ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2011) Volume 22, Issue 4
The inflammatory markers: C-Reactive Protein and TNF-? predict Cardiovascular risks in obese North Indian subjects
Department of Medicine, JNMCH, Aligarh Muslim University, Aligarh, India
- Corresponding Author:
- S .F. Haque
Department of Medicine
Aligarh Muslim University
Aligarh-202002, India
E-mail: sfhalig@yahoo.co.in
Accepted Date: July 24 2011
Obesity is associated with a low-grade inflammation of white adipose tissue (WAT) resulting from chronic activation of proinflammatory molecules: C-reactive Protein(CRP), TNF-alpha and interleukin-6 (IL-6).These cytokines subsequently lead to insulin resistance, im-paired glucose tolerance and even diabetes. This is a cross-sectional, open label, compara-tive, observational study, in a North Indian population cohort. Thirty cases of obesity were evaluated, against twenty normal weight regarding metabolic and inflammatory markers in relation to cardiovascular risk factors. All patients underwent detailed clinical and bio-chemical, CRP and TNF-α estimation at baseline and at the end of the study period. The dif-ferences between the percentage changes in each parameter in the two groups was com-pared by applying the unpaired t-test using the SPSS 10.0 software. Comparison showed significant difference in CRP and TNF-α between normal weight individuals (BMI<30) and obese individuals (BMI>30) at a p value <0.001. Similarly comparison of total cholesterol, LDL-cholesterol, HDL-cholesterol and Triglyceride levels, showed significant difference be-tween normal weight individuals (BMI<30) and obese individuals (BMI>30) at a p value <0.05. Inflammatory markers like TNF-α and CRP levels were elevated in obese subjects, reinforcing the view that obesity is in part an inflammatory disorder. Further there was evi-dence of worsening dyslipidemia with BMI and cardiovascular risks The study also sug-gested that inflammatory marker TNF-α is correlated with cardiovascular risk factors in obesity, rather than just being a manifestation of the inflammatory state.
Keywords
Obesity, inflammation, C-reactive protein, interleukin-6, LDH cholesterol
Introduction
Obesity is a risk factor for atherogenic dyslipidemia, insulin resistance, and hypertension. Overweight and obesity are the fifth leading risk for deaths worldwide. At least 2.8 million adults die each year as a result of being obese. In addition, 44% of the diabetes burden, 23% of the is-chaemic heart disease burden and between 7% and 41% of certain cancer burdens are attributable to overweight and obesity.Obesity is defined by WHO as a Body Mass Index (BMI) of >30 kg/m2[1,2]. The distribution of body fat is an important predictor of obesity-associated, morbidity and it has been clearly shown that upper body visceral fat accumulation is related to insulin resistance [3]. The visceral fat, is considered to be the most ‘atherogenic, diabetogenic and hypertensiogenic’ fat depot of the human body[4] .Visceral fat excess has been associated with decreased sensitivity of insulin mediated glucose uptake and reduced rate of FFA re-esterification [5]. It is estimated that a waist circumference in men of >102 cm and in women of > 88 cm carried the same risk of developing cardiovascular risk as a BMI of 30. It now appears that, in most obese patients, obesity is associated with a low-grade inflammation of white adipose tissue (WAT) ,characterized by an increased production and secretion of a wide range of inflammatory molecules including TNF-alpha and interleukin-6 (IL-6), which may have local effects on WAT physiology but also systemic effects on other organs. Researchers have found that plasma levels of CRP, TNFα and IL-6: markers of inflammation are elevated in subjects with obesity [6].
Higher adipose tissue content of IL-6 has been associated with higher serum CRP levels in obese subjects.[7] .TNF-α plays a role in insulin resistance and T2DM[8]. Plasma TNFα level is negatively correlated with HDL-cholesterol, HbA1C and serum insulin concentration. Therefore in otherwise healthy but overweight and obese subjects, elevated plasma/serum concentration of CRP, IL-6 & TNF-α levels are observed, this led to the concept of the ‘adipo-vascular axis’ which is thought to, contribute to the, increase in cardiovascular events in obese subjects[10]. The Asian Indian has a unique phenotype characterized by increased abdominal obesity and visceral fat despite low body mass index. This was attributed to increased visceral fat [11]. TNF-α correlates with hyperinsulinemia in obesity, a link that is reversed with weight reduction. The effects of TNF- α are manifold: Modulation of lipid metabolism, decrease in tyrosine kinase activity, down regulation of glucose transporter proteins and pancreatic β-cell dysfunction.
The studies correlating inflammatory markers with cardiovascular risks are scarce especially in north Indian population. The present study was undertaken to evaluate inflammatory markers CRP and TNF-α and cardiovascu-lar risks in a North Indian cohort of obese subjects.
Materials and Methods
This prospective, observational study was carried out on obese patients attending the outpatient and admitted in the wards in the Department of Medicine, between January 2006 and July 2007. The study was approved by Institutional ethics committee.
Study Subjects
Study group patients were labeled as obese who had presented with a body mass index (BMI) > 30. Informed consent was taken from each subject. Out of the total 50 subjects taken in this study, 30 comprised the study group. The control group comprised of 20 age and sex matched healthy normal weight volunteers. Detailed history and physical examination was carried out at the recruitment of the patients.
Cardiovascular risk factors taken into consideration for the study were as follows
1. Hypertension – as per the JNC 7 Criteria
2. Family history of premature coronary artery disease.
3. Dyslipidemia
4. Smoking
Exclusion Criteria
Patients with acute infectious states, acute coronary syndrome, renal failure, on steroids, critically ill, septicemic, and moribund and diabetics were excluded from study.
The baseline parameters measured in the study were as follows:
1. Body mass index
2. Levels of CRP and TNF-α
3. Lipid profile: total cholesterol, low density cholesterol, high density cholesterol, triglyceride levels.
The values of various parameters were recorded at the initiation and completion of the study at.
Statistical analysis
The differences between the percentage changes in each parameter in the two groups were compared by applying the unpaired t-test using the SPSS 10.0 software.
Results
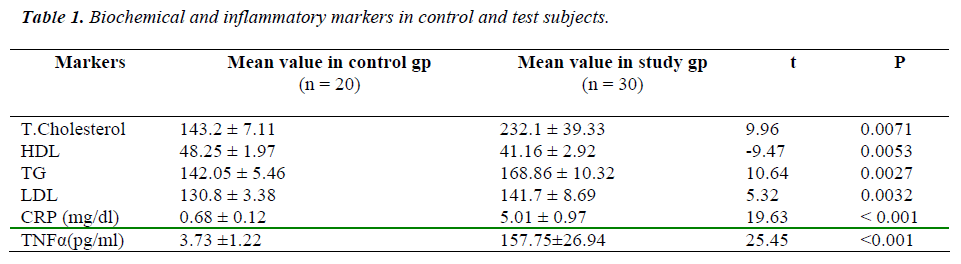
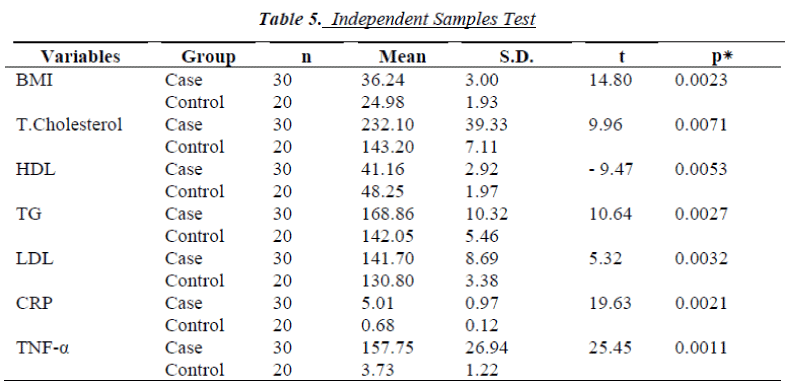
Comparison of CRP and TNF-α levels among the study and control groups using the t test for independent samples, showed significant difference between normal weight individuals (BMI<30) and obese individuals (BMI>30) at a p value <0.001. Similarly comparison of total cholesterol, LDL-cholesterol, HDL-cholesterol and Triglyceride levels among the two groups, showed significant difference in their levels between normal weight individuals (BMI<30) and obese individuals (BMI>30) at a p value <0.05, as depicted in table 1.
Pearson’s correlation coefficient showed a significant association of CRP with Body Mass Index (BMI), LDL-cholesterol and TNF-α level in the study group. The p values for other variables were not significant, as shown in table 2.
Similarly Pearson’s correlation coefficient showed a significant association of TNF-α with Body Mass Index (BMI), Triglycerides, and LDL-cholesterol and CRP levels in the study group. The p values for other variables were not significant, as shown in table 3.
Pearson’s correlation coefficient showed a significant association of Body Mass Index (BMI) with LDL-cholesterol, TNF-α and CRP levels in the study group, thus indicating that with increasing body weight and worsening dyslipidemia, CRP and TNF-α values rise. The p values for other variables were not significant, as shown in table 4.
Discussion
In recent years an association between obesity, cardiovascular events and inflammation has been reported and now appears well established. Recent studies have shown inflammation plays an important role in the pathogenesis of obesity and cardiovascular disease [12,13]. In acute inflammatory conditions, cytokines initiate and coordinate the inflammatory response that includes increasing the hepatic production of acute phase reactants, including C-reactive protein [14]. Plasma levels of CRP in the absence of active diseases are low, but can increase up to 1000 fold in patients with inflammatory reaction. Besides being a marker of inflammation, CRP itself may have pro-inflammatory properties since it can activate the complement system [15]
In our study, the number of cardiovascular risk factors like hypertension, family history of coronary artery disease and smoking was found to differ significantly between normal weight and over weight individuals. Similar results have been obtained in previous studies which have reported a progressive increase in the incidence of chronic diseases such as hypertension, diabetes, and coronary heart disease with increasing body mass index [16, 17,18].
The data generated in our study are strongly indicative of the appreciable correlation between obesity and dyslipidemia, with a direct relationship between LDL-Cholesterol and Triglyceride levels and inverse relation between HDL-Cholesterol and obesity and cardiovascular risks.
C-reactive protein levels were consistently found to be elevated over the increasing grades of obesity in our study. Besides, our study also showed a significant association between cardiovascular risk factors and the likeli-hood of having elevated CRP in multivariate regression models. This is consistent with the recent view that obesity is in part an inflammatory disorder and CRP is one of the strongest markers of metabolic risk and, in addition, may participate directly in the arterial cell wall mechanisms leading to atherosclerotic lesions and cardiac events [19,20,21]
There is growing recognition that coronary heart disease (CHD) has an inflammatory component [22,23] Prospective studies have shown that plasma CRP concentration, a marker of the acute-phase reaction, can predict CHD events in subjects with [24,25] established cardiovascular disease beyond what can be estimated by traditional risk factors.
Pearson’s correlation coefficient showed a significant association of CRP with Body Mass Index (BMI), LDL-cholesterol and TNF-α level in the study group. The p values for other variables were not significant.
Till date various studies have shown that in the basal state TNF-α is directly proportional to fat mass and has been shown to be involved in the development of insulin resistance [26,27]. Within adipose tissue, macrophages ac-count for nearly all TNF-α production, and both TNF-α mRNA content and TNF-α production increase in adipose tissue of obese individuals [28,29]. Circulating TNF-α concentration, in turn, also rises with increasing obesity and correlates with insulin resistance [30].
More data have now accumulated to reinforce the concept that obesity is an inflammatory state [31,32].Human plasma concentrations of TNF-α, IL-6, CRP and other inflammatory mediators have been shown to be increased in the obese subjects [33,34].The most striking finding in our study was the significant difference in TNF-α levels between normal weight individuals (BMI<30) and obese individuals (BMI>30) at a p value <0.001. Also, Pearson’s correlation coefficient showed a significant association of TNF-α with Body Mass Index (BMI), Triglycerides, LDL-cholesterol and CRP levels in the study group. The p values for other variables were not significant.
TNF-α level were also shown to be significantly associated with cardiovascular risk factors and were an important predictor of cardiovascular risks over the increasing range of body mass index, in the logistic regression model.
Pearson’s correlation coefficient showed a significant association of Body Mass Index (BMI) with LDL-cholesterol, TNF-α and CRP levels in the study group, thus indicating that with increasing body weight and worsening dyslipidemia, CRP and TNF-α values rise. The strength of linear association between Body Mass Index and other clinical and biochemical parameters was assessed using Pearson’s correlation. Significant association was noted with LDL-cholesterol, CRP and TNF-α, with varying levels of significance.
When Total cholesterol, LDL-cholesterol, HDL-cholesterol and Triglyceride levels were compared among the study and control groups using the t test for independent samples, significant difference was noted in their levels between normal weight individuals (BMI<30) and obese individuals (BMI>30) at a p value <0.05.
TNF-α levels were extensively analyzed in our study with respect to its association with Body Mass Index, cardiovascular risk factors and the lipid profile. This was further strengthened by the presence of strong correlation between TNF-α levels and BMI using Pearson’s correlation with a p value < 0.001. The other important predictors of TNF-α level as per Pearson’s correlation were Triglycerides, LDL-cholesterol and CRP values.
Inflammatory and metabolic markers were extensively analyzed in our study with respect to their association with increasing body weight and cardiovascular risk factors. This is a small sized yet relevant study highlighting inflammation as intrinsic component of obesity and its cardiovascular complications.
Conclusion
We conclude from our study that there is a strong association between body mass index (BMI), dyslipidemia and cardiovascular risk factors and there is evidence of worsening dyslipidemia with increasing body weight and cardiovascular risks. Furthermore inflammatory markers like TNF-α and CRP levels are elevated in obesity, reinforcing the view that obesity is in part an inflammatory disorder. The study also suggested that inflammatory marker TNF-α is correlated with cardiovascular risk factors in obesity, rather than just being a manifestation of the inflammatory state. Thus cardiovascular risk is an important association with obesity, the severity being determined by body mass index, LDL-Cholesterol, Triglycerides, HDL-cholesterol, CRP and TNF-α level independently. Our study was an attempt to extensively analyze the inflammatory and metabolic markers with respect to their association with increasing body weight and cardiovascular risk factors, and to use these markers to help to identify individuals at higher risk for cardiovascular events despite not meeting criteria based on lipid profile or other traditional risk factors alone. Further large scale multi centre studies with different anthropological parameters are needed to consolidate these preliminary results in a large population.
References
- World Health Organization. WHO report EURICP= Nut 125. Copenhagen, Denmark: World Health Organization; 1987. Measuring Obesity Classification and description of anthropometric data Report on a WHO Consultation on the Epidemiology of Obesity.
- World Health Organization. MONICA Manual. Ge-neva, Switzerland: World Health Organization; 1990.
- Barzilai N, Gupta G: Revisiting the Role of Fat Mass in the Life Extension Induced by Caloric Restriction. J Gerontol 1999;54A: B89-B96,
- Despres JP. Is visceral obesity the cause of the metabolic syndrome? Ann.Med.2006; 38: 52-63
- Gerich JE.Contributions of insulin resistance and insulin secretory defects to the pathogenesis of type 2 diabetes mellitus, Mayo Clinic proceedings, 2003; 78; 447-456
- Burke AP, Tracy RP, Kolodgie F, Malcom GT, Zieske A, Kutys R, Elevated C-reactive protein values and atherosclerosis in sudden coronary death: Association with different pathologies. Circulation 2002; 105: 2019-2023.
- Dandona P, Weinstock R, Thusu K, Abdel-Rahman E, Aljada A, Wadden T. Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metab 1998; 83:2907-2910.
- Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spie gelman BM Increased adipose expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest 1999;95: 2409-2415,
- Howard BV, Ruotolo G, Robbins DC. Obesity and dyslipidemia. Endocrinal Metab Clin N Am 2003;32: 855- 867,
- Engeli S, Feldpausch M, Gorzelniak K, Hartwig F, Heintze U, Janke J, Mohlig M, Pfeiffer AF, Luft FC, Sharma AM: Association between adiponectin and mediators of inflammation in obese women. Diabetes 2003; 52: 942-947.
- Raji A, Ellen W. Seely, Ronald A. Arky, Donald C. Simonson, Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians J Clin Endocrinol Metab 2001; 86: 5366-5371.
- Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol 2001;280: E745-E751
- Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997; 336: 973-979.
- Steel DM, Whitehead AS: The major acute phase reactants: C-reactive protein, serum amyloid P component and serum amyloid A protein. Immunol Today 1994; 15: 81-88.
- Wolbink GJ, Brouwer MC, Buysmann S, Ten Berge IJ, Hack CE: CRP mediated activation of complement in vivo: assessment by measuring circulating complement C-reactive complexes. J Immunol 1996;157: 473-479
- W, Sund M, Fröhlich M, Fischer HG, Lowel H, Doring A, et al. C-Reactive protein, a sensitive marker of in flammation, predicts future risk of coronary heart dis ease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation 1999; 99: 237-242.
- Kuller LH, Tracy RP, Shaten J, Meilahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol 1996;144: 537-547,
- Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Re-buzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med 1994;331: 417-424.
- Liuzzo G, Biasucci LM, Lanza GA, et al. C-reactive proteins increased in unstable angina but not in active variant angina. Is inflammation in acute coronary syndromes related to ischaemia ?. Circulation 1994; 90: 3576.
- Munro JM, Cotran RS. The pathogenesis of atherosclerosis: atherogenesis and inflammation. Lab Invest 1988; 58: 249-261,.
- Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA 2001; 286: 327- 334,
- Thompson SG, Kienast J, Pyke SD, Haverkate F, van de Loo JC. Hemostatic factors and the risk of myocardial infarction or sudden death in patients with angina pec toris: European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. N Engl J Med 1995; 332: 635-641.
- Torzewski J,. C-reactive protein frequently colocalizes with the terminal complement complex in the intima of early atherosclerotic lesions of human coronary arteries. Arteriosclero Thromb Vasc Biol 1998; 18: 1386-1392
- Kluft C, de Maat MP. Determination of the habitual low blood level of C- reactive protein in individuals. Ital. Heart J. 2001; 2:172-180
- de Maat M P, Kluft C The association between inflammation markers, coronary artery disease and smoking. Vascular Pharmacology 2002; 39: 137-139
- Hotamisligil, G.S., Shargill NS, Spiegelman, BM Inflammatory Pathways and Insulin Action, Int J Obes Relat Metab Disord, 1993; 259: 87-91
- Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab. 2001; 280 (5): E745-51
- Tsigos C, Kyrou I, Chala E, Tsapagos P, Stavridis JC, Raptis SA, Katsilambros N: Circulating tumor necrosis factor alpha concentrations are higher in abdominal versus peripheral obesity. Metabolism 1999; 48: 1332-1335.
- Vozarova B, Weyer C, Hanson K, Tataranni PA, Bo-gardus C, Pratley RE. Circulating interleukin-6 in relation to adiposity, insulin action, and insulin secretion. Obes Res 2001; 9: 414-417..
- Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men .N Engl J Med 1996;336: 973-979.
- Tracy RP, Lemaitre RN, Psaty BM, Ives DG, Evans RW, Cushman M, Meilahn EN, Kuller LH. Relationship of C-reactive protein to risk of cardiovascular disease in the elderly: results from the Cardiovascular Health Study and the Rural Health Promotion Project. Arterioscler Thromb Vasc Biol 1997;17: 1121-1127.
- Tracy RP, Psaty BM, Macy E, Bovill EG, Cushman M, Cornell ES, Kuller LH. Lifetime smoking exposure affects the association of C-reactive protein with cardiovascular disease risk factors and subclinical disease in healthy elderly subjects. Arterioscler Thromb Vasc Biol 1997; 17: 2167-2176
- Wakabayashi I. Age-related change in relationship be-tween body-mass index, serum sialic acid, and atherogenic risk factors. J Atheroscler Thromb 1998.;5:60-65
- WHO Consultation on Obesity. Preventing and managing the global epidemic. Geneva: World Health Organization 1997; pp. 1-276.