ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 15
The value of detecting serum PCT and IL-6 levels during the perioperative period of primary hip and knee arthroplasty
Lixuan Zhang1,2, Daozhang Cai3* and Hanming Guo2
1Southern Medical University, Guangzhou, PR China
2Department of Orthopaedic Surgery, Huizhou Municipal Central Hospital, 41st Eling North RD, Huicheng District, Huizhou, PR China
3Academy of Orthopaedics, Guangdong Province, Department of Orthopaedics, the Third Affiliated Hospital, Southern Medical University, Guangzhou, PR China
- *Corresponding Author:
- Daozhang Cai
Academy of Orthopaedics
Guangdong Province
The Third Affiliated Hospital
Southern Medical University
Guangzhou, PR China
Accepted on June 30, 2017
Objective: The current study aimed to characterize the variation of serum PCT and IL-6 levels and look the specificity and the sensitivity in diagnosing pneumonia, urinary and superficial surgical site infections during the perioperative period of primary hip and knee arthroplasty.
Methods: This observational study included 73 patients undergoing primary hip and knee arthroplasty. Serum Procalcitonin (PCT), and Interleukin-6 (IL-6) were measured preoperatively (D0) and at postoperative day 4 (D4) and day 6 (D6). The sensitivity, specificity and predictive values of PCT and IL-6 were assessed.
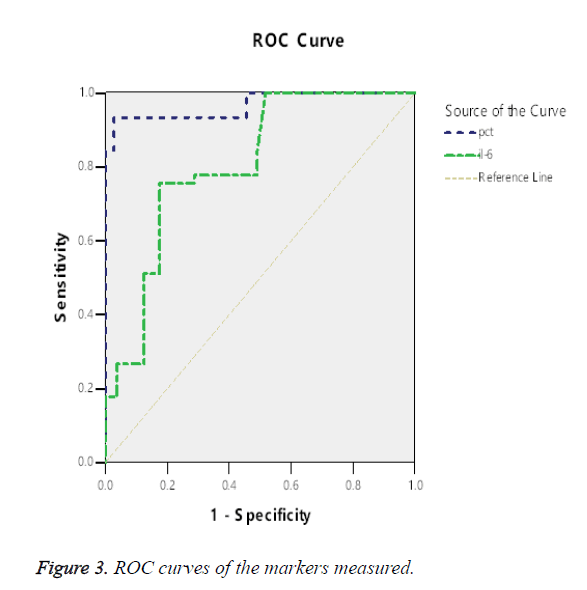
Results: On comparison of the mean of PCT levels between infection group and non-infection group, a significant difference was seen at D6 (day 6) (p<0.01), but with no significant difference for IL-6. For PCT, the AUC was 0.967 (95% CI, 0.934-1.000), for IL-6 the AUC was 0.806 (95% CI, 0.754-0.859). The PCT value was a significant predictor of infection (AUC>0.9). For PCT, the cut-off point of 0.1385 ng/ml had a sensitivity of 93.3% and a specificity of 97.3%. However, the IL-6 was a less significant predictor for infection (0.7<AUC<0.9). The IL-6 value of 30.215 pg/ml had a sensitivity of 77.8% and specificity of 71.3%.
Conclusions: It is valuable to monitor the variation trend of PCT and IL-6 as a marker for possible infection in the early post-operative period. Detecting PCT may be more valuable than using IL-6 in the diagnosis sepsis pathological changes in the perioperative period.
Keywords
Procalcitonin, Interleukin-6, Arthroplasty, Perioperative infection.
Introduction
One of the major complications of total knee and hip joint arthroplasty is periprosthetic joint infection, which complicates revision arthroplasty in as many as 10%-20% of patients in some series [1-4]. Any infections, including the pneumonia, urinary and surgical site infections should be cured during the perioperative period of arthroplasty, which may lead to the occurrence of periprosthetic joint infection. So it is crucial to detect any infections during the perioperative period of arthroplasty in order to rapidly initiate adequate antimicrobial therapy [5-7]. Biomarkers, such as C-Reactive Protein (CRP), White Blood Cell count (WBC) and Erythrocyte Sedimentation Rate (ESR) can be used to aid in diagnosis, therapeutic monitoring, and risk stratification. However, these blood parameters lack sensitivity and specificity in discriminating the inflammation of bacterial infection from that of the surgical injury response [8-13]. Numerous studies suggest that Procalcitonin (PCT) has been shown to be a more accurate marker in detection of early postoperative infection after cardiac, intestinal and major neural surgeries compared to the standard laboratory parameters, such as CRP and WBC [14-17]. PCT, the 116-amino acid pro-hormone of calcitonin, is mainly produced as a precursor hormone of calcitonin by the neuroendocrine cells of the thyroid and lung; alternative pathological pathways in patients with inflammation and sepsis were described. Bacterial endotoxin has been shown to release PCT into the circulation directly [18,19]. It will increase 2-4 h following an appropriate exposure such as sepsis [20-24], and reaches its peak after 6 h and has a half-life of 25-30 h [25,26]. And then a rapid decline following treatment or removal of the underlying trigger. Comparing with CRP, whose peaks only after 36 h, PCT can be detected quicker. IL-6 (interleukin- 6) is produced as an acute phase protein to stimulate immune response by monocytes and macrophages [27,28]. Its serum concentration is about 1 pg/ml in healthy subjects, but it increases rapidly in cases of inflammation, infection, and traumatic injury. It may increase to 30-430 pg/mL for as long as 3 d following total joint arthroplasty [11,29], rapidly returns to normal value and is not elevated in patients with aseptic loosening [30,31]. Serum IL-6 has been shown to be a valuable and even more accurate marker than either the erythrocyte sedimentation rate or the CRP level for the detection of chronic PJI [11]. Disadvantages of IL-6 test are that it is non-specific and may increase in response to several diseases with acute inflammatory reactions.
However, there is much debate in the literature as to what cut-off value they should represent in different types of surgery and local bacterium infection. No studies have detected which better biomarker is helping to the diagnosis of infections around the perioperative period of primary hip and knee arthroplasty. In the present study, we analyzed the kinetics of PCT and IL-6 during the perioperative period of arthroplasty in our institution, including pre-operations and post-operations.
The aim of the study was to characterize the baseline of the two biochemical tests, helping to make the new cut-offs of PCT and IL-6 during the perioperative period of arthroplasty, and detected their difference during the perioperative period. Secondary objectives included looking the specificity and the sensitivity at the characteristics of PCT and IL-6 in diagnosing infections during the perioperative period of arthroplasty.
We hypothesized that monitoring the variational trend of serum PCT and IL-6 levels would help to detect any infections during the perioperative period of arthroplasty, including pneumonia, urinary and superficial surgical sites infections, to rapidly initiate adequate antimicrobial therapy, which may reduce the opportunity of deep surgical sites infection and periprosthetic infection.
Materials and Methods
Patients
The study included 73 individuals (19 males and 54 females, mean age 64.26 y, range 34.17-93) in our Orthopaedic Department between Jan 2015 and Sep 2015. The arthroplasty included primary total hip replacement and total knee replacement.
Exclusion criteria were history of previous joint infection, acute or chronic systemic inflammatory disease, pneumonia, urinary infection, any skin and musculoskeletal system infection, cardiac, renal (creatinine clearance<50 mL/min), coagulopathy, malignoma and operative procedure within 3 months before admission.
At the end of the study, patients were divided into two groups: Non-Infective group (Group 1) and Confirmed postoperative infection group (Group 2) based on the below criteria. The postoperative infections in Group 2 included pneumonia, urinary tract infection occurring within 2 weeks and superficial surgical sites infection occurring within 30 d. There were no other postoperative complications except infections during the inpatient stay, in the first month after operation, and at the final follow-up of 12-20 months.
A diagnosis of pneumonia required a new pulmonary infiltrate at time of hospitalization, and at least one of the following: New or increased cough, leucocytosis, leukopenia, or left shift pattern on white blood cell count, temperature>37.8°C, or <35.6°C. A diagnosis of urinary tract infection required at least one of the symptoms like fever (>38°C), dysuria, pollakiuria, suprapubic tenderness and having ≥ 105 CFU/ml of one or two types of bacteria or culture-negative patients having at least two of the above-mentioned symptoms and one of the seven criteria defined by Centers for Disease Control and Prevention like nitrite test positivity, pyuria were included in the study [32]. Asymptomatic patients were excluded.
The diagnosis of superficial surgical site infection included infection that occurs within 30 d after the operation on surgical site, excepted deep incisional Surgical Site Infection (SSI) and Periprosthetic Joint Infections (PJI) [33,34].
The classification of SSI is shown on Table 1 [34].
| Superficial incisional SSI | Infection involves only skin or subcutaneous tissue and at least one of the following: |
| -Purulent drainage from the superficial incision, with or without laboratory result. | |
| -Isolated microorganism from a culture of fluid or tissue. | |
| -On the surgical site: pain, swelling, heat or redness. | |
| -Diagnosis of superficial incisional SSI established by surgeon or attending physician. | |
| Deep incisional SSI | Infection involves deep soft tissues such as fascia or muscle layer and at least one of the following: |
| -Purulent drainage from the deep incision but not from organ or organ space component. | |
| -A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs: fever (>38°C), localized pain or tenderness. | |
| -An abscess or other evidence of deep infection that is found on direct examination, by histopathologic or radiologic examination. | |
| -Diagnosis of deep incisional SSI made by a surgeon or attending physician. | |
| Organ or space SSI | Infection involves organs or spaces, other than the incision site and at least one of the following: |
| -Purulent drainage from the organ or space. | |
| -Isolated microorganism from a culture of fluid or tissue. | |
| -An abscess or other evidence of deep infection that is found on direct examination or by histopathologic or radiologic examination. | |
| -Diagnosis of organ/space SSI by a surgeon or attending physician. |
Table 1. Classification of SSI.
The study was approved by the local ethics committee. Informed consent was obtained in all cases prior to enrolment. Operational procedure comprised standardized unilateral minimal invasive implantation of an un-cemented or cemented total hip prosthesis based on the preoperative protocol through a posterolateral approach, and cemented total knee prosthesis through anterior midline approach. The surgery was performed in operating rooms with vertical laminar flow and use of helmet aspirator suits and double gloves. Skin was prepared with alcohol and iodine lavage. Over 94% of hip and knee surgeries were performed under spinal/epidural anesthesia at our institution. Prophylactic antibiotics (Cefuroxime 1.5 g) were given 1 h before surgery and every 8 h for 48 h postoperatively. All patients received antithrombotic prophylaxis with low molecular-weight heparin calcium injection, 4100 AXaIU per day in hospital starting from 12 h after surgery. Rivaroxaban, 10 mg per day, following outpatient for 2 weeks.
Laboratory methods
Blood samples of all patients were obtained pre-operative and on the 4th and 6th postoperative days. Serum levels of PCT and IL-6 (KRYPTOR, ECLIA, Cobas 8000, Roce Diagnostics GmbH, and Mannheim, Germany) were measured at the Institute for Clinical Chemistry at Huizhou Municipal Central Hospital.
Statistical analysis
Descriptive data analyses were carried out with Statistical Package for Social Sciences software, version 19.0 for Windows. Comparing the constituent ratio difference between 2-independent-samples, The Pearson chi-square was used. Comparing the difference between 2-independent-samples, The Mann-Whitney U-test was used if the variance was irregular, otherwise the t-test would be used. Comparing the difference between 2-Paired-samples. The Paired-samples T test would be used. Using the Box-plot to show the distribution range of PCT and IL-6 levels. Using the Receiver-Operator-Characteristics (ROC) curves to measure the best cut-off values and calculated individual specificity and sensitivity between PCT and IL-6.
Results
Infection was diagnosed in 9 (12.33%) of 73 patients and involved the pneumonia (one), urinary (two) and superficial surgical site infection (six). Other 64 patients haven’t showed local or systemic complications during the period of observation, such as fever or wound healing problems. The patient demographics and details are given in Table 2. Though uneven in number, there was no statistical difference in age (p=0.563), patient gender (p=0.08) or joint distribution (p=1) between the groups.
| Group | n | Mean age (Mean ± standard deviation) |
Sex (Female/Male) | Hip/Knee |
|---|---|---|---|---|
| Group 1 | 64 | 63.847 ± 10.189 | 50/14 | 39/25 |
| Group 2 | 9 | 67.222 ± 16.438 | 4/5 | 5/4 |
| t/χ2 | -0.6 | 3.064 | 0 | |
| p | 0.563 | 0.08 | 1 |
Table 2. Patient demographics.
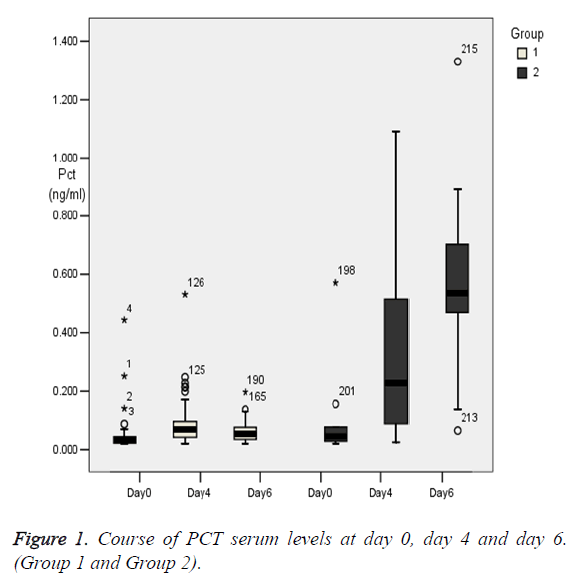
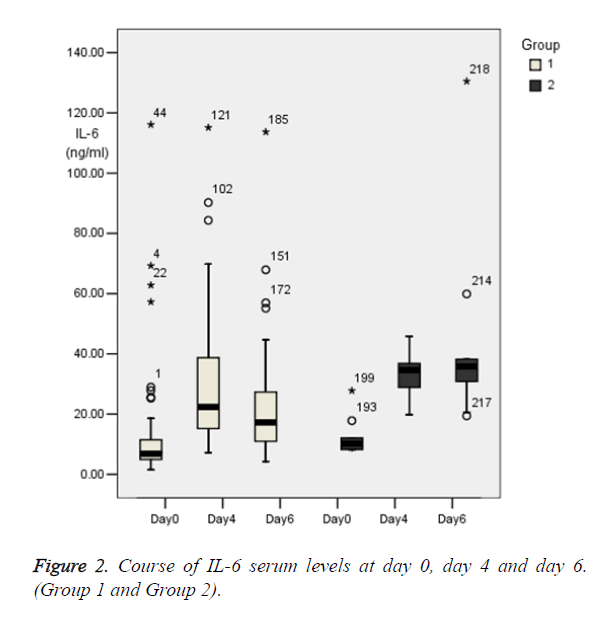
The preoperative PCT mean serum levels (0.045 ± 0.06 ng/ml) were roughly in the normal range in group 1 (Table 3), with 54 patients (84%) had concentrations of PCT within the normal range (0-0.05 ng/ml). In contrast, the preoperative IL-6 mean serum levels (13.06 ± 18.57 pg/ml) were higher than the normal range (0-7 pg/ml) (Table 3), with only 33 patients (52%) had concentrations of IL-6 within the normal range. Thereafter, the levels of PCT (0.086 ± 0.078) increased rapidly on the fourth day (nearly 2-fold higher than baseline mean values) (Table 3), and have significant difference with D0 (p<0.01, Table 4). However, it dropped rapidly on the sixth day (0.061 ± 0.035 ng/ml) as returning close to the height of normal range (Figure 1), and have no significant difference with D0 (p>0.01, Table 4). Levels of IL-6 increased rapidly and reaching a peak on the fourth day (29.73 ± 20.96 pg/ml), and have significant difference with D0 (p<0.01, Table 4). Then, the IL-6 declined on the sixth day (22.12 ± 17.62 pg/ml), and still have significant difference with D0 (p<0.01, Table 4). The same with the group1, levels of PCT and IL-6 in group 2 increased rapidly on the fourth day. Contrasting to the group 1, levels of PCT and IL-6 in group 2 increased constantly on the sixth day (Figure 2). From the clinical point of view, the infection events can be found in these patients during postoperative follow-up. On comparison of the mean of PCT level between group 1 and group 2, a significant difference was seen at D6 (day 6) (p<0.01), but with no significant difference at D0 (day 0) and D4 (day 4) (p>0.01). However, by comparing the mean of IL-6 level between group 1 and group 2, no significant difference was seen at D0, D4 and D6 (day 6) (p>0.01) (Table 3).
| PCT (Mean ± standard deviation ) (ng/ml) | IL-6 (Mean ± standard deviation ) (pg/ml) | |||||
|---|---|---|---|---|---|---|
| D0 | D4 | D6 | D0 | D4 | D6 | |
| Group1 | 0.045 ± 0.06 | 0.086 ± 0.078 | 0.061 ± 0.035 | 13.06 ± 18.57 | 29.73 ± 20.96 | 22.12 ± 17.62 |
| Group2 | 0.112 ± 0.177 | 1.113 ± 1.925 | 1.228 ± 2.16 | 12.56 ± 6.459 | 33.204 ± 7.753 | 45.279 ± 34.047 |
| t/Z | Z=-1.509 | Z=-2.450 | Z=-4.138 | t=0.071 | t=-0.943 | t=-2.003 |
| p-value | 0.131 | 0.014 | 0 | 0.943 | 0.353 | 0.078 |
Table 3. Descriptive statistics of parameter.
| PCT | IL-6 | ||||
|---|---|---|---|---|---|
| D4 | D6 | D4 | D6 | ||
| t | Group 1 | -3.577 | -2.051 | -5.3 | -3.173 |
| Group 2 | -2.21 | -4.018 | -8.749 | -2.71 | |
| p-value | Group 1 | 0.001 | 0.04 | 0 | 0.002 |
| Group 2 | 0.058 | 0.004 | 0 | 0.027 | |
Table 4. Comparison test with D0.
One patient showed a high-level PCT course with PCT peak levels of 0.532 ng/ml at D4, but dropped to 0.197 ng/ml at D6 (Figure 1). From the clinical point of view these findings cannot be explained; there were no clinical events in these patients neither during the hospital stay or during the 12-month postoperative follow-up. One patient, whose PCT level is normal all days, but showed a high-level IL-6 course with peak levels of 116.1 pg/ml at D0, then dropped to 43.37 pg/ml at D4 (Figure 2). Another patient, whose PCT level is also at low levels, but showed a high-level IL-6 course with peak levels of 115.1 pg/ml at D4, and 113.7 pg/ml at D6, then dropped to 51.68 pg/ml at D8. There were no clinical events in these patients neither during the hospital stay nor during the 12- month postoperative follow-up. We think the high-level IL-6 course maybe associate with the aseptic inflammation, as a serious knee synovitis was found in those knees.
To measure the best cut-off values and calculated individual specificity and sensitivity between PCT and IL-6, we used Receiver-Operator-Characteristics (ROC) curves (Figure 3). A summary of the results is given in Table 5. To compare the capability of the two significant biomarkers to distinguish patients without infection from patients with infection, the area under the curve was calculated. For PCT, the area under the curve was 0.967 (95% CI, 0.934-1.000), for IL-6 the area under the curve was 0.806 (95% CI, 0.754-0.859). Based on the data above, the PCT value was a significant predictor of infection (AUC>0.9). For PCT, the cut-off point of 0.3325 ng/mL had a sensitivity of 84.4% and a specificity of 100%. (Figure 3). At a cut-off of 0.1385 ng/mL, PCT is found to be 93.3% sensitive and 97.3% specific in diagnosing positive infections. However, the IL-6 was a less significant predictor for infection (0.7<AUC<0.9). The IL-6 value of 18.975 pg/ml had a sensitivity of 100% and specificity of 48.3%. At a cut off of 30.215 pg/ml, IL-6 is found to be 77.8% sensitive and 71.3% specific in diagnosing positive infections. For combining different parameters, the point with the minimal distance on the ROC curve was the optimal threshold. Obviously, PCT has the higher sensitivity value and specificity value compared with IL-6 (Figure 3).
| Parameter | AUC (95% CI) | Cut-Off | Sensitivity (%) | Specificity (%) | Youden index |
|---|---|---|---|---|---|
| PCT | 0.967 (0.934 to 1.000) |
0.0635 ng/ml | 100 | 54.4 | 0.54 |
| 0.1385 ng/ml | 93.3 | 97.3 | 0.91 | ||
| 0.3325 ng/ml | 84.4 | 100 | 0.84 | ||
| IL-6 | 0.806 (0.754 to 0.859) |
18.975 pg/ml | 100 | 48.3 | 0.48 |
| 30.215 pg/ml | 77.8 | 71.3 | 0.49 | ||
| 122.1 pg/ml | 17.8 | 100 | 0.18 |
Table 5. Cut-off values and calculated individual specificity and sensitivity between PCT and IL-6.
Discussion
Any infections, including the pneumonia, urinary and superficial surgical site infections will be dangerous during the perioperative period of arthroplasty. As it may lead to the occurrence of periprosthetic joint infection, which is a serious postoperative complication following arthroplasty. [35-37]. Inflammatory biomarkers play a pivotal role in helping to find the infections earlier. However, the lack of sensitivity and specificity in discriminating the inflammation of infection from that of acute phase response is a challenge in precise diagnosis [10-13,38,39]. Recent research suggests that PCT and IL-6 are more helpful in diagnosis of sepsis and Systemic Inflammatory Response Syndrome (SIRS) and can be detected more accurate in early postoperative infection after major neural surgeries compared to the standard laboratory parameters (such as CRP and WBC) [14-17,40]. Previous studies have reported that, the IL-6 levels increase rapidly after surgery, infection, and traumatic injury, and may increase to 30-430 pg/mL for as long as three days following total joint arthroplasty [11,29]. Comparing with previous studies, we found some different characterization of the serum PCT and IL-6 levels during the perioperative period of primary hip and knee arthroplasty. In this study, we prospectively analyzed the sensitivity and specificity of PCT and IL-6 for detecting perioperative infections.
(2) The cut-offs of PCT and IL-6 during the perioperative period of arthroplasty and the predictive values in diagnosing perioperative infection.
Our study has also suggested the possibility of using new cut-offs to differentiate elevations in PCT and IL-6 due to aseptic inflammatory reaction versus sepsis. Many researches have demonstrated that PCT and IL-6 not only respond directly to bacterial endotoxin, but also stimulated by non-infective inflammation, such as surgical trauma, aseptic synovitis [18,19,41-44]. So the cut-offs of PCT and IL-6 during the perioperative period may be higher than the normal range.
There is much debate as to what cut-off value of PCT differentiates infection from the acute phase response [41,45]. Bottner et al. have reported in detection of deep chronic periprosthetic infection with PCT levels>0.3 ng/mL while the combination of IL-6 levels>12 ng/L [29]. Syed et al. have reported that fifty patients (85%) had concentrations of PCT within the normal range (<0.5 ng/ml) on days 1, 3 and 5 post-operation, with PCT levels are not significantly elevated by the trauma of total hip and knee arthroplasty [46]. Hogle et al. has shown PCT as a highly sensitivity but low specificity at a cut-off of 0.25 ng/ml [43]. However, we found that the cut-off points of 0.3325 ng/ml had a highest sensitivity (84.4%) and specificity (100%). Meanwhile, Stucker et al. have shown PCT as a poorly sensitive marker with high specificity at a cut-off of 0.5 ng/ml [22,44,45]. Bottner et al. have reported the high specificity (0.98) but low sensitivity (0.33) in detection of deep chronic periprosthetic infection with PCT levels>0.3 ng/mL [46]. Similarly, in our study, at a cut off of 0.1385 ng/ml, PCT is found to be 93.3% sensitive and 97.3% specific in diagnosing positive infections.
In the current study, 0.1385 ng/m is taken as the cut-off for PCT and 30.215 pg/ml is taken as the cut-off for IL-6 in diagnosing perioperative infection, including the pneumonia, urinary and superficial surgical site infection.
So, our study may be helpful in making the new cut-offs of PCT and IL-6. Any significant elevations of PCT referring to the new cut-off may suggest an occurrence of infection during the perioperative period of arthroplasty.
Numerous researches have shown that PCT is elevated in cases of bacterial infection or sepsis and levels are considerably higher in bacterial infections than in viral infections [20,21,24]. PCT shows a favourable kinetic profile for use as a clinical marker: it reaches its peak after 6 h and has a half-life of 25-30 h [26,47]. Some studies has reported that IL-6 is a sensitive marker for bacterial infection after total hip arthroplasty [29,48]. Its serum level increases rapidly after surgery, with a peak after 3-6 h, and has a mean half-life of 15 h and decreases rapidly to normal concentrations [48]. Some study shown serum IL-6 level can increase from 1 pg/mL to 30-430 pg/mL for as long as three days following total joint arthroplasty [11,29]. It will reach the peak level two days after total joint arthroplasty, then rapidly returns to normal value [30,31]. So the elevation of the PCT and IL-6 levels causing by the surgical trauma may nearly drop to the baseline level on day 4. Based on our study, the serum PCT and IL-6 levels will keep on dropping at day 6 if without local or systemic complications during the period of observation, such as pneumonia, urinary or surgical site infection. It means that any significant elevations of PCT and IL-6 at day 6 may suggest an occurrence of infection or other inflammation.
All patients undergoing arthroplasty were given intraoperative antibiotics (most commonly intravenous Cefuroxime), continued for 48 h postoperatively. So it is not easy occurring infection during day 1 and day 2 postoperative. So, the incidence of infection during the period following the stop using antibiotics might be much more.
Perioperative superficial wound infections are more common than deep prosthetic infection. The presence of a wound infection has been identified as a significant risk factor for development of prosthetic infection. So, it is critical to identify a wound infection. We know that most incision bleeding concentrate during the early postoperative period, which means the presence of wound infection following the bleeding, may occur during days 2-4. Meanwhile, the joint drainage tube, being placed during arthroplasty, will be kept for 48 h postoperative. It is therefore not surprising that deep infections related with tube occurred within this period. In a word, based on the characterize of perioperative period infection and the variation of PCT and IL-6,we proposed that detecting PCT and IL-6 on day 4 and day 6 may be more valuable in the diagnosis asepsis pathological changes in the preoperative period.
In conclusion, our study shows the characteristic feature of serum PCT and IL-6 levels during the perioperative period of primary hip and knee arthroplasty. It is valuable monitoring the variational trend of PCT and IL-6 as a marker for possible infection in the early post-operative period. Detecting PCT may be more valuable than using IL-6 in the diagnosis sepsis pathological changes in the perioperative period. Meanwhile, making the new cut-offs of PCT and IL-6 during the perioperative period of arthroplasty may be helpful in discriminating the inflammation of infection from that of acute phase response.
Nevertheless, our study does have some limitations. Firstly, it represents a single center experience with the number of patients less than 100. Secondly, the study design was lack of reference group with PJI. Thirdly, the patients with sepsis pathological changes are only 9, which may increase sampling error.
References
- Esposito S, Leone S. Prosthetic joint infections: microbiology, diagnosis, management and prevention. Int J Antimicrob Agents 2008; 32: 287-293.
- Ghanem E, Azzam K, Seeley M, Joshi A, Parvizi J. Staged revision for knee arthroplasty infection: what is the role of serologic tests before reimplantation? Clin Orthop Relat Res 2009; 467: 1699-1705.
- Haleem AA, Berry DJ, Hanssen AD. Mid-term to long-term follow-up of two-stage re-implantation for infected total knee arthroplasty. Clin Orthop Relat Res 2004; 428: 35-39.
- Savarino L, Tigani D, Baldini N, Bochicchio V, Giunti A. Pre-operative diagnosis of infection in total knee arthroplasty: an algorithm. Knee Surg Sports Traumatol Arthrosc 2009; 17: 667-675.
- Costerton JW, Post JC, Ehrlich GD, Hu FZ, Kreft R, Nistico L, Kathju S, Stoodley P, Hall-Stoodley L, Maale G, James G, Sotereanos N, DeMeo P. New methods for the detection of orthopedic and other biofilm infection. FEMS Immunol Med Microbiol 2011; 61:133-140.
- Savarino L, Baldini N, Tarabusi C, Pellacani A, Giunti A. Diagnosis of infection after total hip replacement. J Biomed Mater Res B Appl Biomater 2004; 70: 139-145.
- Van Kleunen JP, Knox D, Garino JP, Lee GC. Irrigation and debridement and prosthesis retention for treating acute periprosthetic infections. Clin Orthop Relat Res 2010; 468: 2024-2028.
- van Leeuwen MA, van Rijswijk MH. Acute phase proteins in the monitoring of inflammatory disorders. Baillieres Clin Rheumatol 1994; 8: 531-552.
- Rafiq M, Worthington T, Tebbs SE, Treacy RB, Dias R, Lambert PA, Elliott TS. Serological detection of gram-positive bacterial infection around prostheses. J Bone Joint Surg Br 2000; 82: 1156-1161.
- Itasaka T, Kawai A, Sato T, Mitani S, Inoue H. Diagnosis of infection after total hip arthroplasty. J Orthop Sci 2001; 6: 320-326.
- Di Cesare PE, Chang E, Preston CF, Liu CJ. Serum interleukin-6 as a marker of periprosthetic infection following total hip and knee arthroplasty. J Bone Joint Surg Am 2005; 87: 1921-1927.
- Mitaka C. Clinical laboratory differentiation of infectious versus non-infectious systemic inflammatory response syndrome. Clin Chim Acta 2005; 351: 17-29.
- Falcoz PE, Laluc F, Toubin MM, Puyraveau M, Clement F, Mercier M, Chocron S. Usefulness of procalcitonin in the early detection of infection after thoracic surgery. Eur J Cardiothorac Surg 2005; 27: 1074-1078.
- Laffey JG, Boylan JF, Cheng DCH. The systemic inflammatory response to cardiac surgery. Anesthesiol 2002; 97: 215-252.
- Jebali MA, Hausfater P, Abbes Z, Aouni Z, Riou B, Ferjani M. Assessment of the accuracy of procalcitonin to diagnose postoperative infection after cardiac surgery. Anesthesiol 2007; 107: 232-238.
- Laifer G, Wasner M, Sendi P. Dynamics of serum procalcitonin in patients after major neurosurgery. Clin Microbiol Infect 2005; 11: 679-681.
- Oberhofer D, Rumenjak V, Lazic J, Vucic N. Inflammatory indicators in patients after surgery of the large intestine. Acta Medica Croatica 2006; 60: 429-433.
- Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, Bohuon C. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab 1994; 79: 1605-1608.
- Reinhart K, Karzai W, Meisner M. Procalcitonin as a marker of the systemic inflammatory response to infection. Intensive Care Med 2000; 26: 1193-1200.
- Carrol ED, Thomson AP, Hart CA. Procalcitonin as a marker of sepsis. Int J Antimicrob Agents 2002; 20: 1-9.
- Hunziker S, Hugle T, Schuchardt K, Groeschl I, Schuetz P, Mueller B, Dick W, Eriksson U, Trampuz A. The value of serum procalcitonin level for differentiation of infectious from non-infectious causes of fever after orthopaedic surgery. J Bone Joint Surg Am 2010; 92: 138-148.
- Nascimento-Carvalho CM, Cardoso MR, Barral A, Araujo-Neto CA, Guerin S, Saukkoriipi A, Paldanius M, Vainionpaa R, Lebon P, Leinonen M, Ruuskanen O, Gendrel D. Procalcitonin is useful in identifying bacteraemia among children with pneumonia. Scand J Infect Dis 2010; 42: 644-649.
- Pramod J, Singh A. Sepsis biomarkers. Am J Med 2008; 121: 13.
- Ruiz-Alvarez MJ, Garcia-Valdecasas S, De Pablo R, Sanchez Garcia M, Coca C, Groeneveld TW, Roos A, Daha MR, Arribas I. Diagnostic efficacy and prognostic value of serum procalcitonin concentration in patients with suspected sepsis. J Intensive Care Med 2009; 24: 63-71.
- Gendrel D, Bohuon C. Procalcitonin, a marker of bacterial infection. Infect 1997; 25: 133-134.
- Martinot M, Sordet C, Soubrier M, Puechal X, Saraux A, Liote F, Guggenbuhl P, Legre V, Jaulhac B, Maillefert JF, Zeisel M, Coumaros G, Sibilia J. Diagnostic value of serum and synovial procalcitonin in acute arthritis: a prospective study of 42 patients. Clin Exp Rheumatol 2005; 23: 303-310.
- Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis 2004; 39: 206-217.
- Foglar C, Lindsey RW. C-reactive protein in orthopedics. Orthopedics 1998; 21: 687-691.
- Bottner F, Wegner A, Winkelmann W, Becker K, Erren M. Interleukin-6, procalcitonin and TNF-alpha: markers of peri-prosthetic infection following total joint replacement. J Bone Joint Surg Br 2007; 89: 94-99.
- Berbari E, Mabry T, Tsaras G, Spangehl M, Erwin PJ. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am 2010; 92: 2102-2109.
- Buttaro MA, Tanoira I, Comba F, Piccaluga F. Combining C-reactive protein and interleukin-6 may be useful to detect periprosthetic hip infection. Clin Orthop Relat Res 2010; 468: 3263-3267.
- Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. Am J Infect Control 1988; 16: 128-140.
- Surgical site infections: resources for patients and healthcare providers. CDC 2010.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection. Infect Control Hosp Epidemiol 1999; 20: 247-264.
- Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res 2008; 466: 1710-1715.
- Choong PFM, Dowsey MM, Carr D, Daffy J, Stanley P. Risk factors associated with acute hip prosthetic joint infections and outcome of treatment with a rifampinbased regimen. Acta Orthopaedica 2007; 78: 755-765.
- Phillips JE, Crane TP, Noy M, Elliott TSJ, Grimer RJ. The incidence of deep prosthetic infections in a specialist orthopaedic hospital. A 15-year prospective survey. J Bone Joint Surg Br 2006; 88: 943-948.
- van Leeuwen MA, van Rijswijk MH. Acute phase proteins in the monitoring of inflammatory disorders. Baillieres Clin Rheumatol 1994; 8: 531-552.
- Rafiq M, Worthington T, Tebbs SE, Treacy RB, Dias R, Lambert PA, Elliott TS. Serological detection of gram-positive bacterial infection around prostheses. J Bone Joint Surg Br 2000; 82: 1156-1161.
- Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. The Lancet 1993; 341: 515-518.
- Mitaka C. Clinical laboratory differentiation of infectious versus non-infectious systemic inflammatory response syndrome. Clin Chim Acta 2005; 351: 17-29.
- Arkader R, Troster EJ, Lopes MR, Junior RR, Carcillo JA, Leone C, Okay TS. Procalcitonin does discriminate between sepsis and systemic inflammatory response syndrome. Arch Dis Child 2006; 91: 117-120.
- Stucker F, Herrmann F, Graf JD, Michel JP, Krause KH, Gavazzi G. Procalcitonin and infection in elderly patients. J Am Geriatr Soc 2005; 53: 1392-1395.
- Selberg O, Hecker H, Martin M, Klos A, Bautsch W, Kohl J. Discrimination of sepsis and systemic inflammatory response syndrome by determination of circulating plasma concentrations of procalcitonin, protein complement 3a, and interleukin-6. Crit Care Med 2000; 28: 2793-2798.
- Di Filippo A, Lombardi A, Ognibene A, Messeri G, Tonelli F. Procalcitonin as an early marker of postoperative infectious complications. Minerva Chir 2002; 57: 59-62.
- Syed Ali, Andrew Christie, Andrew Chapel. The pattern of procalcitonin in primary total hip and knee arthroplasty and its implication in periprosthetic infection. J Clin Med Res 2009; 1: 90-94.
- Gendrel D, Bohuon C. Procalcitonin, a marker of bacterial infection. Infect 1997; 25: 133-134.
- Wirtz DC, Heller KD, Miltner O, Zilkens KW, Wolff JM. Interleukin-6: a potential inflammatory marker after total joint replacement. Int Orthop 2000; 24: 194-196.