindle JV. Parkinsons disease motor subtypes and mood. Mov Disord 2012; 27: 379-386.
- Blonder LX, Slevin JT. Emotional dysfunction in Parkinsons disease. Behav Neurol 2011; 24: 201-217.
- Adamson BC, Ensari I, Motl RW. Effect of exercise on depressive symptoms in adults with neurologic disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil 2015; 96: 1329-1338.
- Hackney ME, Earhart GM. Effects of dance on movement control in Parkinsons disease: a comparison of Argentine tango and American ballroom. J Rehabil Med 2009; 41: 475-481.
- Ylikoski A, Martikainen K, Sieminski M, Partinen M. Parkinsons disease and insomnia. Neurol Sci 2015; 36: 2003-2010.
- Pellecchia MT, Antonini A, Bonuccelli U. Observational study of sleep-related disorders in Italian patients with Parkinsons disease: usefulness of the Italian version of Parkinsons disease sleep scale. Neurol Sci 2012; 33: 689-694.
- Knie B, Mitra MT, Logishetty K, Chaudhuri KR. Excessive daytime sleepiness in patients with Parkinsons disease. CNS Drugs 2011; 25: 203-212.
- Santamaria J. How to evaluate excessive daytime sleepiness in Parkinsons disease. Neurol 2004; 63: 21-23.
- Andrianasolo RM, Menai M, Galan P. Leisure-Time Physical Activity and Sedentary Behavior and Their Cross-Sectional Associations with Excessive Daytime Sleepiness in the French SUVIMAX-2 Study. Int J Behav Med 2015; 7.
- Gustafsson H, Nordstrom P, Strahle S, Nordstrom A. Parkinsons disease: a population-based investigation of life satisfaction and employment. J Rehabil Med 2015; 47: 45-51.
- Burn DJ, Landau S, Hindle JV. Parkinsons disease motor subtypes and mood. Mov Disord 2012; 27: 379-386.
- King LA, Wilhelm J, Chen Y. Effects of Group, Individual, and Home Exercise in Persons With Parkinson Disease: A Randomized Clinical Trial. J Neurol Phys Ther 2015; 39: 204-212.
- Adamson BC, Ensari I, Motl RW. Effect of exercise on depressive symptoms in adults with neurologic disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil 2015; 96: 1329-1338.
- Kulisevsky J, Pagonabarraga J, Pascual-Sedano B. Motor changes during sertraline treatment in depressed patients with Parkinsons disease. Eur J Neurol 2008; 15: 953-959.
- Wang Y, Shao WB, Gao L. Abnormal pulmonary function and respiratory muscle strength findings in Chinese patients with Parkinsons disease and multiple system atrophy--comparison with normal elderly. PLoS One 2014; 9: 116123.
- Scalzo PL, Flores CR, Marques JR. Impact of changes in balance and walking capacity on the quality of life in patients with Parkinsons disease. Arq Neuropsiquiatr 2012; 70: 119-124.
- Cugusi L, Solla P, Zedda F. Effects of an adapted physical activity program on motor and non-motor functions and quality of life in patients with Parkinsons disease. Neur Rehabilit 2014; 35: 789-94.
- Tomlinson CL, Patel S, Meek C. Physiotherapy intervention in Parkinsons disease: systematic review and meta-analysis. BMJ 2012; 6: 5004.
- Vitale C, Agosti V, Avella D. Effect of Global Postural Rehabilitation program on spatiotemporal gait parameters of parkinsonian patients: a three-dimensional motion analysis study. Neurol Sci 2012; 33: 1337-1343.