ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 2
Traumatic cranio-cervical distraction A case report.
1Department of Neurosurgery, “Gr T Popa” University of Medicine and Pharmacy Iasi, 16 Universitatii St., Iasi 700115, Romania
2Department of Neurosurgery,“N Oblu” Emergency Hospital Iasi, 2 Ateneului St. Iasi 700309, Romania
Accepted date: February 10 2014
A 33- year-old man was a victim of a high speed road traffic accident and he presented a traumatic upper cervical spinal cord injury. He was immobilized in a cervical collar, with tetraplegia and ventilatory assistance. Cervical CT scan showed an unstable dens fracture and distraction between the C1 and C2. Severe distractive hyperflexion or hyperextension accompanied by concurrent axial compression, which may be accompanied by associated rotation, appear to represent the injury mechanism. Dislocation of the cranio-cervical junction and atlanto-axial distraction are very serious injuries. The patient had an unfavorable evolution with death.
Keywords
atlanto-axial distraction, cervical spinal cord injury, tetraplegia
Introduction
A generally lethal trauma, craniocervical dislocation occurs due to osseoligamentous breakdown between the occiput – C1 and C2. Injury at the C1-C2 articulation may cause traumatic atlanto-axial distraction, leading to exaggerated motility around this joint. Neurologic deficits occur in 15%-20% of cervical fractures, and trauma to the atlanto-axial level is associated in 10% of cervical fractures [1,2]. Here, we present a uncommon case of complete craniocervical distraction.
Case Report
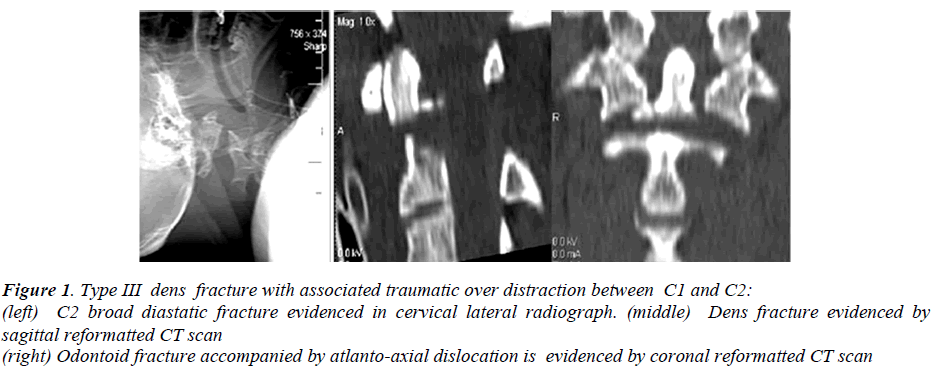
A male aged 33 involved in a high speed car crash suffered a traumatic brain injury and a cervical spine injury resulting in a traumatic coma with apnea (necessitating ventilator aid) and tetraplegia. The subject was immobilised with a cervical collar immediately after the collision; endotracheal intubation and ventilatory support were needed as a result of the respiratory failure. Additionally the patient presented with intermittent bradycardia. The type of cervical injury was established via spinal radiographs and spinal CT evaluation. The CT evaluation did not reveal any brain lesions. The patient suffered a complex atlanto-axial injury, comprising of an unstable type III dens fracture with the extending of the fracture to the superior face of C2 and distraction between the C1 and C2 (Fig.1). The treatment was ineffective and the patient died.
Figure 1: Type III dens fracture with associated traumatic over distraction between C1 and C2:
(left) C2 broad diastatic fracture evidenced in cervical lateral radiograph. (middle) Dens fracture evidenced by
sagittal reformatted CT scan
(right) Odontoid fracture accompanied by atlanto-axial dislocation is evidenced by coronal reformatted CT scan
Discussion
The articulations of the craniocervical junction are complex joints and ensure the craniocervical stability and the head movements. The integrity of the atlas and axis and their attaching ligaments determine the upper cervical biomechanical continuity. The most prevalent causes of upper cervical spine lesions are foremost car accidents, followed by falls and diving accidents. An associated head injury may present in these cases; additionally a cervical spine injury should be assumed in patients suffering serious polytrauma (including when associated with head injury). For children under 10 years old, upper cervical injuries manifest most often as injuries of the craniocervical junction [1-3].
The diagnosis and assessment of cervical fractures and luxations is possible via spinal computed tomography with sagittal and coronal reformatted images [3,4].
The injury mechanism for C1-C2 dislocation is commonly a severe hyperflexion accompanied of an axial compression, in some cases there are a hyperextension with axial compression and also a rotation movement can be associate. Dislocation of the cranio-cervical junction and atlanto-axial distraction is a very serious injuries. The ligamentous continuity is injured by the atlanto-axial articulation’s rotational and shearing forces; it is damaged by fractures near the attachments, avulsion etc. The characteristics of these distraction injuries are the loss of the C1-C2 continuity and the atlanto-axial separation [4-6].
A cervical collar must be used to promptly immobilize the victim following the accident. The injury may be evidenced by a cervical spine lateral radiography. An assessment of the fracture and luxation can be done via a computed tomography (CT) of the cervical spine. An assessment of the majority of potential upper cervical spine injuries can be done in a very sensitive manner via a CT scan.
The osseoligamentous lesions at the cranio-cervical junction and the spinal cord injuries can be found via magnetic resonance imaging (MRI) of the cervical spine. Maintaining spinal integrity as well as the potential spinal cord lesions must be prime factors in the planning of all examinations.
Swift treatment of concerned patients is imperatively dependent on a fast diagnosis of this injury. Trauma patients’ early care must comprise as a first concern the cervical spine injuries’ diagnosis and stabilization.
Satisfactory ventilatory as well as cardiovascular supports are the next steps in patient management subsequent to the cervical injury diagnosis.
Then the production of cervical radiographs should follow the immobilization of the cervical spine in a neutral position. The requisite stability can be achieved via halo immobilization, as cervical collar immobilization does not restrain atlanto-axial movement. Surgery will consist of odontoid screw fixation with a high union rate, of 80% - 100%, and it may retain atlanto-axial movements. Posterior C1-C2 arthrodesis has a high union rate as well, however the fusion sacrifices atlanto-axial movement [3,4,7]. Upper cervical injuries and traumatic craniocervical dislocations are not very rare entity, but the complete craniocervical distraction is uncommon and the report shows this extreme situation of traumatic craniocervical dislocations with very serious consequences because of the very high complete spinal cord transection [8].
References
- Crook TB, Eynon CA. Traumatic atlantoaxial rotator subluxation. Emerg Med J 2005; 22: 671-672.
- Cooper Z, Gross JA, Lacey JM, Traven N, Mirza SK, Arbabi S. Identifying survivors with traumatic craniocervical dissociation: a retrospective study. J Surg Res 2010; 160: 3-8.
- Fuentes S, Bouillot P, Palombi O, Ducolombier A, Desgeorges M. Traumatic atlantoaxial rotatory dislocation with odontoid fracture: case report and review. Spine 2001; 26: 830-834
- Violas P, Ropars M, Doumbouya N, Bracq H. Case reports: Atlantooccipital and atlantoaxial traumatic dislocation in a child who survived. Clin Orthop Relat Res 2006; 446: 286-290.
- Howard JJ, Duplessis SJ. Posterolateral dislocation of the C1-C2 articulation associated with fracture of the anterior arch of C1: a case report. Spine 2001; 29: E562-564.
- Payer M, Wetzel S, Kelekis A, Jenny B. Traumatic vertical atlantoaxial dislocation. J Clin Neurosci 2005; 12: 704-706.
- Vilela MD, Bransford RJ, Bellabarba C, Ellenbogen RG. Horizontal C-1 fractures in association with unstable distraction injuries of the craniocervical junction. J Neurosurg Spine 2011; 15: 182-186.
- Martínez-Lage JF, Alarcón F, Alfaro R, Gilabert A, Reyes SB, Almagro MJ, López López-Guerrero A. Severe spinal cord injury in craniocervical dislocation. Case-based update. Childs Nerv Syst 2013; 29:187-94.