ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2012) Volume 23, Issue 1
The prevalence of ? Thalassemia in South Western Maharashtra
Department of Biochemistry, Government Medical College, Miraj, Maharashtra, India
- *Corresponding Author:
- Abdulrahaman A Momin
Department of Biochemistry
MVP’s Dr. Vasantrao Pawar Medical College
Adgaon, Nashik 3, Maharashtra
India
Accepted date: August 09 2011
The early identification of some clinically significant hemoglobinopathies and precise differentiation of hemoglobin variants are important to provide early comprehensive medical care to prevent some serious complications, assess prognosis and offer genetic counseling. A prospective study of 500 infants from South Western Maharashtra showed that 0.4% (4 in 1000) of them had detectable levels of Hb Bart’s (γ4) in the neonatal period by using hemoglobin electrophoresis. The levels of Hb Bart’s indicate that the newborns are heterozygous for α thalassemia (-α/αα).
Keywords
α Thalassemia, hemoglobinopathies, Hb Bart’s, hemoglobin electrophoresis.
Introduction
The thalassemias are heterogeneous group of disorders of hemoglobin synthesis resulting from the reduced rate of synthesis of one or more globin chains of hemoglobin. Decreased synthesis of α chain produces α thalassemia, while decreased synthesis of β chains produce β thalassemia. The thalassemias are among the most common genetic disorders worldwide, occurring more frequently in Mediterranean region, the Indian subcontinent, Southern Asia, and West Africa. [1]
The result of such unbalanced globin chain synthesis is the production of an excess of partner chains which are synthesized at normal rate, and most of the clinical features of the thalassemias can be related to the deleterious effects on erythropoiesis, caused by precipitation of the goblin chains that are produced in excess. [2,3]
If there is a reduced output of α chains, any excess of γ chains or β chains produced will give rise to molecules with the formula γ4 (Hb Bart’s) and β4 (Hb H), respectively. Hence the α thalassemias are usually associated with the presence of Hb Bart’s in infancy and Hb H in adult life.[4] We conducted a study to investigate the prevalence of α thalassemia in the South Western Maharashtra (India), because, there is no published report on prevalence of α thalassemia in this area
Materials and Methods
This is a cross sectional study to find out the prevalence of α thalassemia from south western Maharashtra region. Blood samples were collected randomly from successive infants from the Obstetrics department of the General Hospital, Sangli and Government Medical College & Hospital, Miraj and were analyzed at department of biochemistry. The written informed consent of mother was taken.
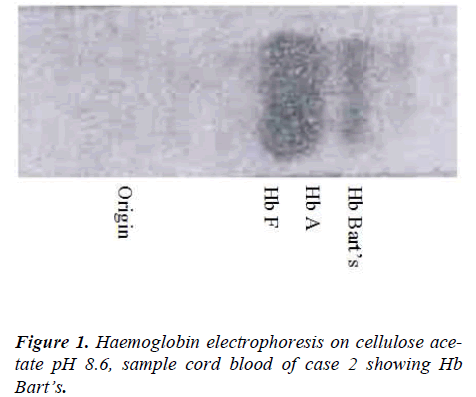
Electrophoretic analysis was done on cellulose acetate membranes using Tris-EDTA-Borate buffer at pH 8.6. Cellulose acetate membranes were stained with Ponceau S then made clear by using methanol and acetic acid mixture in a proportion of 7:3 respectively, [5,6] and the results were read by using densitometer.
Results
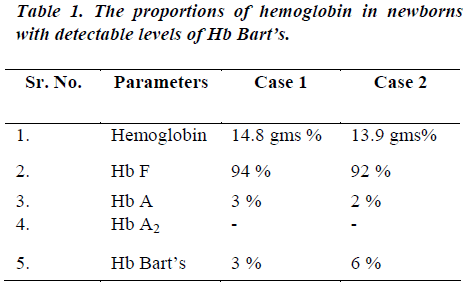
Our study included 500 newborns, all were normal at birth. Out of 500 cord blood samples examined 498 had no Hb Bart’s. Electrophoretic pattern of only 2 samples showed a fast migrating component. This band occupied a position taken up by Hb Bart’s. Analysis of samples showed that Hb Bart’s level was 3% of total Hb in 1st case and 6% of total Hb in 2nd case. 1st case showed Hb F level of 94% of and Hb A level of 3% while 2nd case showed 92% and 2% respectively.
The total hemoglobin content in these two samples was 14.8 gms/dL and 13.9 gms/dL respectively. The levels of Hb Bart’s in these cases were suggestive of heterozygous α thalassemia with single gene deletion (-α/αα). The incidence of α thalassemia in South Western Maharashtra is 0.4% (i.e. 4 in 1000).
No cases of homozygous α thalassemia or hydrops fetalis (--/--) were detected in sample size studied. The results are summarized in the following Table 1.
Discussion
Hb Bart’s is a tetramer of γ chains (γ4). Most reports on incidence of alpha thalassemia among Indians are based on demonstration of Hb Bart’s in cord blood samples. [4] It is generally accepted that Hb Bart’s is formed because of defective synthesis of α chains. As a result there is relative excess production of γ chains. These polymerize to form γ4 tetramers, which are often associated with abnormal red cell morphology and hemolytic anemia. [3]
Hb Bart’s usually disappears by the age of four to six months but might persist beyond the first year of life after which a tetramer of β chains or Hb H makes its appearance. This happens because the rate of synthesis of γ chains rapidly declines with an increase in production of β chains. [7] A study by Fessas P. [8] showed 1-1.5% Hb Bart’s may be present in normal cord bloods, however according to Wasi P. [9] Hb Bart’s of 1-2 % in cord blood is indicative of α thalassemia trait.
The heterozygous α thalassemia diagnosed by the increased level of Hb Bart’s in cord blood, has been found in a number of racial and ethnic groups throughout the world. The prevalence of α thalassemia in India varies from one sub-geographical area to another. The prevalence is 71% in Behrampur, 42% in Jaipur and 11% in the nearby villages of Andhra Pradesh. [10]
Our study gives the incidence of α thalassemia 0.4% or 4 per thousand populations in South Western Maharashtra.
In a similar study, Misra R. C. [11] showed 7 cases of α thalassemia out of 91 cord blood samples analyzed. The amount of Hb Bart’s was approximately 5-10 % in 6 samples and upto 2% in one sample. In the study done by Dash S., [12] 54 cases of α thalassemia with Hb Bart’s were found out of 300 samples.
In a study, Misra R. C. [13] had showed the prevalence of 12.6 % and Mitra S. S. [14] noted the presence of Hb Bart’s in 4 % of cord bloods of Bengali newborns. Sankar V. [15] found 32 cases of α thalassemia out of 276 patients of microcytic hypochromic anemia, 30 patients of which had heterozygousα3.7 deletion (-α/αα) and two patients had homozygous α3.7 (-α/-α) deletion.
Conclusion
500 cord blood samples were investigated for presence of Hb Bart’s by using cellulose acetate hemoglobin electrophoresis at an alkaline pH. Out of 500 only 2 samples revealed a fast migration Hb Bart’s. The levels of Hb Bart’s were 3% and 6% which were an indication of cases of heterozygous α thalassemia or silent carrier state, thus giving the prevalence of 0.04% in South Western Maharashtra.
References
- Wood WG. Hemoglobin synthesis during human fetal development. Br Med Bull, 1976; 32 (3): 282-287.
- Bertil E. G., Kelly A. L.: Hematological disorders in children from Southest Asia. Pediat Clin N Amer, 1996; 43 (3): 665-681.
- Giardina PJ, Forget BG. Thalassemia syndromes. In: Hoffman R., Benz E.J. Jr., Shattil S.J., Furie, L.E. Sil- berstein, McGlave P, Heslop H. Hematology: Basic Principles and Practice. 5th edn, Churchill Livingstone, Philadelphia, 2009; pp. 535-563.
- Lehmann H. Different types of alpha thalassemia and significance of hemoglobin Bart’s in neonates. Lancet, 1970; 11: 78-80.
- Fairbanks VF, Klee GG. Method for the separation of hemoglobins by alkaline electrophoresis. In: Biochemical aspects of hematology: Tietz textbook of Clinical Chemistry. 3rd edn, W. B. Saunders Co., 1999, pp 1679- 1682.
- Briere RO, Golias T, Batsakis JG. Rapid qualitative and quantitative hemoglobin fractionation: Cellulose acetate electrophoresis. Am J Clin Pathol, 1965; 44:695-701.
- Vora S, IyerP. D, Bhagat MP, Patel JC, Mehta BC. Incidence of hemoglobin Bart’s in cord blood samples. Indian J Med Sci, 1975; 29 (8-9): 205-207.
- Fessas P: Hemoglobin “Bart’s”. Brit Med J, 1959; 2: 886.
- Wasi P. Is the human α chain locus duplicated? Brit J Hemat, 1973; 24: 267.
- Balgir RS. The burden of hemoglonopathies in India and challenges ahead. Curr Sci, 2000; 79(11):1536- 1547.
- Misra RC. Detection of alpha thalassemia in sickle cell trait patients by Hb Bart’s screening and quantitaion of Hb A and Hb S. Ind J Med Res, 1989; 90: 459-462.
- Dash S, Vashist K, Sehgal S, Devi S, Verma A. Iso- electric focusing for measurement of hemoglobin Bart’s level in cord blood and detection of alpha thalas- semia. Ind J Med Res, 1988; 87: 62-66.
- Misra RC, Ram B, Mohapatra BC, Das SN, Misra S. C. High prevalence & heterogenicity of thalassemias in Orissa. Indian J Med Res, 1991; 94: 391-394.
- Mitra SS. The clinical and hematological profile of thalassemia and hemoglobinopathies in India. Ind Pe- diat, 1983; 20: 701-713.
- Sankar VH, Arya V, Tiwari D. Genotyping of alpha thalassemia in microcytic hypochromic anemia patients from North India. J Appl Genet, 2006; 47 (4):391-395.