ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2017) Volume 28, Issue 6
Transperitoneal laparoscopic adrenalectomy for a large pheochromocytoma: case report and review of the literature
1Department of Urology Surgery, Ningbo Urologic and Nephrotic Hospital, Qianhe Road, Ningbo, PR China
2Department of Ultrasound, Ningbo Urologic and Nephrotic Hospital, Qianhe Road, Ningbo, PR China
- *Corresponding Author:
- Guobin Weng
Department of Urology Surgery
Ningbo Urologic and Nephrotic Hospital, PR China
Accepted date: November 21, 2016
Background: Laparoscopic adrenalectomy is the standard procedure for the removal of adrenal masses. Transperitoneal laparoscopic resection of adrenal tumor is the preferred surgical technique. In the present case report authors described a case with a 20 cm right pheochromocytoma successfully treated by using transperitoneal laparoscopic approach.
Methods: A 26-year old man had a 20 cm retroperitoneal mass that was revealed by a contrast enhanced computed tomography and his preoperative blood epinephrine level was 421.41 pg/ml(normal range, <100 pg/ml). The patient was suspected to have a pheochromocytoma and received preoperative treatment with α-receptor blocker terazosin. A 20 cm retroperitoneal mass was successfully removed by transperitoneal laparoscopic approach.
Results: The operative time was 180 min and blood loss was 100 ml. No intraoperative or postoperative complications developed in the patient. Pheochromocytoma of right adrenal gland was confirmed by histopathology.
Conclusions: This case report suggests that adrenal tumor up to 20 cm in size may be treated by transperitoneal laparoscopic approach without complications. The experience and sufficient preoperative preparation are important for the success of the procedure.
Keywords
Pheochromocytoma, Laparoscopic adrenalectomy, Transperitoneal, Retroperitoneal mass
Background
Since the first laparoscopic resection of adrenal pheochromocytoma was reported in 1992, growing evidence has indicated that laparoscopic surgery for pheochromocytoma is feasible and safe [1-4]. Both the transperitoneal and retroperitoneal approaches have been reported for laparoscopic adrenalectomy [2]. The transperitoneal approach is preferred by most surgeons. However, mass larger than 5-7 cm is considered to be a contraindication for transperitoneal approach [5,6]. Laparoscopic excision of pheochromocytoma presents a challenge for surgeons. In the present case report authors present a patient with a 20 cm pheochromocytoma to demonstrate that adrenal pheochromocytoma up to 20 cm in size may be treated successfully by transperitoneal laparoscopic approach without complications.
Case Report
A 26-year old previously healthy man was referred to authors' hospital with a huge retroperitoneal mass revealedabdominal ultrasonography. He had a 1-month history of a huge retroperitoneal mass and was otherwise asymptomatic. Physical examination revealed an abdominal mass and rebound tenderness in the abdomen. Upon pressing the mass, the patient complained of palpitation and dizzy. His blood pressure was 145/91 mmHg, and resting heart rate was over a hundred beats per minute at admission. The blood tests and tumor marker levels (serum CA19-9 and CEA levels) were normal. There was no history of hematuresis, weight loss or bowel obstruction.
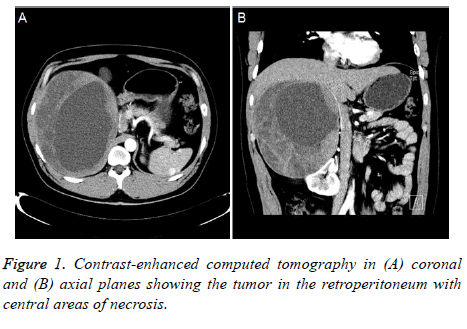
The patient’s preoperative blood epinephrine (E) and norepinephrine (NE) level was 421.41 pg/ml (normal range, <100 pg/ml) and 337.81 pg/ml (normal range, <600 pg/ml), respectively. A contrast enhanced computed tomography scan revealed a round-shaped mass that was about 20 cm in diameter with central areas of necrosis. The mass was in close proximity to and located between the liver and the right kidney. Furthermore, the mass was pressing and deforming the upper pole of the right kidney (Figure 1).
Preoperatively, the patient was suspected to have a pheochromocytoma and was treated by selective α-receptor blocker terazosin (2 mg, once a day for two weeks) to control hypertension and improve blood vessel capacity. The patient was offered to be treated by laparotomy or laparoscopic approach for pheochromocytoma. After careful preoperative hemodynamic optimization, the patient agreed to undergo transperitoneal laparoscopic approach.
Surgical procedure
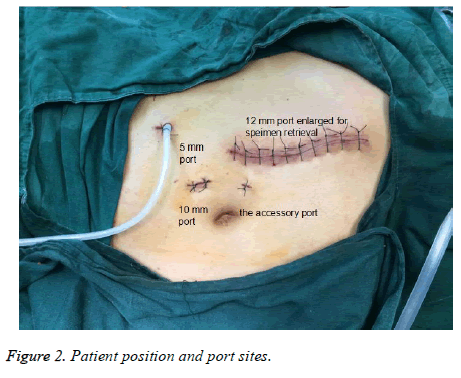
The procedure was performed with the patient in left lateral position. We employed four ports (Figure 2). A 1.0 cm skin incision was made lateral to the right of the umbilicus, and a 10 mm trocar was inserted to induce pneumoperitoneum. 12 mm and 5 mm trocars were then placed on the right mid-clavicular line under the costal arch and on the anterior axillary line above the iliac crest, respectively. The accessory port was positioned between the 12 mm trocars and the umbilicus. The dissection was initiated at the Gerota’s fascia. Subsequently, the large round-shaped mass was exposed, and the upper pole of the right kidney was pressed. With blunt dissection, right renal artery was freed between the right kidney and the tumor. The right renal artery gave off three branches. One of these branches was then followed caudally to the blood vessels that nourished the tumor, and was ligated and divided between clips. Next, careful dissection along inferior vena cava allowed the identification of right adrenal vein which was clipped and divided. As authors dissected this sheet, the tumor arising from the adrenal gland was identified. The adrenal gland and remaining attachments were cut with ultrasonic scalpel. The resected specimen was retrieved into an end pouch by 15 cm incision by extending the 12 mm port (Figure 2). A drainage was placed in the adrenal space.
Results
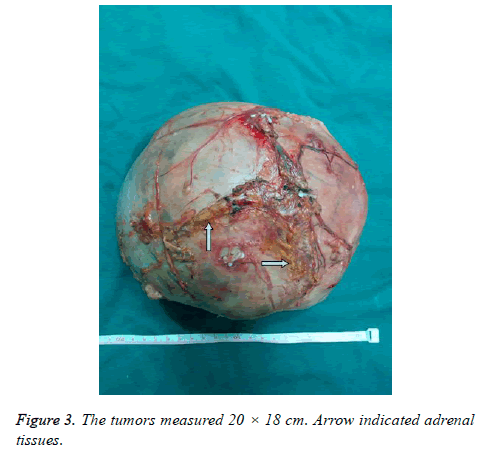
The mass measured 20 × 18 cm (Figure 3). The operative time was 180 min and blood loss was 100 ml. There were no intraoperative or postoperative complications. The patient started liquid diet on postoperative day 2 and remained asymptomatic with normal blood pressure. The patient was discharged on the 3rd of operation and the drainage tube was removed on postoperative day [7].
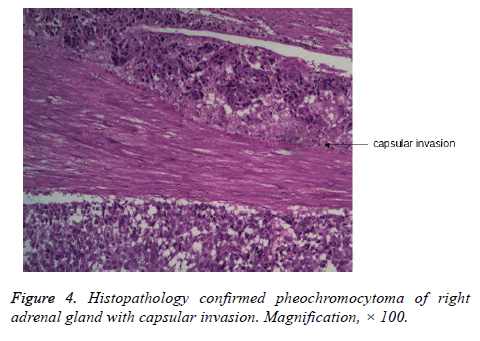
Histopathology confirmed pheochromocytoma of right adrenal gland with capsular invasion and malignant potential (Figure 4). Three months later, the patient’s preoperative blood epinephrine (E) and norepinephrine (NE) level was 84.96 pg/ml (normal range, <100 pg/ml) and 188.98 pg/ml (normal range, <600 pg/ml), respectively. The patient was doing well at follow-up.
Discussion
Laparoscopic adrenalectomy is the standard surgical treatment for the vast majority of adrenal tumors [7,8]. However, adrenal pheochromocytoma has been considered as a relative contraindication for the laparoscopic approach to adrenalectomy [8]. The reasons include potential hemodynamic instability with tachycardia, blood pressure fluctuations and low blood volume due to the stimulation of pheochromocytoma and pneumoperitoneum pressure. Therefore, intraoperative blood pressure and the risk of squeezing of the tumor present intractable problems for anesthesiologists and surgeons. Gill described laparoscopic surgery involving a milder stimulation technique compared to laparotomy [9]. Furthermore, the development of vasoactive drugs, the improvement of anesthetic technique and monitoring, and the application of laparoscopic surgery have dramatically improved postoperative management of patients undergoing surgical excision for pheochromocytoma. Several studies have shown that early ligation of the adrenal vein could lead to catecholamine-induced hypertensive crisis [10,11]. In this case, authors used selective α-receptor blocker terazosin to control arterial blood pressure and enlarge blood volume to normal prior to surgery. On the other hand, minimal manipulation and dissection of this large mass was performed prior to early ligation of adrenal vein during operation, Moreover, the procedure was smoothly manipulated by an experienced surgeon, and the patient showed stable fluctuations in blood pressure [12-20].
Surgical approaches for laparoscopic adrenalectomy include: anterior or lateral transperitoneal approach, and posterior or lateral retroperitoneal approach [20,21]. Published reports do not demonstrate whether one approach is superior to another. The choice of the surgical approach mainly depends on the operators’ experience and skill. Although anterior transperitoneal approach give more workplace and can reduce operation time as it does not need the change of position, authors prefer lateral transperitoneal approach because of the proper identification of anatomic landmarks and the convenience to perform the procedure. Compared to transperitoneal approach, posterior or lateral retroperitoneal approach can provide direct access to the adrenal gland without interfere with any abdominal organs. However, the lateral approach need longer learning curve and more time spent in patient positioning. Even the posterior retroperitoneal approach has been used for bilateral lesions. Additionally, disadvantages of this retroperitoneal approach are the narrow working space, which restricts the area for treating large tumors. For tumors with size exceeding 6 cm, transperitoneal approach is preferred by most surgeons, and contraindications for the transperitoneal approach include tumors bigger than 5-7 cm in size. However, a number of reports have been documented on successful transperitoneal laparoscopic adrenalectomy for tumors lager than 6 cm [12-16].
With increasing size of adrenal masses, transperitoneal laparoscopic adrenalectomy is expected to be more challenging and might be associated with increased risk of malignancy, intraoperative bleeding, and abdominal adhesions. Since the occurrence of large pheochromocytoma is rare, there are few reports on laparoscopic resection of pheochromocytomas lager than 10 cm. Is it safe and feasible to remove 20 cm pheochromocytoma using transperitoneal laparoscopic approach? Several factors are crucial to authors' success in performing this procedure in this case. First, by accurate preoperative localization of the pheochromocytoma based on abdominal ultrasonography, CT scan and magnetic resonance imaging, we found no vascular invasion, distant metastasis and local invasion. Furthermore, the patient’s clinical symptom was not obvious. These allowed us to select transperitoneal laparoscopic approach for the excision of this mass. Second, compared to open approach, transperitoneal laparoscopic approach provides excellent tumor location and better visualization during surgery. Third, emerging evidence suggests that there are no absolute contraindications for tumor size. Chaudhary et al. have successfully managed 11 cm pheochromocytoma by laparoscopic approach with minimal complications [17]. Kent et al. showed that laparoscopic resection of pheochromocytomas (at least 7 cm with the largest being 12.1 cm) was safely performed by experienced surgeons [7]. Fiszer et al. reported that an 18 cm adrenal tumor was successfully removed by laparoscopic approach [6]. Fourth, careful preoperative hemodynamic optimization and intraoperative hemodynamic stability are important for us to successfully accomplish this procedure.
Is authors' procedure considered minimally invasive with the 15cm incision required at the end of the procedure? In general, minimal handling and intraoperative morbidity support a minimally invasive approach for resecting a large pheochromocytoma compared to open approach. Furthermore, the incision can avoid tumor spillage which leads to peritoneal implantation with pheochromocytoma. On the other hand, open approach requires a larger incision (about 30 cm) for manipulation, and increases postoperative pain, abdominal adhesions, and incisional hernia. Consequently, our laparoscopic technique is in line with the principles of minimally invasive surgery.
Conclusion
In conclusion, this case report suggests that adrenal tumor up to 20 cm in size may be treated by transperitoneal laparoscopic adrenalectomy without complications. The experience and sufficient preoperative preparation are important for the success of the procedure.
Ethics Approval and Consent for Publication
Written informed consents were obtained from the patient for publication of his clinical and imaging data. A copy of the written consent is available for review by the Editor-in-Chief of this journal. The ethical review has been approved by our ethics committee.
Conflict of Interest
The authors have no conflict of interest or financial ties to disclose.
Author’s contributions
Xiangcheng Qin, Gang Wang and Aimei Lu contributed to the concept, study design and manuscript writing. Weizhi Zhu and Guobin Weng provided valuable comments. Kewen Zhouand Bin Zheng revises the manuscript. All authors read and approved the final manuscript.
References
- Carter YM, Mazeh H, Sippel RS, Chen H. Safety and feasibility of laparoscopic resection for large (≥ 6 CM) pheochromocytomas without suspected malignancy. Endocr Pract 2012; 18: 720-726.
- Beisa V, Klimovskij M, Simutis G, Sileikis A, Strupas K. Two-stage bilateral laparoscopic adrenalectomy for large pheochromocytomas. Videosurgery Miniinv 2014; 9: 110-114.
- Yadav K, Bakshi G, Prakash G, Tamhankar A, Verma K. Simultaneous bilateral laparoscopic adrenalectomy for pheochromocytoma in multiple endocrine neoplasia (MEN) syndrome: Case report with review literature. Int J Surg Case Rep 2014; 5: 487-490.
- Castilho LN, Simoes FA, Santos AM, Rodrigues TM, dos Santos Junior CA. Pheochromocytoma: a long-term follow-up of 24 patients undergoing laparoscopic adrenalectomy. Int Braz J Uro 2009; 35: 24-31.
- Lee CR, Walz MK, Park S, Park JH, Jeong JS, Lee SH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS. A comparative study of the transperitoneal and posterior retroperitoneal approaches for laparoscopic adrenalectomy for adrenal tumors. Ann Surg Oncol 2012; 19: 2629-2634.
- Fiszer P, Toutounchi S, Pogorzelski R, Krajewska E, Sutkowski B, Gierej P, Skórski M. Is tumor size a contraindication to laparoscopic adrenalectomy? Case report. Videosurgery Miniinv 2012; 7: 144-146.
- Kercher KW, Novitsky YW, Park A, Matthews BD, Litwin DE, Heniford BT. Laparoscopic curative resection of Pheochromocytomas. Ann Surg 2005; 241: 919-926.
- Humphrey R, Gray D, Pautler S, Davies W. Laparoscopic compared with open adrenalectomy for resection of pheochromocytoma: a review of 47 cases. Can J Surg 2008; 51: 276-280.
- Gill IS. The case for laparoscopic adrenalectomy. J Urol 2001; 166: 429-436.
- Rocha MF, Tauzin-Fin P, Vasconcelos PL, Ballanger P. Assessment of serum catecholamine concentrations in patients with pheochromocytoma undergoing videolaparoscopic adrenalectomy. Int Braz J Urol 2005; 31: 299-307.
- Flavio RM, Faramarzi RR, Tauzin FP, Vallee V, Leitao de Vasconcelos PR, Ballanger P. Laparoscopic surgery for pheochromocytoma. Eur Urol 2004; 45: 226-232.
- Agrusa A, Romano G, Frazzetta G, Chianetta D, Sorce V, Di Buono G, Gulotta G. Laparoscopic adrenalectomy for large adrenal masses: single team experience. Int J Surg 2014; 1: S72- S74.
- Dalvi AN, Thapar PM, Thapar VB, Rege SA, Deshpande AA. Laparoscopic adrenalectomy for large tumours: Single team experience. J Minim Access Surg 2012; 8: 125-128.
- Keinan A, Halfteck G, Reissman P. Laparoscopic adrenalectomy of large adrenal lesions. Harefuah 2014; 153: 727-730.
- Agha A, Iesalnieks I, Hornung M, Phillip W, Schreyer A, Jung M, Schlitt HJ. Laparoscopictrans-and retroperitoneal adrenal surgery for large tumors. J Minim Access Surg 2014; 10: 57-61.
- Mesci A, Celik O, Akand M, Aydogdu O, Arici G, Arici C, Erdogru T. Evaluation of laparoscopic transperitoneal adrenalectomy: is it feasible for large masses? Minerva Urol Nefrol 2015; 67: 175-178.
- Chaudhary R, Deshmukh A, Singh K, Biswas R. Laparoscopic resection of a large (11 cm) adrenal phaeochromocytoma. BMJ Case Rep 2011.
- Naya Y, Nagata M, Ichikawa T, Amakasu M, Omura M, Yamaguchi K, Ito H. Laparoscopic adrenalectomy: comparison of transperitoneal and retroperitoneal approaches. BJU Int 2002; 90: 199-204.
- Smith CD, Webber CJ, Amerson R. Laparoscopic adrenalectomy: new gold standard. World J Surg 1999; 23: 389-396.
- Hsu TH, Gill IS. Bilateral laparoscopic adrenalectomy: retroperitoneal and transperitoneal approaches. Urology 2002; 59:184-189.
- Bonjer HJ, Sorm V, Berends FJ, Kaziemer G, Steyerberg EW, de Herder WW. Endoscopic retroperitoneal adrenalectomy: lessons learned from 111 consecutive cases. Ann Surg 2000; 232: 769-803.