ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2013) Volume 24, Issue 1
The prevalence of MRSA infection in orthopaedic surgery in a Medical College Hospital: A 2-year analysis.
S Nijalingappa Medical College and HSK Hospital, Navanagar, Bagalkot, Karnataka, India
- *Corresponding Author:
- Shiddanna M Patted
Department of Orthopaedics
S Nijalingappa Medical College and HSK Hospital and Research Centre
Navanagar, Bagalkot 587102
Karnataka, India.
Accepted Date: October 18 2012
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) infection is increasing world-wide. Vancomycin is one of the drug of choice for MRSA infection. The resistance to vancomycin in Staph. aureus, which was once thought to be very less, is also on a rise.So the present study aimed to find out the prevalence rate of MRSA infection and vancomycin resistance in patients admitted to orthopaedic wards. We analysed the data of patients admitted for orthopaedic care in a medical college hospital requiring bacterial culture-sensitivity study for either a suspected or an obvious infection between September 2007 and August 2009 in a retrospective observational study. The specimens were collected by either sterile cotton swab stick, an aspirate or the tissue obtained at surgery. The specimens were studied as per the standard protocol of the institute to note the organism grown and sensitivity to antibiotics. There were 1207 admissions to orthopaedic wards between September 2007 and August 2009.A total of 131 specimens collected from 115 patients were studied, yielding 81growths. Staph. aureus was isolated in 38 specimens of which 24(63%) were MRSA and 6(25%) of these MRSA were resistant to vancomycin. The prevalence of MRSA infection was 1.99 % ( 24/1207) and that of vancomycin resistant Staph. aureus infection was 1.07% (13/1207) of total orthopaedic admissions. The prevalence rate of MRSA infection and development of resistance to vancomycin is alarmingly high. There is need for increased awareness regarding incidence, pathogenicity, preventive and treatment measures of MRSA.
Keywords
MRSA, Infection, Orthopaedic surgery.
Introduction
Nearly half of the entire surgical site infectionsirrespective of the speciality- are caused by staphylococci, of which 81% are Staph. aureus, of these, 63% are resistant to methicillin [1]. The incidence of methicillinresistant Staphylococcus aureus (MRSA) infection is increasing [2]. The incidence of MRSA varies from region to region, and depends to great extent on the policy for infection control [3,4]. The rate of methicillin resistance is higher in orthopaedic units compared to other medical specialities [5]. MRSA produces biofilm and becomes more resistant to antibiotics [6]. When caused by MRSA either because of resistance to antibiotic or biofilm formation, the treatment of orthopaedic infection becomes complicated and poses a higher economic burden [7].
Vancomycin has been the cornerstone of treatment of MRSA infection [1]. It is considered that resistance to vancomycin is rare.
Our aim in this retrospective study was to find out the prevalence of MRSA infection and the rate of vancomycin resistance in patients admitted to the orthopaedic wards.
Materials and Methods
We analysed the data pertaining to patients admitted to orthopaedic wards of HSK hospital a tertiary care centre attached to SN medical college, Bagalkot, catering to rural and urban population of about 100 km radius , between September 2007 and August 2009 in a retrospective observational study. The clearance was obtained from the institutional ethical clearance committee before collecting the data. The patients who required a bacterial culture-sensitivity study for either a suspected or an obvious infection of musculoskeletal system were included in the study. The patients in whom a musculoskeletal system was not suspected or obviously infected though admitted to orthopaedic wards were excluded. The asymptomatic carrier state was not investigated. The specimens were collected by either a sterile cotton swab stick in a test tube, an aspirate in sterile syringe or the tissue collected at surgery with aseptic precautions. All the specimens thus collected were studied as per standard protocol of the institute to note the organism grown and sensitivity to antibiotics.
Results
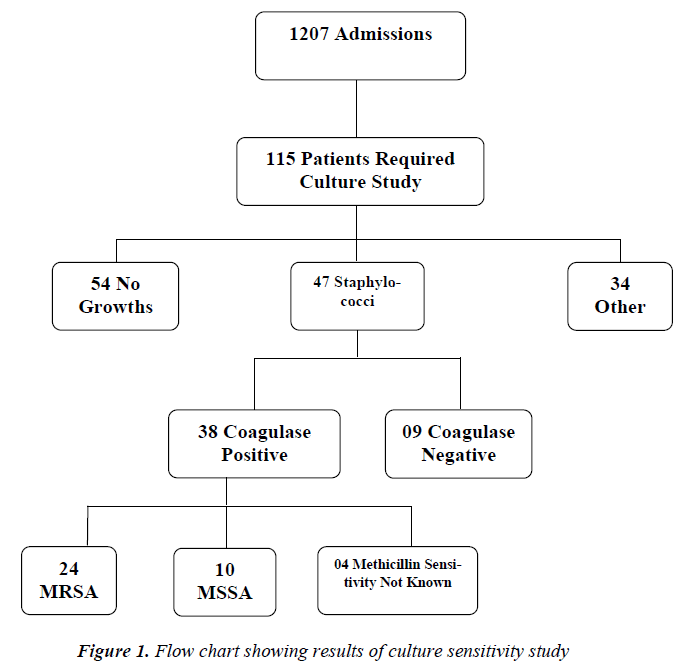
There were 1207 admissions to orthopaedic wards between September 2007 and August 2009[Figure1]. A total of 131 specimens collected from 115 patients were studied of which 92 were males and 23 were females. There was no growth in 54 specimens, single organism was grown in 73 specimens and 2 organisms were grown in 4 specimens making a total of 81 growths. There were 47 Staphylococci, of which 38 were coagulase positive (Staph. aureus). Among these 38 Staph. aureus growths 24(63%) were resistant to methicillin, 10 were sensitive to methicillin and in 4 patients the methicillin sensitivity was not known. Among these 38 Staph. aureus growths 13(34%) were resistant to vancomycin, 19 were sensitive, 1 was intermediate sensitive and in 5 the status was not known. Of the 24 MRSA growths 6(25%) were resistant to vancomycin also.
The prevalence of MRSA infection was 1.99 %( 24/1207) and prevalence of vancomycin -resistant Staph. aureus infection was 1.07 %( 13/1207) of total orthopaedic admissions.
The prevalence rate of MRSA infection was higher in female patients 30.4 %( 7/23) compared to male patients 18.4 %( 17/92) of the orthopaedic patients requiring bacterial culture studies.
Discussion
We have found that 1.99% of the patients admitted to orthopaedic wards were infected with MRSA during the study period. Roche et al reported a 0.29% of patients admitted to orthopaedic department had a confirmed MRSA infection of which 15% had infection at the time of admission in an Irish orthopaedic centre [7]. The high rate of MRSA infection in this study may be explained by the fact that nearly 67% (16/24) were infected with MRSA at the time of admission. Of these 16 patients who had MRSA infection at the time of admission 10 were either hematogenous osteomyelitis or septic arthritis, 6 were related to trauma. Of the 8 patients who developed MRSA infection in the hospital, 6 were open fractures and 2 were closed fractures.
The prevalence rate of Vancomycin resistant Staph. aureus infection was 1.07%. With a fourth of MRSA growths being resistant to vancomycin too, the antibiotic use policy against MRSA may require a revision.
There was no growth in 54 of the 131 specimens studied. This could be because of four reasons, 1.The cases with suspected infections were also included 2.Improper sample 3.The sample consisted of biofilm form, 4.Improper culture techniques.
Biofilms are communities of microorganisms attached to a solid surface (either an abiotic or biotic) consisting of sessile phenotypes, these are difficult to culture by ordinary culture techniques. MRSA readily forms biofilms [6].
The values obtained in this study regarding MRSA infection may be a tip of the iceberg, with better culture techniques these values may still go up.
The small sample size, lack of advanced isolation and culture techniques of the organisms, the four patients in whom the methicillin sensitivity was not known are primary limitations of the study. Inclusion of the cases infected even before admitted to the study set up may not be true representation of the actual prevalence in either the community or the hospital, may represent only the share of the load borne by the hospital.
Various studies have shown that protocols for identification of MRSA carriage and treatment of an established infection have helped reduce the burden [8-10].
Considering the magnitude and seriousness of the problem, there is a definitive need for increased awareness regarding incidence, pathogenicity, preventive and treatment measures of MRSA infection. Formulation and implementing institutional policy for screening, culture techniques, antibiotic use and eradication methods is the need of the hour.
References
- Boyce JM. MRSA patients: proven methods to treat colonization and infection. J Hosp Infect 2001;48 (suppl- A): 9-14.
- Patel A,Calfee RP, Plante M, Fischer SA, Arcand N, Born C. Methicillin resistant Staphylococcus aureus in orthopaedic surgery. J Bone Joint Surg (Br) 2008; 90- B: 1401-1406.
- Voss A, Milatovic D,Wallrauch-Schwarz C, Rosdahl VT, Braveny I. Methicillin- resistant staphylococcus aureus in Europe. Eur J Clin Microbiol Infect Dis 1994; 13: 50-55.
- 4.Giannoudis PV, Parker J, Wilcox MH.Methicillinresistant staphylococcus aureus in trauma and orthopaedic practice.J Bone Joint Surg (Br)2005; 87-B: 749-54.
- Turek SL,Orthopaedics principles and their application(vol-I).4th ed. New Delhi: Jaypee brothers;1984.pp 258-282.
- Thomas JG, Lehman DC, Biofilms: Architects of disease. In : Mahon CR,Lehman DC,Manuselis G,editors. Textbook of diagnostic microbiology,3rd ed. New Delhi:Elsevier;2007.pp 884-898.
- Roche SJ, Fitzgerald D, O’RourkeA, Mc Cabe JP.Methicillin-resistant Staphylococcus aureus in an Irish orthopaedic centre:a five year analysis. J Bone Joint Surg(Br) 2006; 88-B: 807-811.
- Shukla S, Nixon M, Acharya M, Korim MT, Pandey R. Incidence of MRSA surgical- site infection in an orthopaedic trauma unit. J Bone Joint Surg (Br) 2009; 91-B: 225-228.
- S.Mathanraj, S.Sujatha, K.Sivasangeetha, SC Parija. Screening for methicillin resistant staphylococcus aureus carriers among patients and health care workers of a tertiary care hospital in south India.Indian journal of microbiology 2009; 27-1: 62-64.
- Nixon M, Jackson B, Varghese P, Jenkins D, Taylor G. Methicillin resistant staphylococcus aureus on orthopaedic wards: incidence , spread, mortality, cost and control. J Bone Joint Surg (Br) 2006; 88-B: 812-817.