ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2023) Volume 34, Issue 1
The ĂŹ?-shaped reverse guidewire technique for extremely angulated bifurcation of severe left main disease.
Nguyen Thuong Nghia*, Nguyen Hoang Tai My
Department of Interventional Cardiology, Cho Ray Hospital, Ho Chi Minh City, Vietnam
- Corresponding Author:
- Nguyen Thuong Nghia
Department of Interventional Cardiology
Cho Ray Hospital
Ho Chi Minh City
Vietnam
Accepted date: February 22, 2023
We describe a clinical case of 51 year-old man with severe left main bifurcation lesion who had 90% stenosis of distal LM and 90% stenosis of the LAD ostium. The LAD take-off was highly angulated from the LM and a guidewire was very difficult to get into the vessel. For dealing with this rare situation, we used the new modified guidewire technique in which the guidewire was “ϕ”, so-called “ϕ-shape” reverse guidewire technique. This technique is considered to be a feasible method for treating extremely angulated bifurcation lesion of severe LM disease.
Keywords
Reverse guidewire technique, Left main bifurcation, Backstop technique.
Introduction
In the practice of Percutaneous Coronary Intervention (PCI), an important step often concerns the successful wiring of a side branch of a bifurcation lesion. Although this usually has not many difficulties, some coronary anatomies can cause technical challenges. One of the most difficult anatomies is when a branch vessel arises at a retroflexed steep angle from the main vessel and is severe stenosed. Moreover, it is a rarely particular case of an extreme angulation of the Left Circumflex (LCx) or Left Anterior Descending (LAD) artery that is severely stenosed and the distal Left Main (LM) is also severely stenosed. This article reviews a case of true severe LM bifurcation lesion who had a severe stenosis of the ostium LAD which was angulated steeply from the LM, and was successfully treated using a guidewire with ϕ-shaped technique.
Illustrated case
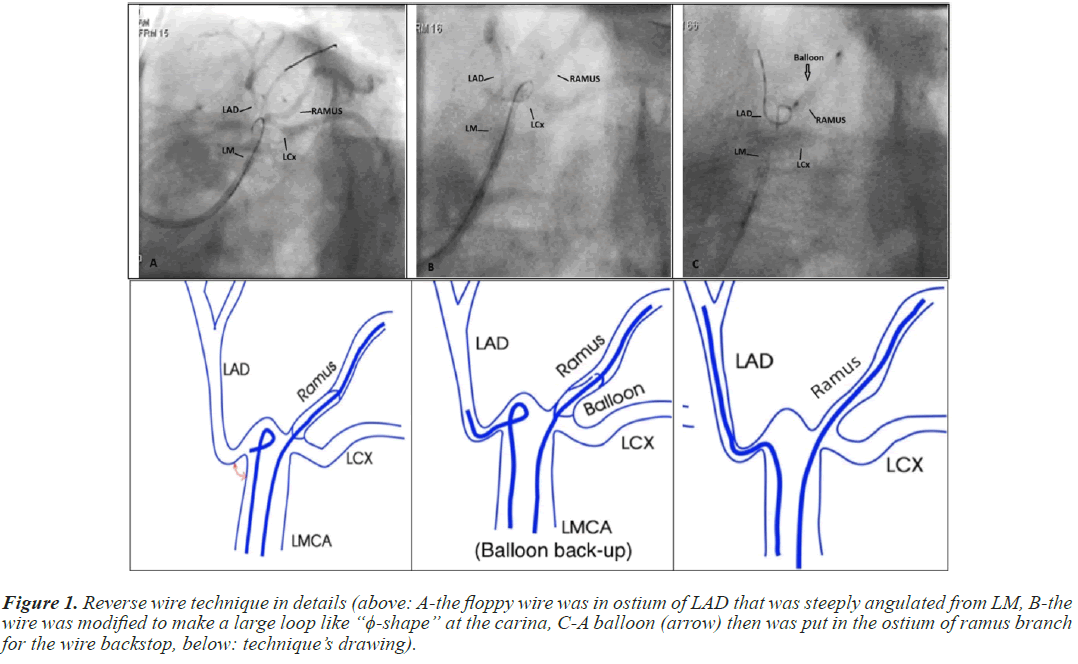
A male patient, 51 year-old, was admitted to Cho Ray hospital with the chief complaint of chest pain on mild exertion. 30 days before this admission the patient had chest pain and dyspnea on mild exertion, which gradually increased in the intensity and the duration. A coronary CT angiogram performed at a local medical center revealed severe stenosis (90%) of left main and then he was referred to Cho Ray Hospital. His previous history was hypertension, hypercholesterolemia and heavy smoking. The vital signs were normal with heart rate 80 bpm, blood pressure 120/70 mmHg, BMI 25.5 kg/m2 with no abnormalities on heart and lung examinations. Blood test results were total cholesterol 149 mg/dl, HDL-C 42 mg/dl, LDL-C 93 mg/dl, triglyceride 253 mg/dl, cardiac troponin I<0.006 ng/ml and good renal function with eGFR 99 ml/min/1.73m2. The chest X-ray and ECG were normal. The echocardiography revealed good left ventricular function EF 55% (Teichholz) with no wall region motion abnormality. The patient was diagnosed unstable angina (GRACE Score 110) with hypertension and dyslipidemia. The patient was recommended to undergo coronary angiogram. His coronary angiography which was performed via right radial access with Judkins Technique using catheter JL3.5, JR 4 (5F) revealed a bifurcation lesion with 90% stenosis of distal LM and 90% stenosis of ostial LAD, and 70% diffuse stenosis of mid LAD (Figure 1). The SYNTAX score was 29.
Figure 1: Reverse wire technique in details (above: A-the floppy wire was in ostium of LAD that was steeply angulated from LM, B-the wire was modified to make a large loop like “ϕ-shape” at the carina, C-A balloon (arrow) then was put in the ostium of ramus branch for the wire backstop, below: technique’s drawing).
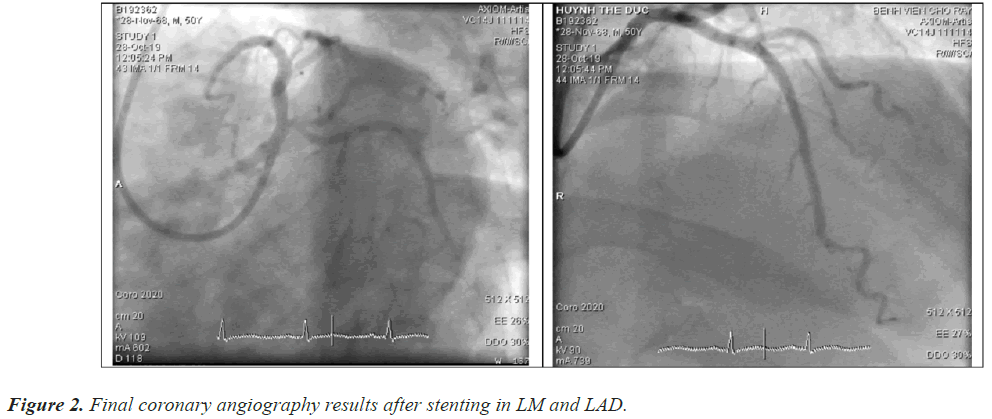
He underwent PCI procedure via right radial access with guiding Catheter CLS 3.0 (6F). We tried to directly wire this branch vessel with both floppy-tipped and hydrophilic wires. We also used the twin-pass catheter (Crusade catheter) but it still failed. We then moved on to another technique. Based on the morphology of the lesion, we used the reverse wire technique with a very floppy wire modified a little bit in order to make a large loop in the carina. The hydrophilic, 0.014”, very floppy guidewire (SUOH) with a ϕ-shaped, large loop in the carina directed toward the LAD ostium while using one balloon in the ostium of the ramus branch for the wire not to prolapse into LCx/OM branch (balloon backstop technique) and to support the wire to enter the ostium LAD successfully. Pre-dilatation was done with a semi-compliant balloon 2.0 × 15 mm. Finally, 2 stents were implanted successfully (XIENCE Sierra 2.75 × 38 mm (20 atm) in middle LAD and XIENCE Xpedition 3.5 × 48 mm (18 atm) in LM-middle LAD). The final result was shown in Figure 2.
Discussion
The incidence of complex coronary interventions is increasing in the catheterization room, perhaps because the patients often come to us in late stages of the coronary disease and are reluctant to CABG. Besides, bifurcation lesions with the side branch meeting the main vessel at a angle of more than 90° are occasionally present. One of the cases is at the left main bifurcation. An important step in complex PCI of bifurcation lesions often concerns the successful wiring of a side branch [1,2]. There are many conventional methods for manipulating the guidewire into a highly retroflex angulated side branch such as changing wire to a stiffer or hydrophilic polymer coated one, making a large, more than 90° curve of the wire tip or utilizing a micro or multifunction catheter such as Sasuke, Twin pass, Crusade, etc., [3].
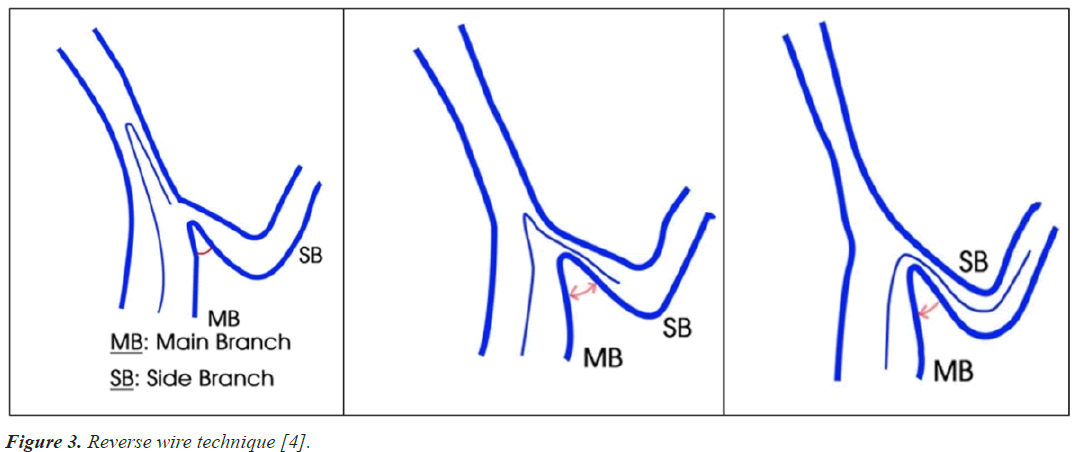
As we know, the reverse wire technique was first introduced by Japanese authors since 2008 by Kawasaki and improved later in 2013 by Watanabe with the use of a double-lumen catheter [4,5]. Thanks to this technique, the success rate increased significantly. In this technique, tip of a hydrophilic wire is made as a J loop by engaging onto one side branch. After that, it is pointed toward the target branch vessel before the wire is carefully pulled back until it catches and goes into the side branch ostium. Being pulled backward farther, it migrates more into the side branch. Sometimes we initially make a hairpin-like bend at a point 3-5 cm from the wire tip before inserting the wire into the main vessel until it traps the ostium of an extremely retroflex side branch (Figure 3) [4,6].
Figure 3: Reverse wire technique [4].
In this case, initially we utilized the conventional methods such as changing the hydrophilic wire to a stiffer one (Pilot 50, Fielder), making a large, more than 90° curve in the wire tip, using micro-catheter (Finecross) and dual lumen catheter (Crusade) but they all failed. Therefore, we decided to use the reverse wire technique. Sometimes it was not easily to solve a problem by one method. The wire continuously prolapsed into the ramus branch so that we needed the support of a balloon standing in another branch. This is so-called backstop technique. We combined two techniques to perform the wiring into LAD artery successfully. Discussing about the wire type, we considered the SUOH hydrophilic wire was the most suitable one for this technique because we can easily modify its shape. By the way, it had less resistance, and was relatively softer than other wires. Moreover, we have tested two others such as hydrophilic guidewire (Whisper MS) and non-hydrophilic guidewire (PT 2 floppy) before, but the pushability and steerability of them both were not as good as those of SUOH wire.
Although extremely angulated birfurcated lesion is one of very difficult lesions and there are several techniques to solve [7]. But this case is the special steep angulated left main case that we utilized combined reversed technique with balloon support in the beside branch to overcome the lesion successfully.
Conclusion
However, our technique may have some limitations. Firstly, this technique needs a rather large diameter of the main vessel to have enough room for the wire curve so that it will be not used for a small vessel or distal bifurcations. Secondly, vessel dissection and wire entrapment may be the main complications. Therefore, interventionists need pay deep attention doing this technique. The classic technique using only the wire like ϕ -shaped reverse guidewire technique may be a feasible method for treating of steeply angulated bifurcation lesions, especially in severe LM disease.