ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 4
The effects of preoperative smoking cessation on the healing of fractures and postoperative complications: A systematic review and meta-analysis
1The Fifth Affiliated Hospital of Zunyi Medical University, Zhuhai, China
2Shenzhen Children’s Hospital, China
3Affiliated Hospital of Zunyi Medical College, China
- *Corresponding Author:
- Wei Min
The Fifth Affiliated Hospital of Zunyi Medical University
Zhuhai, China
Accepted date: October 3, 2016
Introduction: Smoking is a known risk factor for fracture healing and postoperative complications. However, most evidence upon the association between bone healing and smoking was investigated in retrospective studies or laboratory-based animal studies. This meta-analysis evaluated the clinical efficacy of preoperative smoking cessation on the healing of fractures and postoperative complications.
Evidence Acquisition: MEDLINE, EMBASE, CNKI and the Cochrane Database were retrieved for identifying relevant study. Four studies, including three Randomized Controlled Clinical Trials (RCTs) and one Non-Randomized Concurrent Controlled Trial (NRCCTs), involving a total of 510 patients, were included.
Evidence Synthesis: In the patients with preoperative smoking cessation, the risk of overall postoperative complications was lower (Risk Ratio (RR) 0.37; 95% Confidence Interval (CI) 0.26 to 0.52; P=0.49) when compared with the patient without smoking cessation. Preoperative smoking cessation reduced the risk of wound-related complications ((RR) 0.21; 95% (CI) 0.11 to 0.39; P=0.42), recurrent surgery ((RR) 0.23; 95% (CI) 0.08 to 0.67; P=0.42) and additional complications ((RR) 0.41; 95% (CI) 0.25 to 0.67; P=0.85). One NRCCT showed that the risks of fracture non-union (P=0.03) and osteomyelitis (P=0.49) in the patients with preoperative smoking cessation were reduced.
Conclusion: Our study supports the role of preoperative smoking cessation on orthopaedic surgery outcomes.
Keywords
Preoperative smoking cessation, Fractures healing, Postoperative complications, Meta-analysis.
Introduction
Smoking continues to induce serious health consequences worldwide. A large amount of evidence supports the fact that smoking is associated with chronic diseases and cancer [1]. Similarly, smokers have been observed to have higher rates of fracture non-union and other serious postoperative complications [2,3]. Additionally, a recent estimate of worldwide health-related costs has showed that smoking related complications caused $193 billion extra costs, annually [4]. In orthopaedic surgical procedures, the effects of smoking on bone healing and postoperative complications are inconsistent. There were non-significant trends between increased hospital stay and fractures union, increased postoperative rates of superficial and deep infections [5]. Smoking cessation is widely believed to be an effective measure to decrease the incidence of postoperative complications including: general morbidity, wound complications, general infections, pulmonary complications, neurological complications, and admission to the Intensive Care Unit (ICU) [6,7]. Furthermore, longer periods of smoking cessation provide better surgery outcomes [8]. During the last few years, some researches have shown that smoking cessation improving bone healing and reducing preoperative complications in various orthopaedic surgical procedures [2,3,9,10]. Following the recent evidences in the published literature, we investigated the associations between smoking cessation and the healing of fractures and the development of postoperative complications by conducting a meta-analysis of Randomized Controlled Trials (RCTs) and Non-Randomized Concurrent Control Trial (NRCCT).
Evidence Acquisition
Literature search
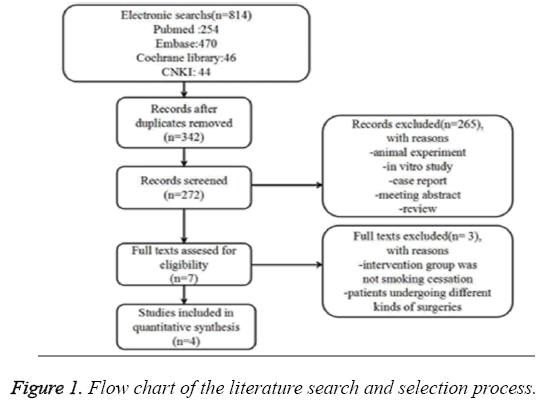
A systematic search of the databases MEDLINE, EMBASE, China National Knowledge Infrastructure (CNKI) and the Cochrane Database for all the original published studies was conducted up to February 2016. The flow of selecting studies for this systematic review and meta-analysis is shown in Figure 1. The relevant search terms were ‘smoking’ and ‘cessation’; ‘smoking’ and ‘abstinence’; ‘cigarette’ and ‘cessation’; ‘postoperative’ or ‘pre-operative’; ‘bone’ and ‘healing’; ‘fracture’ and ‘healing’ or ‘complications’. All manuscripts were reviewed to select those that met the requirements.
Study selection
Published studies were eligible for meta-analysis if they met the following criteria: (1) Type of research: Randomized Controlled Trials (RCTs) and Non-Randomized Concurrent Control Trial (NRCCT); (2) Participants: patients who underwent orthopaedic surgery including open reduction and internal fixation, hip or knee arthroplasty and who had a record of smoking status and history; (3) Intervention: preoperative smoking cessation, including all types of preoperative smoking cessation therapy; (4) Outcomes: radiologically-confirmed union of fracture. Overall rates of preoperative complications and the incidence of each complication were described; (5) full texts should be available.
Data extraction
The following information was independently extracted by two authors, including basic information (including authors and year of publication), study design, fracture location, treatment method (operation technique and others), number of participants, interventions, smoking status, history of diseases, preoperative smoking cessation period and follow-up duration. Disagreements were resolved by consensus.
Cochrane collaboration's tool was used to assess the risk of bias in each RCT, to provide a qualification of risk of bias. For analysis of the NRCCTs, we used the Methodological Index for Non-Randomized Studies (MINORS) guidelines to assess the methodological quality [11]. The MINORS guidelines consisted of 12 indexes: every item has two scores and the total score is 24; when the score is ≥ 16 points this indicated a high quality study; otherwise the quality was low (<16 points).
Levels of evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system was used to rate the level of evidence and strength of recommendation [12]. GRADE profiler 3.6 software was used to create the evidence profile.
Evidence synthesis
All statistical analysis was performed using the Cochrane Review Manager 5.3 software to generate forest plots and assess the heterogeneity of the included studies. The effect was measured as Risk Ratio (RR) with 95% Confidence Intervals (CIs), and pooled estimates were computed according to a fixed-effects model. Chi2 and I2 statistic were used to qualified heterogeneity, so that I2 ≤ 25% and Chi2 (P>0.5) indicated no evidence of heterogeneity. Sensitivity analysis was performed to explore possible explanations for heterogeneity. The robustness of the main results was tested by removing each single study in turn. The results from only RCTs were pooled by meta-analysis to ensure appropriate statistical outcomes analysis both clinically and statistically.
Results
Search results
We identified seven potentially relevant studies including 5 Randomized Controlled Trials (RCTs) and 2 Non-Randomized Concurrent Control Trials (NRCCT) of preoperative smoking cessation and bone healing. Of these seven studies, three were excluded because the operative procedure contained not only orthopaedic procedures but also general surgery or other surgical procedures [6,7], or the patients undergoing orthopaedic surgery were second-hand smokers [13]. The four left studies [2,3,9,10] including three RCTs and one NRCCT were chosen for the final analysis (Figure 1). The characteristics and quality assessment of each study are presented in Table 1.
| First author | Study design | Surgery/Fracture location | Treatment method (operation technique and others) | No.of patients | Male sex (%) | Mean age (y) | Smoking status | Interventions | Preoperative smoking cessation period |
History of disease | Follow-up period post-surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Moller | RCT | Knee Hip |
Knee/hip replacement | 108 | 43 | IG: 66 (41-83) CG: 64 (30-85) |
IG:15 (5-30) cigarettes per day; (11-65) pack years# CG:15 (3-30)cigarettes per day; (1-102) pack years |
IG: smokers received smoking cessation 6-8 week preoperatively CG: smokers did not receive any intervention before surgery | 6-8 week | Chronic heart disease Chronic obstructive Lung disease Diabetes mellitus |
4week |
| Nasell | RCT | Ankle Hip Tibia/knee Foot Upper extremity |
Open reduction internal fixation Closed reduction internal fixation Closed reduction external fixation Hip/Shoulder arthroplasty |
104 | 30 | IG: 54.7 ±2.2 CG: 51.5 ±2.0 |
IG: 21.5 ± 11.8 cigarettes per day; 12.8 ± 5.7 pack years CG:21.5 ± 16.2 cigarettes per day; 13.2 ± 6.3 pack years |
IG: smokers received smoking cessation 6 week preoperatively CG: smokers did not receive any intervention before surgery |
6 week | Heart disease Lung disease Diabetes mellitus Depression High blood pressure |
12week |
| Pei | RCT | Knee Hip |
Knee/Hip replacement | 113 | 100 | IG: 67±8 CG: 65±9 |
IG:15 cigarettes per day; 35 pack years CG:15 cigarettes per day; 37 pack years |
IG: smokers received smoking cessation 4 week preoperatively CG: smokers did not receive any intervention before surgery |
4 week | Chronic heart disease Chronic obstructive lung disease Diabetes mellitus |
Not reported |
| Castilo | NRCCT | Lower extremitybelow the distal femur excluding foot | Fracture debridement Antibiotic coverage Fracture stabilization Early soft tissue coverage Stimulation procedures§ |
187 | 73 | 33.4 | IG: ex-smoker CG:100 or more cigarettes over the course of one's lifetime |
IG:information on time since quitting smoking was not quantitative$ CG: smokers did not receive any intervention before surgery |
Month/decades | Not reported | 2years |
Table 1: Characteristics of included studies.
These four studies were performed in the USA [2], Denmark [9], Sweden [3], and China [10], respectively, during the period between 2002 and 2014. The total number of patients in each study ranged from 105 to 187. The quality of each RCT was assessed by the Cochrane bias risk assessment tools (Table 2). According to the Methodological Index for Non-Randomized Studies (MINORS) evaluation criteria [11], only the NRCCT scored 20 points. The items of deduction were summarized as follows: 1) loss rate in the follow-up was greater than 5% in both ‘preoperative smoking cessation’ group (14.6%) and the ‘continued smoking ‘ group (23.8%); 2) no prospective calculation on the sample size (Table 3).
| First author | Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blanding of participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias |
|---|---|---|---|---|---|---|---|
| Moller | + | - | - | + | + | + | ? |
| Nasell | + | + | ? | + | + | + | ? |
| Pei | + | + | + | + | + | + | ? |
Table 2: Risk of bias assessment for randomized control trial.
| First author | Castilo |
|---|---|
| A clearly stated aim | + |
| Inclusion of consecutive patients | + |
| Prospective collection of data | + |
| Endpoints appropriate to the aim of the study | + |
| Unbiased assessment of the study endpoint | + |
| Follow-up period appropriate to the aim of the study | + |
| Loss to follow-up less than 5% | - |
| Prospective calculation of the study size | - |
| Adequate control group | + |
| Contemporary groups | + |
| Baseline equivalence of groups | + |
| Adequate statistical analyses | + |
Table 3: Methodological quality assessment for non-randomized concurrent control trial.
Overall incidence of postoperative complications
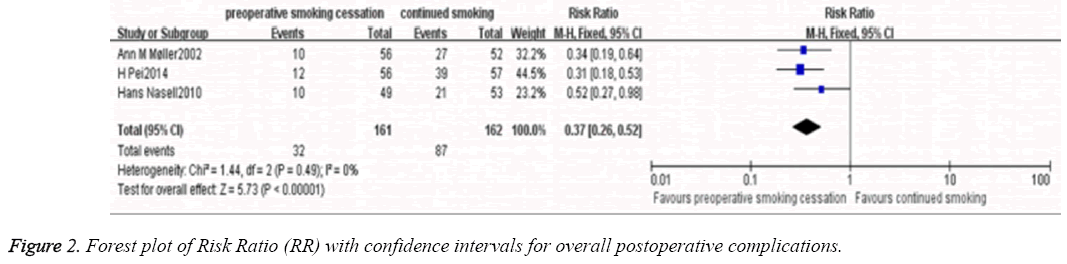
Meta-analysis of the three RCTs [3,9,10] was performed using a fixed-effects model (P=0.49; I2 =0%). The results of overall incidence of postoperative complications shown that there were the patients with preoperative smoking cessation did not have an overall increased rate of postoperative complications. Moreover, it was significantly lower compared with the patients without preoperative smoking cessation (RR, 0.37; 95% CI, 0.26-0.52; P<0.01; Figure 2).
Rate of wound-related complications
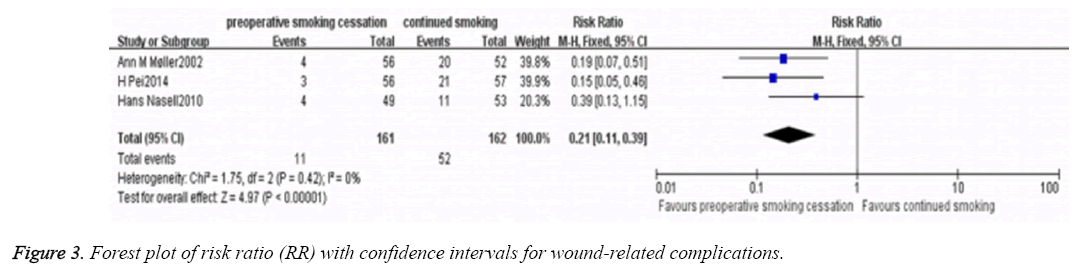
Meta-analysis of wound-related complications in three RCTs [3,9,10] was performed using a fixed-effects model (P=0.42; I2 =0%). The results showed that wound-related complications (including: haematoma, superficial infection, subfascial infection) of patients with smoking cessation was significantly lower compared with the patients without smoking cessation (RR, 0.21; 95% CI, 0.11-0.39; P<0.01; Figure 3).
Rate of secondary surgery
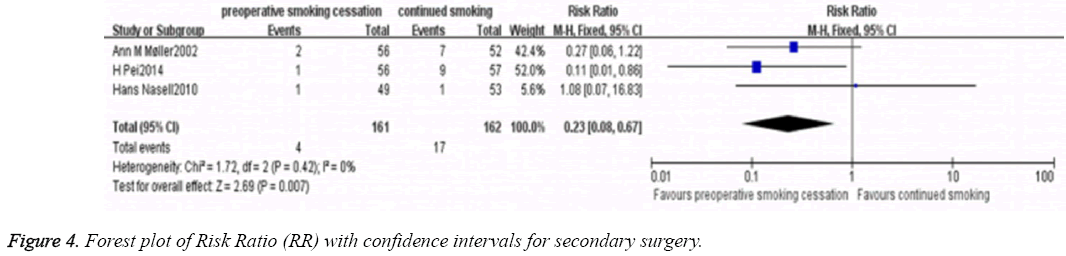
Meta-analysis of the secondary surgery rate of the three RCTs [3,9,10] was performed using a fixed-effects model (P=0.42; I2 =0%). The results showed that the smoking cessation significantly decreased the secondary surgery rate (RR=0.23; 95% CI, 0.08-0.67; P<0.01; Figure 4).
Rate of other postoperative complications
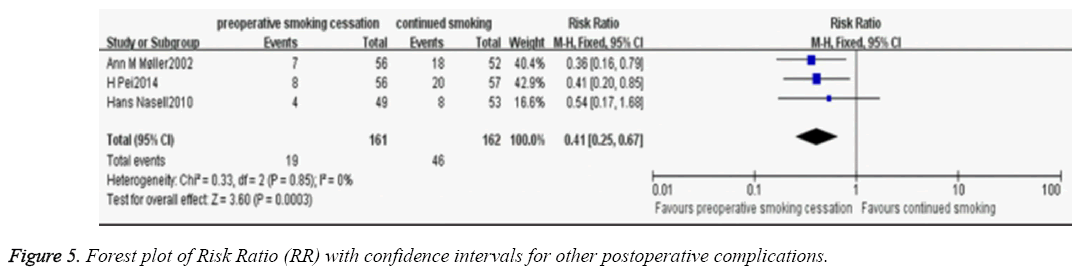
Meta-analysis of other postoperative complications rate of the three RCTs [3,9,10] was performed using a fixed-effects model (P=0.85; I2 =0%). The patients with preoperative smoking cessation had a lower incidence of other postoperative complications (including: respiratory insufficiency, cardiovascular insufficiency, renal insufficiency, gastrointestinal bleeding, deep venous thrombosis and pulmonary embolus) compared with the patients without smoking cessation (RR, 0.41; 95% CI, 0.25-0.67; P<0.01; Figure 5).
Rate of fracture non-union and osteomyelitis
The NRCCT [2] showed that the patients with preoperative smoking cessation had a lower incidence of fracture non-union than the patients without preoperative smoking cessation (RR=0.46; 95% CI, 0.23-0.93; P=0.03). In addition, the incidence of osteomyelitis was lower in the patients with preoperative smoking cessation compared with the patients without preoperative smoking cessation, although this difference was not statistically significant (RR=0.78; 95% CI, 0.39-1.56; P=0.49).
GRADE profile evidence
The included RCTs had same outcome indicators which were overall incidence of postoperative complications, rate of wound-related complications and rate of secondary surgery. In addition, the rate of fracture non-union was determined in NRCCT. Table 4 shows the outcome levels classified by GRADE system.
| Fracture non-union |
Overall incidence of postoperative complications |
Wound-related complications | Secondary surgery |
Other postoperative complications |
Osteomyelitis | |
|---|---|---|---|---|---|---|
| Studies design and no. of consisting studies | NRCCT/1 | RCT/3 | RCT/3 | RCT/3 | RCT/3 | NRCCT/1 |
| Risk of bias | Serious | Serious | Serious | Serious | Serious | Serious |
| Inconsistency | No serious inconsistency |
No serious inconsistency |
No serious inconsistency |
No serious inconsistency |
No serious inconsistency |
No serious inconsistency |
| Indirectness | No serious indirectness |
No serious indirectness |
No serious indirectness |
No serious indirectness |
No serious indirectness |
No serious indirectness |
| Imprecision | Serious | No serious imprecision |
No serious imprecision |
No serious imprecision |
No serious imprecision |
Serious |
| Other considerations | None | None | None | None | None | None |
| Preoperative smoking cessation | 9/82 (11%) | 32/161 (19.9%) | 11/161 (6.8%) | 4/161 (2.5%) | 19/161 (11.8%) | 11/82 (13.4%) |
| Continued Smoking | 25/105 (23.8%) CI (0.32 to 0.93) |
87/162 (53.7%) | 52/162 (32.1%) | 17/162 (10.5%) | 46/162 (28.4%) | 18/105 (17.1%) |
| Relative effect | RR 0.46 (from 17 fewer to 183 fewer) |
RR 0.37 CI (0.26 to 0.52) |
RR 0.21 CI (0.11 to 0.39) |
RR 0.23 CI (0.08 to 0.67) |
RR 0.41 CI (0.25 to 0.67) |
RR 0.78 CI (0.39 to 1.56) |
| Absolute effect | 129 fewer/1000(from 17 fewer to 183 fewer) |
1000 (from 258 fewer to 397 fewer) |
1000 (from 196 fewer to 286 fewer) |
81 fewer/1000 (from 35 fewer to 97 fewer) |
168 fewer/1000 (from 94 fewer to 213 fewer) |
1000 (from105 fewer to 96 fewer) |
| Quality | ⊕⊕○○ Low | ⊕⊕⊕○ Moderate | ⊕⊕⊕○ Moderate | ⊕⊕⊕○ Moderate | ⊕⊕⊕○ Moderate | ⊕⊕○○ Low |
| Importance | Critical | Critical | Important | Important | Important | Important |
Table 4: Grade profile evidence.
Discussion
Four studies were included in this systematic review, including three Randomized Controlled Clinical Trials (RCTs) and one Non-Randomized Concurrent Controlled Trial (NRCCT), involving a total of 510 patients. We have conducted the first systematic review and meta-analysis to evaluate the effect that smoking cessation is beneficial to the postoperative outcome of orthopaedic surgical patients. In our study, the results showed that in the patients with preoperative smoking cessation, the risk of overall postoperative complications was lower that the patients without preoperative smoking cessation. Furthermore, preoperative smoking cessation reduced the risk of woundrelated complications, recurrent surgery and additional complications. The NRCCT study demonstrated that the risks of fracture non-union and osteomyelitis in the patients with preoperative smoking cessation were reduced. These findings support the previously published reports on the benefits of smoking cessation prior to orthopaedic surgery [3,9,10]. It is also reported that smoking is associated with a significantly increased risk of aseptic loosening of prosthesis, deep infection and all-cause revisions after total hip arthroplasty [14]. However, these findings were in contrast to the results of Castilo et al. [2] who showed that the incidence of postoperative complications in patients who ceased smoking preoperatively were not reduced (RR=0.54, P>0.05) compared with the patients who continued to smoke.
Most previous studies that have shown the harmful effects of smoking were either epidemiological studies of patient populations or laboratory-based animal studies. Smoking studies using animal models have shown that nicotine and other components of cigarette smoke impede the healing of bone fractures by inhibiting the expression of genes for bone growth factors such as Bone Morphogenetic Proteins (BMPs), Transforming Growth-Factor beta (TGF-β) and Platelet- Derived Growth-Factor (PDGF) in a dose-dependent way [15-19]. In terms of clinical evaluation on the effects of smoking in orthopaedic patients undergoing surgery, as this study has shown, there has been little evidence-based, controlled clinical research.
The inconsistencies in the findings of the clinical literature have recently been highlighted by the systematic review and meta-analysis of data conducted by Scolaro et al. [5] nineteen clinical studies which showed that time to achieve union of fractures and the incidence of superficial and deep postoperative infections was not prolonged in smokers when compared with non-smokers. The reasons for the different results may be due to the variations in trial design and quality, including confounding factors of metabolic bone disease diseases, alcohol use, neurological and psychiatric medications use, for example.
Recent developments in orthopaedic surgical techniques have refined surgical procedures combined with new therapies, for example, the application of tissue-engineered bone in treating fracture non-union, and improvement of postoperative treatment, which reduced the incidence of fracture non-union and postoperative complications. The preoperative smoking cessation should be recommended to reduce morbidity and inhospital mortality following general surgery, vascular surgery, cardiothoracic surgery and, in our view, orthopaedic surgery.
The present study has provided further evidence that preoperative smoking cessation is beneficial to bone healing and may reduce the incidence of complications following orthopaedic surgery. However, according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system used in the study analysis, the quality of the evidence was only intermediate or low.
There were some limitations in this study. First, the number of published studies is small. There is a lack of allocation concealment and blinding in these studies. The imprecision of meta-analysis may be caused by un-conforming to the Optimal Information Size (OIS) standards. As a key indicator, the rate of fracture union was only performed in the non-randomized trial. Second, the way of recording cigarette consumption (per day/year) varies in these studies. There were also differences of periods of preoperative smoking cessation, surgical technique and the clinical outcomes among these studies.
Further prospective large-scale, multi-center, randomized controlled clinical trials are still needed to evaluate the relationship between smoking and outcome in orthopaedic surgery.
In conclusion, current evidence supported by this study indicates that for smokers who are planning to undergo orthopaedic surgery, preoperative smoking cessation does not increase the rate of fracture non-union, but can decrease the incidence of postoperative complications, reduce health care expenses and hospital stay.
Conflict of Interest
The authors declare no conflict of interests.
References
- Czernin J, Waldherr C. Cigarette smoking and coronary blood flow. Prog Cardiovasc Dis 2003; 45: 395-404.
- Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma 2005; 19: 151-157.
- Nasell H, Adami J, Samnegard E, Tonnesen H, Ponzer S. Effect of smoking cessation intervention on results of acute fracture surgery: a randomized controlled trial. J Bone Joint Surg Am 2010; 92: 1335-1342.
- Dube SR, Mcclave A, James C, Caraballo R, Kaufmann R. Vital signs: current cigarette smoking among adults aged>or=18 years-United States, 2009. Morbid Mortal Rep 2010; 60: 1135-1140.
- Scolaro JA, Schenker ML, Yannascoli S, Baldwin K, Mehta S. Cigarette smoking increases complications following fracture: a systematic review. J Bone Joint Surg Am 2014; 96: 674-681.
- Lindstrom D, Sadr Azodi O, Wladis A, Tonnesen H, Linder S. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 2008; 248: 739-745.
- Lee SM, Landry J, Jones PM, Buhrmann O, Morley-Forster P. The effectiveness of a perioperative smoking cessation program: a randomized clinical trial. Anest Analg 2013; 117: 605-613.
- Wong J, Lam DP, Abrishami A, Chan MT, Chung F. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Canadian JAnesth 2012; 59: 268-279.
- Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002; 359: 114-117.
- Pei H, Zhang L, Zeng L. Effect of preoperative smoking intervention on postoperative complications of total hip replacement. Chinese J Evid Med 2014; 14: 399-403.
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003; 73: 712-716.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336: 924-926.
- Krannitz KW, Fong HW, Fallat LM, Kish J. The effect of cigarette smoking on radiographic bone healing after elective foot surgery. J Foot Ankle Surg 2009; 48: 525-527.
- Teng S, Yi C, Krettek C, Jagodzinski M. Smoking and risk of prosthesis-related complications after total hip arthroplasty: a meta-analysis of cohort studies. PLoS One 2015; 10: e0125294.
- Ma L, Zwahlen RA, Zheng LW, Sham MH. Influence of nicotine on the biological activity of rabbit osteoblasts. Clin Oral Implan Res 2011; 22: 338-342.
- Morimoto N, Takemoto S, Kawazoe T, Suzuki S. Nicotine at a low concentration promotes wound healing. J Surg Res 2008; 145: 199-204.
- Raikin SM, Landsman JC, Alexander VA, Froimson MI, Plaxton NA. Effect of nicotine on the rate and strength of long bone fracture healing. Clin Orthop Res 1998; 353: 231-237.
- Skott M, Andreassen TT, Ulrich-Vinther M, Chen X, Keyler DE. Tobacco extract but not nicotine impairs the mechanical strength of fracture healing in rats. J Orthop Res 2006; 24: 1472-1479.
- Wong LS, Green HM, Feugate JE, Yadav M, Nothnagel EA, Martins-Green M. Effects of second-hand smoke on structure and function of fibroblasts, cells that are critical for tissue repair and remodeling. BMC Cell Biol 2004; 5: 13.